Research - (2023) Volume 18, Issue 3
The grading of uterine endometriosis by MRI findings
Zahraa Abdulhussein Katea* and Kassim Amir Hadi Taj Al-DeanReceived: 04-Sep-2023, Manuscript No. gpmp-23-113511; Editor assigned: 05-Sep-2023, Pre QC No. P-113511; Reviewed: 16-Sep-2023, QC No. Q-113511; Revised: 22-Sep-2023, Manuscript No. R-113511; Published: 29-Sep-2023
Abstract
Background: Endometriosis is the presence of the endometrium outside the uterine cavity accompanies by chronic inflammation or deep pelvic infiltrating affect premenopausal women. Magnetic resonance imaging (MRI) plays an important role in the detection of endometriosis.
Aim: The study aimed to observe the patterns of endometriosis By MRI, to estimate the MRI grades of endometriosis and to achieve the planning of a management approach.
Methods: A prospective study of total of 55 women with history of chronic abdominal pain or menstrual disturbances or pelvic pain were diagnosed as a case of endometriosis enrolled at a period from August 2022 to April 2023 at Department of Radiology, Al-Hillah General Teaching Hospital. Data collected including age, and symptoms. MRI findings include: location of lesion, stage, present of implantation, number of implantation, present of cystation, site, and present of adhesion. MRI (Philips N.V.2021 MRI unit 1.5 Tesla, SRN: 32534) was done for all women in supine position.
Results: The most common reported age group was between (25-35 years) with mean age was (32.22 ± 6.01 years). Regarding MRI findings of endometriosis, the most location of lesion was observed at anterior of pelvis (41.8%). Endometriosis stage III in (60.0%) is common. The severity is mainly moderate in (58.2%). The majority of implantation of endometriosis was seen in deep layer (78.2%). The majority of endometriosis observed with large cystation in (85.5%). Both ovaries involved in most of cases (78.2%). Thes inter-observer agreement Kappa (k) statistic revealed that diagnosis of endometriosis by MRI have better agreement (k= 0.835) than US (k= 0.378) with significant difference.
Conclusion: Younger age women are the most commonly detection with endometriosis. The common MRI findings of endometriosis include anterior segment lesion, stage III, moderately severe, deep seated, large cystic, bilateral and densely adhesion. Statistically, the diagnosis of endometriosis by MRI had better agreement than US.
Keywords
Endometriosis; Premenopausal women; MRI; Infertility
Introduction
Endometriosis is an enigmatic disease; however, there was long history of work of basic sciences and clinical aspects. Firstly, Sampson published his initial article in 1927, suggesting that retro-grade menstruation is the reason of peritoneal endometriosis [1]. Globally, the prevalence in women varies wide: 0.7% to 11% in visitors to health care centers, 2% to 22% in the surgical sterilization, 17% to 47% in infertility and 2% to 74% in female with chronic pelvic pain [2]. In Iraq, several studies detected endometriosis in younger age group. Naji and co-workers reported the mean age of 31.16 ± 5.61 years [3]. The prevalence rate in Iraqi women is range between 15 - 33% [3-5].
Shorter menstrual cycles, flow longer than usual, heavier flow, and low parity are the etiological factors for endometriosis [1].
In term of pathogenesis, researchers thought that implantation theories, coelomic metaplasia theories, and embryonic Mullerian rests are the major aspect of development of endometriosis [6]. Women complained of pelvic pain, dysmenorrhea, dyspareunia and infertility [7]. Early diagnosis and evaluation of the spreading and severity of adhesions, prior and post management are important for formulating strategies of treatment [8]. Three main entities of endometriosis are ovarian endometriotic cysts, superficial peritoneal and Deep Infiltrating Endometriosis (DIE) [9].
MRI plays important roles in the ovarian endometriotic cysts and DIE detection. Also, it is helpful for diagnosing characteristic features of illnesses associated with ovarian endometriotic cysts: pregnancy decidual changes, hormonal treatment sequel and endometriosis-related tumors [8-12]. Additionally, it assist gynecologists in evaluating the precise locations of the endometriosis and adhesions severity, which are clinically strongest issue in the management [8].
The study aimed to observe the patterns of endometriosis By MRI, to estimate the MRI grades of endometriosis and to achieve the planning of a management approach.
