Research Article - (2022) Volume 17, Issue 1
Received: 15-Mar-2022, Manuscript No. gpmp-22-57307; Editor assigned: 18-Mar-2022, Pre QC No. P-57307; Reviewed: 21-Mar-2022, QC No. Q-57307; Revised: 24-Mar-2022, Manuscript No. R-57307; Published: 29-Mar-2022
Caesarean hysterectomy (CH) is a standard treatment for placenta accreta spectrum (PAS) but it sometimes causes bladder/ureter injury. We attempted to test whether ureter dissection reduces the incidence of bladder/ureter injury at CH for PAS.
Methods: Patients with CH for PAS (n=140) was divided into two groups: ureter dissection (+) vs. (-). We compared the perinatal and surgical outcomes between the two groups.
Results: Two groups showed the same background characters: parity, frequency of previous miscarriages, or indication for hysterectomies. No significant differences in outcomes were observed between the two groups: operative time, perioperative blood loss, drop of hemoglobin, number of transfused RBC/plasma, or hospital-stay length. The following morbidities did not differ between the two groups: bladder/ureter/bowel injury, wound complications, ICU admission, and maternal mortality.
Conclusion: Ureteric dissection did not reduce bladder/ureter injury in CH for PAS.
Ureteric dissection; Uterine artery clamping; Caesarean hysterectomy; Morbidly adherent placenta.
Placenta accreta spectrum (PAS), refers to a spectrum of abnormal pathological adherence of the placenta, including placenta increta, placenta accreta, and placenta percreta. PAS is associated with a major morbidity still the main risk is the massive obstetric hemorrhage, which leads to secondary complications including coagulopathy, multi-system organ failure, and death. However, maternal morbidity and mortality is reduced when care is provided in centers of excellence (COE), the main step in these centers is a directed care plan and multidisciplinary team including all concerned specialties, and surgical expertise capable of managing the full spectrum of accrete complexity [1].
Caesarean hysterectomy is the gold standard treatment for PAS - however, conservative treatment may be considered in young needing future pregnancy provided there is close follow-up and monitoring - There are many complications for caesarean hysterectomy one of them leads to increase operative time, prolonged postoperative recovery, and sepsis: is urological injury which is mainly bladder injury. In a systematic review of surgical techniques used for placenta accreta, the overall rate urinary tract injury at peripartum hysterectomy was 29%, most of them involving the urinary bladder 78%, whereas 17% involve the ureter [1].
Modification of surgical approaches reduced urinary tract injuries compared with standard hysterectomy [1]. reducing the risk of urinary tract injury during caesarean hysterectomy Intraoperative measures like proper surgical technique, gentle and proper exposure of structures, blind clamping of the blood vessels is forbidden, dissection with routinely ureteric direct visualization, The careful dissection and mobilization of the bladder, extreme cautious during use of the electrocautery [2], a mandatory step to prevent injury to the ureter is to proper identification during its path through the pelvic inlet and the regions where it is more susceptible to be injured [3].
The aim of the current prospective study is to compare between two different techniques of caesarean hysterectomy for placenta accreta spectrum the first performing caesarean hysterectomy with the classical approach without ureteric dissection and the second with ureteric dissection and visualization before uterine artery clamping.
This cohort prospective study was carried out in Ain Shams University Maternity Hospital, Cairo, Egypt during the period starting from October 2018 till Oct 2020. The Ethical Committee of The Faculty of Medicine Ain-Shams University approved the study.
The present prospective cohort study assessed the safety and efficacy of early ureteric visualization in decreasing the incidence of urologic injuries in caesarean hysterectomy for placenta accreta in comparison with the standard approach. The study included patients with abnormally invasive placenta diagnosed and confirmed and revised by senior sonographer and repeated caesarean section and excluded morbidly obese patient (BMI over 35). Severely anemic patients (Hb less than 8 mg/dl), previous ureteric injury or previous uro-gynecological surgery and patients with bleeding disorders.
