Review Article - (2023) Volume 18, Issue 2
Received: 05-May-2023, Manuscript No. GPMP-23-97520; Editor assigned: 08-May-2023, Pre QC No. P-97520; Reviewed: 19-May-2023, QC No. Q-97520; Revised: 06-Jun-2023, Manuscript No. R-97520; Published: 30-Jun-2023
Modern hysteroscopy has become the main diagnostic and therapeutic tool for the majority of endometrial pathologies and for managing women with fertility issues. Historical data reveals evidence of endoscopic procedures in gynecologic cases dating back over 4,500 years, long before the concept of hysteroscopy was developed. In 1869, Pantaleoni performed the first successful diagnostic and operative hysteroscopy on a menopausal woman suffering from postmenopausal bleeding due to an endometrial polyp. Since then, many advancements have been made in instrumentation, distension media and applications of hysteroscopy. Office hysteroscopy is the latest trend in this field, offering the advantage of "see and treat" without the need for preoperative analgesia or anaesthesia. This review focuses on the history and evolution of hysteroscopy as an endoscopic method, presenting all milestones chronologically. Important background information is provided on the limitations at the time, the concepts upon which researchers based their refinements, and the first-ever applications of any technological improvements. Year by year, the hysteroscope underwent reforms until it became the inseparable diagnostic and operative tool for gynaecologic endoscopists that we know today.
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
Haberler
History; Diagnostic hysteroscopy; Evolution; Endoscopy; Pantaleoni; Bozzini; Hamou; Bettocchi
Endoscopy as a "philosophy"
In the field of medicine, progress is often driven by the imagination of pioneers and the dedication of subsequent researchers. Endoscopy, as a medical philosophy, rests on the belief that the most effective way to diagnose and treat diseases is through direct visualisation. This idea has been present throughout the history of medicine, as physicians and researchers have sought to explore the human body's cavities through natural orifices.
However, endoscopy is more than just a product of technological advancement and new equipment. The earliest endoscopists recognised the value of direct visualisation of the human body, even in the absence of advanced technological tools. In fact, the concept of minimal invasiveness, a central pillar of medical science, has been present since the earliest days of medicine. Until the middle of the 19th century, surgeons rarely performed operations, instead relying on indirect approaches to treating disease.
Endoscopy is rightfully a novel, philosophical approach to surgery and it would be important to be able to break down any limited and/or outdated concept that makes endoscopy a product of technological advances and of novel equipment. It is a fact that the first endoscopists insisted on the value of direct visualisation of the human body with a naked eye, despite their limited know-how and lack of technological means. Minimal invasiveness is a pillar of medical science and, it is worth noting that until the middle of the 19th century, surgeons only indirectly approached any disease and rarely reached a decision to perform an operation [1,2].
Origins of endoscopy: Antiquity
Since ancient times, the study of the human body has been a subject of fascination for scientists and scholars. In the 5th century BC, students of hippocrates, the father of medicine, were influenced by the anatomy of animals and began studying the human body. "Benefit or no harm" was taught first the axiom of the minimal invasive approach by Hippocrates, indicating the importance of avoiding invasive methods [3]. Hippocrates himself emphasised the importance of minimal invasiveness, cautioning against invasive methods that could cause inflammation and subsequent death.
The first references regarding the study of the human body are attributed to the students of hippocrates in 5th century BC, who were influenced by the anatomy of animals. In addition, Aristotle managed, through his physiognomic works, to create designs that approached the anatomy of mammals. During the hellenistic period, alexandria became a cultural centre where the study of human anatomy and physiology flourished. Herophilus identified the fallopian tubes, while rufus recognised the shape of the uterus as a "cup-shaped vessel" [4]. Soranos the Ephesian, known as the father of obstetrics and gynaecology, identified the ovaries. Galen, who laid the foundations for the study of human anatomy and physiology, maintained his view of the subdivided womb, influenced by his study of monkeys.