Methods
Study design and setting
A prospective study of total of 55 women with history of chronic abdominal pain or menstrual disturbances or pelvic pain were diagnosed as a case of endometriosis enrolled at a period from August 2022 to April 2023 at Department of Radiology, Al-Hillah General Teaching Hospital.
Data collection
Data collected including age, and symptoms. MRI findings include: location of lesion, stage, present of implantation, number of implantation, present of cystation, site, and present of adhesion.
Inclusion criteria
- Age above 18 years (women with child bearing age).
- Clinical features suggestive of endometriosis (chronic pain, dyspareunia, dysmenorrhea, and infertility).
- Endometriotic lesions detected by gynecological or surgical examination.
- Endometriotic lesions in US.
Exclusion criteria
- Any contraindication for MRI examination (pregnancy, pacemaker, shells, golden or plutonium denture or fixation and allergy to contrast).
- Women unwilling to do the MRI.
- Malignancy.
MRI protocols
MRI (Philips N.V.2021 MRI unit 1.5 Tesla, SRN: 32534) was done for all women in supine position. The following sequences were performed; T2WI sagittal and axial. T1WI sagittal and axial. Transverse images and SPAIR (with and without fat –suppression). An intravenous gadolinium chelates (with a dose of 0.1 mmol/kg) was injected. Lesion of interest scanned using the (b) values: zero, 500, 1000 and 1500 s/mm2. MRI protocol performed in the current study are:
- T2 sagittal: TR= 3000 ms, TE= 90 ms, FOV= 290 × 290 mm, Matrix= 208 × 205, Thickness= 4 mm
- T2 axial: 3700 ms, 100 ms, 288 × 350 mm, 292 × 180, 5 mm
- T1 axial: 500 ms, 10 ms, 260 × 216 mm, 263 × 171, 5 mm
Also, we used MRI deep Pelvic Endometriosis Index (dPEI) classification to categorized lesion according to laterality.
Statistical analysis
Statistical package for social science (SPSS version 24.0, Chicago: SPSS, Inc., USA) was used. Results were described in the form of frequencies and percentage for qualitative data and mean ± SD to describe quantitative data. Inter-observer agreement was assessed via weighted-kappa statistic (k). A one-sided P value of 0.05 or less was considered statistically significant.
Results
The most commonly reported age group was between (25-35 years) as (35, 63.64%). The mean age was (32.22 ± 6.01 years). About 15(27.27%) women aged between 36-45 years (Table 1).
In term of symptoms, 8(14.55%) pain, 13(23.64%) dysmenorrhea, 3(5.45%) dyspareunia and 6(10.91%) infertility. Out of 55, 25(45.45%) women complained from all symptoms mentioned (Tab. 1.).
| Variables | No. | % | |
|---|---|---|---|
| Age (years) Mean ± SD (Median)= 32.22 ± 6.01 (31) |
<25 | 4 | 7.27 |
| 25-35 | 35 | 63.64 | |
| 36-45 | 15 | 27.27 | |
| >45 | 1 | 1.82 | |
| Symptoms | Chronic pelvic pain | 8 | 14.55 |
| Dysmenorrhea | 13 | 23.64 | |
| Dyspareunia | 3 | 5.45 | |
| Infertility | 6 | 10.91 | |
| All | 25 | 45.45 | |
Tab. 1. Patients of the study.
Regarding MRI findings of endometriosis, the most location of lesion was observed at anterior aspect of pelvis (23, 41.8%). Posterior and lateral endometriosis seen in 13(23.6%) of cases for each. Only one case detected in colorectal region. Five cases were situated in different sites. In relation to stages of endometriosis, stage I reported in 4(7.3%), II in 11(20.0%), III in 33(60.0%) and IV in 7(12.7%). The severity of endometriosis visualized as minimal in 5(9.1%), mild in 15(27.3%), moderate in 32(58.2%) and severe in 3(5.5%). The majority of implantation of endometriosis was seen in deep layer (43, 78.2%) whereas superficial reported in 12(21.8%) of cases. Most of implantation number distribution of endometriosis as more in (49, 89.1%) whereas few number reported in 6(10.9%) of cases. Regarding cystation, the majority of endometriosis observed with large cystation in (47, 85.5%) whereas small type was documented in 8(14.5%) of cases. One ovary involved by endometriosis was visualized in (12, 21.8% cases) whereas both ovaries involved in most of cases (43, 78.2%). There was no adhesion seen in 12(21.8%) of women. The majority of endometriosis cases were adhered with dense layer (37, 67.3%) whereas firmly adhesion seen in 6(10.9%) of cases (Tab. 2.).