One hundred and sixty patients were diagnosed as placenta accreta, they were enrolled to the study, twenty of them were excluded from the study, and eighteen of them were managed conservatively so hysterectomy was not done, while the remaining two had thrombocytopenia. The remaining 140 cases were equally divided into two groups Group A cesarean hysterectomy was done using the classical approach while, Group B consisted cesarean hysterectomy with ureteric dissection before uterine artery clamping.
Study population
The pregnant females were recruited form women attending labor ward to undergo cesarean section for placenta accreta and ended with cesarean hysterectomy. They have been diagnosed by 2D and power Doppler. Sonographic evaluation was done and confirmed by senior sonographer in our accreta team. Patients were divided randomly into two groups as follows:
Group A: patients with elective caesarean section for placenta accrete ended with caesarean hysterectomy and caesarean hysterectomy was performed with the classic approach.
Group B: patients with elective caesarean section for placenta accrete ended with caesarean hysterectomy and caesarean hysterectomy was performed with ureteric dissection.
The two groups were carefully studied as regards to incidence of urologic injuries, the intraoperative timing, time needed for dissection and complications.
Methodology and surgical intervention
After taking informed written consent about possible complications, all women recruited in the study were subjected to:
Data collection:Careful history taking; antenatal history included demographic details.
Maternal age and BMI
Obstetric history:Gravidity, parity and gestational age, risk factors for placenta accreta: antepartum hemorrhage, previous dilatation and curettage, myomectomy septic miscarriage, detecting also inclusion and exclusion criteria.
I. Thorough clinical assessment:
a) General examination: For vital colors and vital signsArterial blood pressure, pulse, temperature, anemia, jaundice.
b) An abdominal examination: Assessment of fundal level, uterine contractions, uterine tenderness, fetal lie, fetal viability.
II. Investigations:
a) Blood group and Rh type. b) Full blood count. c) Coagulation profile. d) Comprehensive metabolic panel (serum creatinine, ALT, AST, RBS). e) Abdominal ultrasound and color Doppler U/S (gestational age, placental location, placental grading, criteria of invasion, fetal viability, fetal lie, fetal count, liquor amount and turbidity). f) 4 units of packed RBCs already cross-matched and available fresh frozen plasma.
III. Surgical intervention:
All patients done by the same surgical team
In group A: The standard approach for caesarean hysterectomy (dissection or visualization is not performed). Midline abdominal incision, Hysterotomy: classic midline incision of the uterus [above upper margin of the placenta], delivery of the fetus in presence of a well-trained neonatology team. Avoid traction of the placenta, no ecbolics given, and quick closure of the uterus [leaving placenta in situ] in one layer. Clamping and cutting the round ligament, clamping and cutting the ovarian ligament with preservation of the ovaries, Lateral dissection of the uterus from the pelvic side wall, followed by very careful sharp bladder dissection. Finally clamping of the uterine vessels is done below the level of the placenta with or without complete removal of the cervix depending on degree of placental adherence. Closure of the uterine stump is performed, repair of urological injuries if present, internal artery ligation if needed followed by careful hemostasis, then closure of the abdomen is performed after leaving two wide bore drains.
In group B: As in group A but with ureteric dissection. Careful dissection of the posterior leaflet of the broad ligament until the ureter is properly visualized, careful dissection and exposure of both ureters and proper identification of the iliac vessels so as to facilitate the ligation of anterior division of internal iliac artery if needed and to avoid any major vascular injury. Following ureteric dissection is performed lateral dissection of the uterus is completed from the pelvic side wall, followed by very careful sharp bladder dissection below level of the cervix. Finally clamping of the uterine vessels is done and continue as in group A.
Assessment of blood loss in both groups by counting towels, every single soaked towel 150 cc, suction machine set at the end of operation by anesthesia team to guard against bias and (NB) liquor volume subtracted from suction machine just before uterine incision till frank blood in the field.