During the middle ages, efforts to study the human body were banned, except in Salerno, Sicily [5]. It was not until the Renaissance that scientists once again turned their attention to the study of the human body. Mondino dei Luzzi wrote a book on the female reproductive system, presenting it in a manner similar to modern understanding [6]. Leonardo da Vinci depicted the ovaries, fallopian tubes, and corresponding ligaments in his drawings. Berengario da Carpi, Vesalius, and their students proposed that the uterus consisted of a single cavity, a theory that was supported by endoscopic methods [7].
The first reports of endoscopic techniques can be traced back to hippocrates from Kos, who described a primitive ortho scope, which he called a "mirror," in his work "on the Articulations." Similar endoscopes were discovered in the ruins of ancient Pompeii. An Egyptian seal stone depicts a patient in a position similar to that used in ortho sigmoidoscopic examinations. The Talmud, a Jewish religious text dating back to 200 BC, describes a lead drainage tube inserted into the vagina, possibly indicating a primitive attempt at hysteroscopy. Abu-al-Qasim, an Arab physician who lived from 936-1013 AD, used a mirror to shed light on the vaginal canal during gynaecologic examinations. He is considered one of the world's "Fathers of Surgery" and his discoveries have been used in Europe and Asia for over 500 years [8].
The rise of hysteroscopy during 19th century
Centuries went by, reaching 1805, when the German Philip Bozzini built the first endoscope, a discovery that was once considered a "toy" by his contemporaries (Fig. 1.). Unfortunately, the Vienna Medical Academy suspended all of Bozzini's research while the pioneering physician, a victim of scientific competition, died of typhoid fever at the age of 35. As for the first successful diagnostic and therapeutic hysteroscopy, it was performed several years later, in 1869, by Pantaleoni.
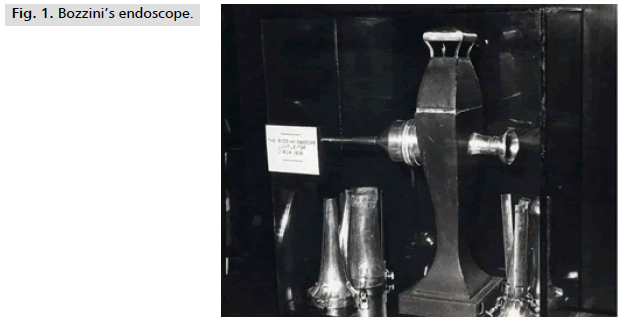
Figure 1: Bozzini’s endoscope.
Hysteroscopy was particularly innovative in the early 19th century and attracted the interest of more researchers in the following years. The improvement of hysteroscopic equipment offered patients better diagnosis and treatment. Important researchers worth mentioning were: Desormeaux, who designed the first truly functional cystoscope in 1853 and Cruise, who 12 years later in Dublin modified the first endoscope using a small-volume oil lamp and dissolved camphor as a light source [9].
It was not until 1869 that Pantaleoni, a student of Cruise, performed the first hysteroscopy on a woman with post-menopausal bleeding. Pantaleoni’s hysteroscopy has been successful both in diagnostic and operative level. He managed to recognise endometrial polyps and to use silver nitrate during hysteroscopy for cauterisation of the endometrial pathology. That made him, rightfully, the first surgeon to achieve both diagnostic and operative hysteroscopy [10].
The Viennese urologist Nitze, managed successfully to get the necessary lighting of the bladder, which was an important milestone of modern hysteroscopy, in 1879 (Fig. 2.) [11]. In particular, Nitze applied to his "Incandescent platinum loop" cystoscope, a lighting source, which was cooled with liquid. Technically, cystoscopy was easier than hysteroscopy, since demanded lower pressure and there was less possibility of bleeding, when the endoscope was in contact with bladder’s wall [12].