| Findings | No. | % | |
|---|---|---|---|
| Location | Posterior | 13 | 23.6 |
| Anterior | 23 | 41.8 | |
| Lateral | 13 | 23.6 | |
| Colorectal | 1 | 1.8 | |
| Multi-sites | 5 | 9.1 | |
| Stages | I (1-5) | 4 | 7.3 |
| II (6-15) | 11 | 20.0 | |
| III (16-40) | 33 | 60.0 | |
| IV (>40) | 7 | 12.7 | |
| Severity | Minimal | 5 | 9.1 |
| Mild | 15 | 27.3 | |
| Moderate | 32 | 58.2 | |
| Severe | 3 | 5.5 | |
| Implantation | Superficial | 12 | 21.8 |
| Deep | 43 | 78.2 | |
| Implantation number | Few | 6 | 10.9 |
| More | 49 | 89.1 | |
| Cystation | Small | 8 | 14.5 |
| Large | 47 | 85.5 | |
| Cyst site | One | 12 | 21.8 |
| Both | 43 | 78.2 | |
| Adhesions | No | 12 | 21.8 |
| Filmy | 6 | 10.9 | |
| Dense | 37 | 67.3 | |
Tab. 2. MRI findings of endometriosis in this study.
MRI findings of endometriosis classified according to deep pelvic endometriosis index (dPEI) into (Fig. 1.): Right lateral which further subdivided into antero in (4, 7.3%), medio in (39, 70.9%) and postero in (12, 21.9%). Left lateral which further subdivided into all site in (9, 16.4%), medial in (37, 67.3%) and posterior in (9, 16.4%). Central which further subdivided into antero in (8, 14.5%), medio in (9, 16.4%) and postero in (38, 69.1%).
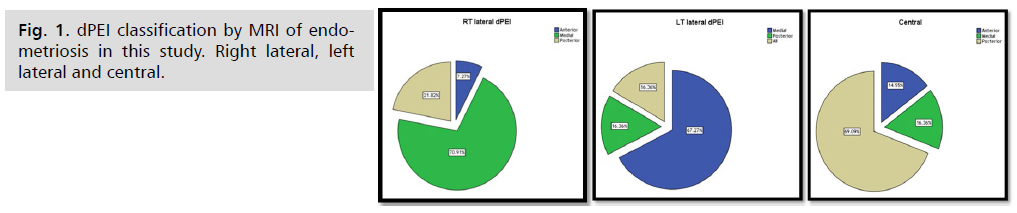
Fig. 1. dPEI classification by MRI of endometriosis in this study. Right lateral, left lateral and central.
These inter-observer agreement Kappa (k) statistic of MRI findings vs. US findings revealed that diagnosis of endometriosis by MRI had better agreement (k= 0.835) than US (k= 0.378) with significant difference (Tab. 3.).
| Radiology | *Kappa value | 95%CI | p-value |
|---|---|---|---|
| MRI | 0.835 | 0.769-1.000 | 0.012 |
| US | 0.378 | 0.235-0.676 |
fair 0.21-0.40, moderate 0.41-0.60 , substantial 0.61-0.80, #perfect 0.81-1.0
Tab. 3. Kappa value in this study.
Discussion
The endometriosis is one of common gynecological problems among the productive age of women [13-16].
In the present study, the most commonly age group was (25-35 years) in (63.64%) with mean age (32.22 ± 6.01 years). Our age mean similar to means of age of Thomassin-Naggara, et al. [15] (34.5 ± 4.45 years), and Bazot, et al. [13] (33.7 ± 6.55 years). These are much lower than mean age of Bader and Taj-Aldean [16], in Al-Hilla city, the mean age was 42.14 ± 7.78 years. Previous studies reported a mean age more than (50 years) [17, 18]. The reasons in these different in mean ages of the patient are because the development of diagnosis modalities, early detection and raising the awareness about the problem such as MRI -DWI based upon measuring water molecules by the random Brownian motion within a tissue voxel. The restriction in water movement indicating the abnormal cell member and pathological tissue cellularity [19,20], and in general, pathological lesions are associate with restricted diffusion, because of raise the cellularity [21]. Adenomyosis and endometriosis are demonstrating regions of low-signal intensities on T2-WI [19].