Statistical methods
Data were analyzed using IBM© SPSS© Statistics version 23 (IBM© Corp., Armonk, NY). Continuous numerical variables were presented as mean and SD and inter-group differences were compared using the unpaired t test. Discrete variables were presented as median and interquartile range and between-group differences were compared using the Mann-Whitney test. Categorical variables were presented as number and percentage and differences were compared using Fisher’s exact test. Ordinal data were compared using the Chi-squared test for trend. Two-sided P-values <0.05 were considered statistically significant.
160 patients were planned to be recruited, 80 patients for each group, during the on-going research 20 were excluded 18 of them due to placental separation and other two due to bleeding tendency before surgery as shown in Fig. 1., So percentage of placental delivery 11.25 and the rest of patients under went hysterectomy
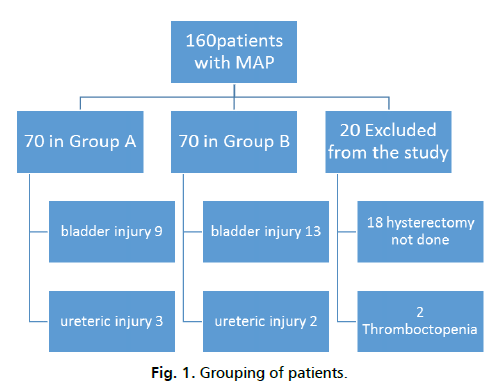
Fig 1. Grouping of patients.
Tab. 1. Shows the demographic characteristics, parity & previous miscarriages in both groups, Tab. 2. shows the perioperative data in both groups, while Tab. 3. Postoperative drop in hemoglobin and volume of blood in drain in both study groups.
| Variables | Group A (n=70) | Group B (n=70) | P-value* |
|---|---|---|---|
| Age (Years) | 33.0 ± 4.8 | 32.4 ± 6.2 | 0.523 |
| BMI (kg/m2) | 30.0 ± 3.1 | 29.6 ± 2.9 | 0.485 |
| GA (Weeks) Parity (n & %) | 35.4 ± 2.2 | 35.3 ± 2.3 | 0.831 |
| P1cs 2 (2.9%) | 2 (2.9%) | 0.124 | |
| P2cs 9 (12.9%) | 10 (14.3%) | - | |
| P3cs 27 (38.6%) | 30 (42.9%) | - | |
| P4cs 20 (28.6%) | 24 (34.3%) | - | |
| P5cs 6 (8.6%) | 3 (4.3%) | - | |
| P6cs 4 (5.7%) | 1 (1.4%) | - | |
| P7cs 2 (2.9%) | 0 (0.0%) | - | |
| Frequency of previous miscarriages (n & %) | Nil 45 (64.3%) | 41 (58.3%) | 0.943 |
| One 14 (20%) | 18 (25.7%) | - | |
| Two 4 (5.7%) | 6 (8.6%) | - | |
| Three 2 (2.9%) | 2 (2.9%) | - | |
| Four 4 (5.7%) | 1 (1.4%) | - | |
| Five 1 (1.4%) | 2 (2.9%) | - |
Tab. 1. Demographic characteristics, parity & previous miscarriages of both study groups.
| Variables | Group A (n=70) | Group B (n=70) | P-value* |
|---|---|---|---|
| Operative time (h) | 2.7 ± 0.7 | 2.7 ± 0.6 | 0.944† |
| Operative blood loss (ml) | 2,200 (2,000 to 3,000) | 2,500 (2,000 to 3,000) | 0.467 |
| Number of packed RBC units | 2 (2 to 4) | 2 (2 to 4) | 0.526 |
| Number of plasma units | 1 (1 to 2) | 1 (1 to 4) | 0.706 |
Tab. 2. Perioperative data in both study groups.
| Variables | Group A (n=70) | Group B (n=70) | P- value* |
|---|---|---|---|
| Drop in hemoglobin (g/dl) | 1.5 (1.0 to 2.0) | 2.0 (1.0 to 2.0) | 0.030 |
| Volume of blood in drain (ml) | 500 (400 to 600) | 500 (300 to 600) | 0.492 |
| Hospital length of stay (days) | 5 (3 to 9) | 4 (3 to 6) | 0.303 |
Tab. 3. Postoperative drop in hemoglobin and volume of blood in drain in both study groups.