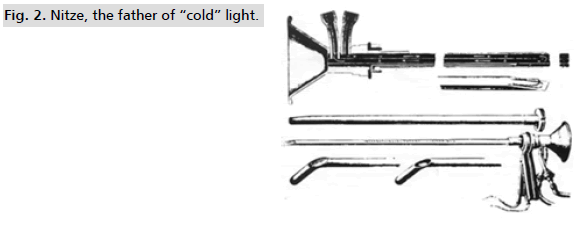
Figure 2: Nitze, the father of “cold” light.
In 1898, the first scientific record of hysteroscopic findings is made by S. Duplay and S. Clado, according to references in the historical book of Evangelos Kalliontzis, "Operative Surgery". The book contained 28 designs of the intrauterine cavity, it described the hysteroscopic equipment and the technique (Fig. 3.). Spiro Clado, who turned out to be a Greek from Smyrna, designed his own hysteroscope which was called "Endohysteroscope", around 1886 [13].
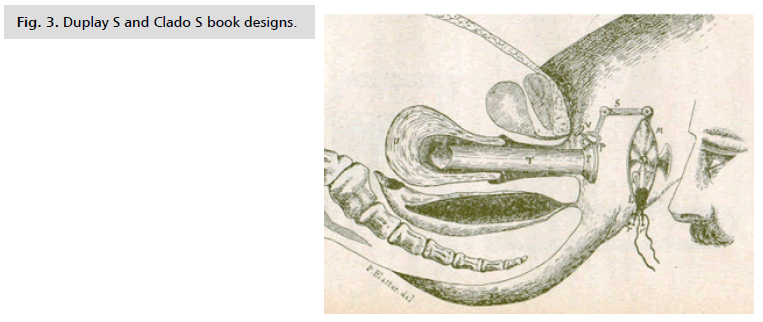
Figure 3: Duplay S and Clado S book designs.
Researchers as Blondel (France), Morris (America) and Bumm (Germany), tried to present their ideas about hysteroscopy, but they mainly reported their experience of uterine bleeding after attempting endoscopic evaluation of human cavities (uterus, bladder). Twenty more years were needed in order to improve Nitze’s hysteroscope: In 1914, Alred Heineberg of Philadelphia introduced an improved version of this hysteroscope, adding a hot-dip liquid supply channel that allowed a continuous flow of liquid distension medium with an additional output channel [14]. For this reason, Heineberg’s "mitroscope" (the word mitro comes from the greek word mitra, which means uterus) can be considered the first continuous flow hysteroscope [15].
The next key point in the development of hysteroscopy, is the choice of carbon dioxide as a uterine distension medium, as the use of gas achieves excellent distension of the endometrial cavity [16]. Gas medium is still in use today, rarely though, since most hysteroscopists nowadays prefer normal saline as optimal distension medium. This innovation was introduced in 1925 by Isidor Clinton Rubin. The first hysteroscope with adjacent functional channel was developed by Mikulicz-Radecki and Freund in 1927, which allowed endometrial biopsy along with direct visualisation of the endometrium [17]. A few years later, Gauss used normal saline in order to distend the intrauterine cavity, while determining the ideal pressures to achieve perfect visibility and safety for the patient herself. Gauss also introduced the first hysteroscopic images. In 1934 Schroeder added the optimal pressure measurements, with regards to liquid distension medium. According to him pressures of 25-30 mm Hg were satisfactory for achieving adequate visualization [18]. Schroeder also set the threshold of 55 mm Hg upon which possible fluid diffusion into the peritoneal cavity was warranted [19]. The hysteroscope was initially used to diagnose endometrial polyps, submucous fibroids, and to determine the phase of the menstrual cycle. In 1936, second designed the hysteroscope with a liquid supply system and fixed optical fibres [20]. Direct visualization of the endocervix was performed in 1942 by Palmer during hysteroscopy, and he proposed this procedure as the standard of care to be achieved in all hysteroscopies [21]. Contact hysteroscopes were created later on in 1947 by Norment, who placed the light source at the proximal end of the hysteroscope [22].