The number of cases of placenta accreta were 22 (31.4%) in group A vs. 14 (20%) in group B, while placenta previa accreta were 47(67.1%) in group A vs. 51 (72.9%) in group B, and the number of cases of placenta percreta were 1 (1.4%) in group A vs. 5 (7.1%) in group B (P value = 0.106) using Fischer exact test.
Blood products transfusion in both groups 1- Packed RBCS :10 patients received one unit, 69 patients received two units, 5 patients received three units, 22 patients received four units, One patient received five units, 4 patients received six unit, 29 patients received more than six units 2-FFP: 11 patients didn’t receive plasma transfusion 56 patients received one unit 27 patients received two units, 2 patients received three unit 8 patients received four units, 26 patient received more than four units detail of both groups in Tab. 4.
| Number of packed RBCs Transfused | Standard Approach | Ureteric Visualization |
|---|---|---|
| One unit | 4 | 6 |
| Two unit | 35 | 34 |
| Three unit | 2 | 3 |
| Four units | 12 | 13 |
| Five units | 1 | 1 |
| six units | 4 | 3 |
| more than six units | 9 | 8 |
Tab. 4. Pattern in packed RBCS transfusion in both groups.
As regards complications we had 9 (12.9%) cases of bladder injury in group A vs. 13 (18.6%) in group B (P=0.487), ureteric injuries were 3 (4.3%) in group A vs. 2 (2.9%) in group B (P= 1.000), Types of genitourinary injuries Bladder: all of them sharp injury to the dome by scissors during dissection of the bladder way from lower uterine segment prior to clamping the uterine arteries, Ureteric injuries: in group A one of them was inadvertent ligation during uterine artery clamping and other two after uterine artery clamping there still bleeding and need to secure uterine pedicle in which accidental ligation of the ureter were discovered and ureteric sharp injury occurred during removal of the ligature. all primary repair by urology team with stenting. In group b the two ureteric injuries happened during control of bleeding from lateral pelvic wall the clamping and accidental ligation of ureter at level not visualized which were sharply injured during removal of the stitch (which was encompassing the ureters) and repaired by suturing and stenting, bowel injury 1 (1.4%) in both groups (P= 1.000), wound complications 23 (32.9%) in group A vs. 18 (25.7%) in group B (P=0.458), ICU admission 9 (12.9%) in group A vs. 12 (17.1%) in group B (P = 0.637), and maternal mortality 1 (1.4%) in group A vs. zero (0.0%) in group B (P = 1.000) using Fischer exact test.
In planned caesarean hysterectomy most patients had total hysterectomy due to involvement of cervix by morbid adherent placenta and Internal iliac artery ligation were 14 in group A and in group 9 B, and was done to control massive pelvic hemorrhage (not done routinely) and following analysis for subgroup with internal iliac ligation in both groups (details in urological injuries in Tab. 5-7.), as shown in Tab. 8. in patient who no urological injuries no significant difference between the two groups as regard operative time and blood loss.
| Urological Injures | Standard Approach |
Ureteric Visualization | P-value | |
|---|---|---|---|---|
| Injured | 4 | 4 | 0.65 | ns |
| Not injured | 10 | 5 | ||
Tab. 5. Comparison between both groups in urological injures in patient with internal iliac artery ligation Fisher’s exact test-Bladder injury.
| Urological Injures | Standard Approach |
Ureteric Visualization | P-value | |
|---|---|---|---|---|
| Injured | 1 | 0 | 1.0 | ns |
| Not injured | 13 | 9 | ||
Tab. 6. Comparison between both groups in urological injures in patient with internal iliac artery ligation Fisher’s exact test- Ureteric injury.