Hysteroscopy in the 20th century
The progress of hysteroscopy in the second half of the 20th century was characterised by the introduction of new means for uterine distension and the introduction of operative hysteroscopy [23]. In 1962, Silander used a hysteroscope with two channels (internal observation channel and external irrigation channel). The distal end of the hysteroscope had a light bulb and a thin balloon. By alternating the pressure of the balloon, the additional opportunity to examine the endometrial cavity in great detail was offered. A fiber optic cable was incorporated into the hysteroscope only in 1965. The illumination was performed using cold xenon light and the light source was placed outside the body of the hysteroscope [24].
Since 1980, hysteroscopy has been established as the standard procedure for the diagnosis and treatment of endometrial and endocervical pathology [25]. New hysteroscopic equipment was developed. Today, "office" hysteroscopy is performed in the clinic, without the use of anaesthesia or analgesia. Operative hysteroscopic procedures continued to be developed and widely performed [26]. The available types of hysteroscopes are rigid or flexible. Hysteroscopes are available in different diameters with different viewing angles. The rigid hysteroscope with a diameter of 2.9 mm, an angle of 30°C and an outer sheath of 5 mm is used widely in gynaecologic procedures. The first flexible hysteroscope was made by Mohri in 1971. These hysteroscopes have fibre optics, with diameters from 3.1 mm to 3.7 mm, and are used for diagnostic hysteroscopy. Versascope semi-flexible mini fibre hysteroscopes (Gynecare, Ethicon) have a 1.8 mm of 0°C angle and a 3.2 mm outer sheath. These hysteroscopes are used for diagnostic and operative procedures and provide the option of using mechanical tools such as scissors and forceps and 5 Fr bipolar electrodes for excision, haemostasis, and cauterization [27].
Since 1970, more distension media started to be used. Edstrom used 32% dextrose (MW 70,000 Daltons) as a distension medium during hysteroscopy [28]. Later on, a number of different media have been used successfully to distend the endometrial cavity. In particular, Lindemann used carbon dioxide, Menken used a high molecular weight polyvinylpyrrolidone solution, while Sugimoto used isotonic NaCl and Quinones-Guerrero used dextrose solution 5% [29].
It was not until 1980, that Hamou, the father of modern hysteroscopy, introduced microcolpohysteroscopy (Fig. 4.) [30]. His idea of reducing the diameter of hysteroscopes was a crucial step in the development of hysteroscopy and its evolution. From 1980 onwards, the technique is improved by the addition of a video camera with a surveillance screen. The surgeon's position became more comfortable, permitting wider hysteroscopic movements. In addition, a monopolar electrothermal system was introduced that allowed endometrial septum excision, polypectomy as well as excision of small diameter submucous fibroids. Nevertheless, the technique was still problematic, with the hysteroscopic equipment being large in diameter [31].
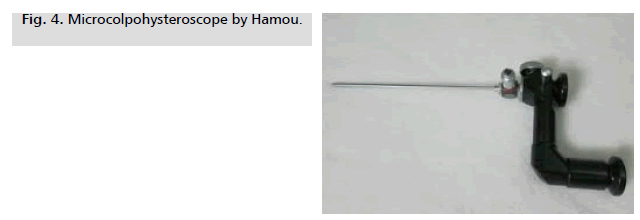
Figure 4: Microcolpohysteroscope by Hamou.
Hysteroscopic surgeries were made possible and continuously improved by the use of different means of distension and the development of new instruments. Female sterilization was performed by Menken in 1971 [32]. Lindemann and Quinones-Guerrero successfully performed transcervical catheterization of the fallopian tubes using operative hysteroscopy in 1972. In 1974, Edstrom used the biopsy forceps for intrauterine symphysiolysis and also used the same type of equipment to perform metroplasty, in case of a uterine septum. The first successful attempt in resecting a submucous fibroid has been performed by Neuwirth and Amin in 1976. An electrode was used for hysteroscopic myomectomy by Hanning et al. 1980. Finally, hysteroscopic laser ablation of the endometrium was performed by Goldrath et al. In 1981 [33].
The Charge Coupled Device (CCD), publicly known as "chip", was developed in 1982 consisting of a small endocamera and a sensor, which introduced video assisted endoscopy [34]. The High Definition (HD) camera was developed few years later. de Cherny and his colleagues used an electrotome, only in 1986, to excise a uterine septum. Hysteroscopic myomectomy using an Nd: YAG laser was performed by Baggish in 1989, while Choe performed the first hysteroscopic resection of a septum of the uterus with a Nd: YAG [35].
Introducing office hysteroscopy
In 1996, Bettocchi developed the first operative "office" hysteroscope, which was used at an outpatient facility (Fig. 5.). The hysteroscope can be inserted into the uterus without dilating the cervix and allows the procedure to be performed in an outpatient setting. The Bettocchi office hysteroscope with a 2 mm diameter endoscope, single flow and 3.6 mm outer sheath is used for diagnostic hysteroscopy. Also, the Bettocchi Integrated Office Hysteroscope (B.I.O.H.) with a diameter of 4 mm provided the advantage of performing both diagnostic and operative office hysteroscopies [36].
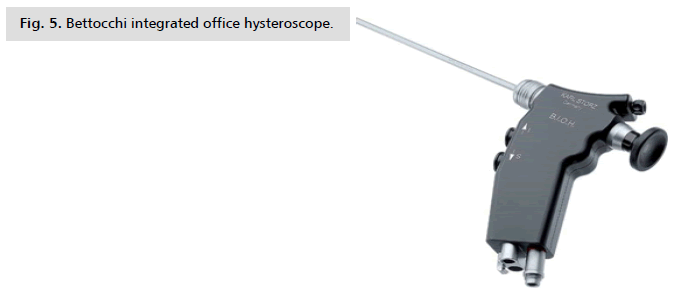
Figure 5: Bettocchi integrated office hysteroscope.
Further technologic improvements led to the development of the operative electrotomy, which uses monopolar energy. An electrode is used for surgery and consists of an endoscope ranging from 2-4 mm, an angle of 12°C, two sheaths with irrigation and suction channels and a functional part that carries haemostasis and/or cauterization electrodes. The electrode is connected to a high frequency electrosurgical unit. When high frequency monopolar energy is used for operative hysteroscopy, the distension medium should not contain electrolytes (i.e 4% sorbitol-mannitol, 1.5% glycine, 5% glucose) [37]. This limitation was surpassed by the construction of bipolar electrotomy by various manufacturers, including Karl Storz (Tuttingen, Germany), and the bipolar electrotomy olympus corporation (Tokyo, Japan) and the resectoscope of Richard Wolf Medical Instruments Corporation (Vernon Hill, USA). Bipolar electrotomy allows hysteroscopic resection of submucous fibroids, resection of uterine septa, removal of endometrial polyps, and endometrial biopsies. This electrotome allows the use of low viscosity mediums containing electrolytes, such as 0.9% NaCl and Ringer's lactate, which reduces the risk of hyponatremia and fluid overload syndrome [38-40].
Advances in the field of electrosurgical technology have allowed the introduction and use of electrosurgical systems such as the Gynecare Versapoint (Ethicon) bipolar electrosurgical system. A high frequency electrosurgical generator and a bipolar electrotomy are provided by the system. The m odern A utocon 400 high-frequency electrosurgical unit (Karl Storz) can operate in both monopolar and bipolar mode. An upgraded electrosurgical unit, the Olympus UES-40 SurgMaster generator, was also developed providing monopolar and bipolar energy, which makes it possible to use the bipolar electrotomy even when the distension medium is normal saline.