| Variables | Standard | Ureteric Visualization | P-value* | |
|---|---|---|---|---|
| Operative time (hr) | 3 ± 0.33 | 3.1 ± 0.52 | 0.52 | ns |
| Perioperative blood loss (ml) | 2750 (2375-3625) | 2750 (2300-3625) | 0.97 | ns |
Tab. 7. Comparison between both groups in operative time in patient with internal iliac artery ligation Data are mean ± standard deviation or median (interquartile rang).
| Variables | Standard | Ureteric Visualization | P-value* |
|---|---|---|---|
| Operative time (h) | 2.6 ± 0.59 | 2.6 ± 0.52 | 0.70† |
| Operative blood loss (ml) | 2,000 (2,000 to 3,000) | 2,400 (2,00 to 3,000) | 0.31 |
Tab. 8. Comparison between two groups non genitourinary injury as regard operative time and operative blood loss.
The current study showed that there was no significant difference between the two groups as regards demographic characteristics, previous deliveries, previous miscarriages, indications for hysterectomies, perioperative data (operative time, perioperative blood loss, number of packed RBCs and plasma units transferred), length of hospital stay, volume of blood loss in drains, drop in hemoglobin level and complications as wound complications, ICU admissions, bowel injury, bladder injury and ureteric injury although the latter complication was more in the group which didn't have ureteric dissection (group A) which may point out to the importance of meticulous ureteric identification taking into account that one of the two injuries in the ureteric dissection group (group B) was unavoidable as the case was placenta percreta invading both the bladder and the ureter. Glimour, et al. [4] did a literature review and agreed with the current study in suggesting that the most effective method for prevention of urological injuries is proper intraoperative identification of both the bladder and the ureters, especially that Jauniaux, et al. [5] in their systemic review found that the overall rate of urinary tract injuries in peripartum hysterectomies performed for placenta accreta was 29%, which is higher than the rate of 4.8% found for hysterectomies performed for gynecological indications [6]; therefore, modifications in the surgical technique may contribute in reducing the risk of such injuries, particularly in those with risk factors associated with ureteric injury as previous pelvic surgery, pelvic adhesions, obesity, large pelvic masses and intraoperative bleeding [7]. The urgency in dealing with the latter complication leaves the surgeon little time to dissect the bladder from the uterus. Late discovery is also one of the problems of ureteric injuries as Jacob, et al. [7] found in their study that 70% of cases were diagnosed after discharge, 50% of cases had a complicated course and 45% had unfavorable legal outcomes suggesting intraoperative ureteral identification in high-risk cases.
Other methods of ureter identification include pre-operative ureteric stenting, which has the advantage of avoiding denervation and devascularization associated with extensive ureterolysis [8]; however, this approach may not be feasible in some cases of placenta percreta particularly if both the bladder and the ureter are invaded as the case found in group B. The current study has the advantages of being done in a tertiary dedicated center and recruiting relatively large number of cases in relation to the frequency of such condition; however, its main limitation is the lack of proper randomization.
Ureteric dissection before cesarean hysterectomy for placenta accreta spectrun didn’t show merit. It was not associated with statistically significant difference as compared to classical hysterectomy in decreasing the risk of intraoperative urological injuries Usually we just expose the ureter ensuring its safety before uterine artery clamping in some cases we had to dissect it in ureteric canal for selective ligation of uterine artery, in severe pelvic hemorrhage in morbid adherent placenta with urge of surgeon to control it blind clamping of uterine artery compromise the ureter so visualization of the ureter ensures its safety so no need to ureter dissection. Further randomized controlled trials are needed to support or refute such finding.
M. Khallaf: Designed the study, shared in data collection & analysis, revision & drafting of manuscript. The rest of the authors: Shared in data collection & analysis, revision & drafting of the manuscript.
Authors report that they neither have conflict of interest nor received financial support for this work.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.