Operative hysteroscopy progresses and is widely used in the beginning of the 21st century. Using bipolar energy, laser energy and various instruments, hysteroscopy is a safe method to perform a wide variety of procedures with minimal complications. Endometrial morcellation is the newest approach to operative hysteroscopy that removes endometrial lesions under direct visualization with continuous dissection and removal of tissue fragments in real time. Hysteroscopic morcellators were manufactured to reduce surgical time as well as to maintain and increase a high level of technical safety. The US Food and Drug Administration (FDA) in 2005 approved the use of the first hysteroscopic morcellator "TRUCLEAR" (Smith and Nephew, Andover, MA). This morcellator is 9 mm in diameter and has a rotating blade, which allows the fibroid and polypoid tissue to be removed from the endometrial cavity.
FDA approval was also given to "MyoSure tissue removal system" (Hologic, Bedford, MA) in 2009, another type of morcellator, which had a diameter of 6.25 mm and a blade that could rotate and oscillate. This hysteroscope provides the option of removal of submucous fibroids up to 3 cm in diameter. A mechanical hysteroscopic morcellator called Intrauterine Bigatti Shaver (IBS) made by Bigatti (Karl Storz, Germany) is also available.
Moving on to the future of Hysteroscopy
Hysteroscopy continues to play an important role in gynecologic practice today, with ongoing developments in technology and techniques. The use of smaller, more flexible hysteroscopes has made hysteroscopy less invasive and more comfortable for patients. The availability of high-definition cameras and advanced imaging software has improved visualization and accuracy during hysteroscopic procedures. In addition, new methods for uterine distension and tissue removal, such as mechanical morcellation and bipolar electrosurgery, have expanded the range of procedures that can be performed hysteroscopically. The introduction of "office" hysteroscopy has made the procedure more accessible and convenient for patients, as it can be performed in the clinic without the need for anaesthesia or hospitalization. With ongoing advancements in hysteroscopic technology and techniques, it is likely that hysteroscopy will continue to play an important role in the diagnosis and treatment of gynaecologic pathology in the future.
Over the last 30 years, hysteroscopy became the first line investigation of the diagnosis and treatment of endometrial pathology. The main milestones in hysteroscopic equipment are summarised in Tab. 1. Milestones in the history of hysteroscopy.
| Year | Researcher | Innovation |
|---|---|---|
| 1805 | Bozzini | Construction of endoscope |
| 1869 | Commander Pantaleoni | First successful diagnostic and operative hysteroscopy |
| 1879 | Nitze | Father of “cold” light |
| 1898 | S. Duplay and S. Clado | First book on hysteroscopy |
| 1925 | Isidor Clinton Rubin | CO2 as a uterine distension medium |
| C. Schroeder | Definition of endometrial pressures | |
| 1971 | R. Porto | Insufflator |
| 1971 | H.J. Lindemann | Insufflator |
| 1980 | J. Hamou | Father of modern hysteroscopy |
| 1981 | F.A. Chervenak | Monopolar electrode |
| 1983 | Α DeCherney | Endometrial ablation |
| 1987 | J.P. Hallez | Electrode for gynaecologic procedures |
| 1996 | Bettocchi | Office hysteroscopy |
| 2005 | Bigatti-STORZ, Smith andNephew, Hologic | Hysteroscopic morcellator FDA approved |
Tab. 1. Milestones in the history of hysteroscopy.
Hysteroscopy is a method, simple, safe, and universally accepted by patients. The future of hysteroscopy due to the rapid technological innovations can be hardly defined with certainty and accuracy. However, the rich history and heritage of the technique makes it certain, that its progress in improving women's medical care is inevitable.
All pictures presented were retrieved by Google images which are available for every user. The author team would like to thank Ms Banu Godfri who acted as native English-speaking editor of the final form of the manuscript. Her support is highly appreciated.
All authors declare no conflict of interest.
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
[Crossref] [Google Scholar] [PubMed]
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.