In the current study, the symptoms of endometriosis as (14.55%) pain, (23.64%) dysmenorrhea, (5.45%) dyspareunia, (10.91%) infertility and (45.45%) of women complained from all symptoms mentioned. Thomassin-Naggara, et al. [15] reported different percentages in 150 women with endometriosis as chronic pelvic pain (95%), dysmenorrhea (91%), dyspareunia (76%), infertility (31%), catamenial diarrhea (26%), rectal bleeding (7%), bladder disorders (20%) and abnormal uterine bleeding (11%).
Regarding MRI findings of endometriosis, the most location was observed at anterior aspect of pelvis (41.8%). Posterior and lateral endometriosis seen in (23.6%) of cases for each. Only one case detected in colorectal region. Dislike with Thomassin-Naggara, et al. [15] they described endometriomas (33%), posterior (98%), anterior (24%) and lateral (52), colorectal endometriosis (34.6%) and multiple lesions (11.3%). These may be attributed to different in sample size, and population studied [15].
In Iran, Nouri, et al. [22] conducted a cross-sectional study on 433 patients with endometriosis, their mean age of 34.18 ± 7.99 years. They found the predictive value of MRI strongest than the values of clinical symptoms. They concluded that there are no suitable and accurate non-invasive methods for detecting endometriosis. MRI, clinical examination and symptoms alone are not helpful for definitive diagnosis and suggested to shift to biomarkers and artificial intelligence methods.
In Egypt, Abdelghany and colleagues conducted a prospective study on 23 women with endometriosis at 2021, their mean age of (32.1 ± 5.8 years). They recorded the symptoms of patients as pelvic pain (95.7%), VB (56%), infertility (69.5%), dysmenorrhea (78.3%) and dysuria (91.3%) [23], which greater than our percentage. The endometriosis clinical features are varying; but the most common are chronic pelvic pain and infertility [24].
As results, the endometriosis is common in younger age women group which is agree with Abo-Gamra, et al. [25] and disagree with Jramillo Cardoso, et al. [26].
In relation to stages of endometriosis, stage I reported (7.3%), II (20.0%), III (60.0%) and IV (12.7%). A disagreement with Bazot, et al. [13] reported that stages 0, I, II, III, IV and V were observed in (3%), (21%), (5%), (3%), (39%) and (29%) patients, respectively because they studied a large number of preoperative MRI of 751 women.
The severity of endometriosis in this study visualized as minimal (9.1%), mild (27.3%), moderate (58.2%) and severe (5.5%). The majority of implantation of endometriosis was seen in deep layer (78.2%) whereas superficial in (21.8%) of cases. Thomassin-Naggara, et al. [15] disagree with our findings, they recorded 45.3% of the patients had mild DE (<2 compartments), 30% patients with moderate DE (3 or 4 compartments) and 24.7% with severe DE (>5 compartments).
In the present study, most of implantation number distributed more in (89.1%) whereas few number reported in (10.9%) of cases. The majority observed with large cystation in (85.5%) whereas small type was documented in (14.5%). One ovary involved by endometriosis was visualized in (21.8% cases) whereas both ovaries (bilateral) involved in most of cases (78.2%). Dislike with Abdelghany, et al. [23] which found that unilateral ovarian involvement was the most common site.
The study of Thomassin-Naggara, et al. [15], lateral pelvic was present in 20.6%, 82.2% and 97.2% of patients in the mild, moderate and severe groups, respectively. Moreover, bilateral DE was present in 22.2% and 81.1% of the patients with moderate and severe DE, respectively.
There was no adhesion seen in (21.8%) of women. The majority of endometriosis cases were adhered with dense layer (67.3%) whereas firmly adhesion seen in (10.9%) of cases. Similarly with a meta-analysis de Resende, et al. [27].
In this study, MRI findings of endometriosis classified according to deep pelvic endometriosis index (dPEI) into: Right lateral which further subdivided into antero (7.3%), medio (70.9%) and postero (21.9%). Left lateral which further subdivided into all site (16.4%), medial (67.3%) and posterior (16.4%). Central which further subdivided into antero (14.5%), medio (16.4%) and postero (69.1%). This is in line with a previous study of Zilberman, et al. [28] while the preoperative MRI of Thomassin-Naggara, et al. [15] revealed lateral locations in 76% and vaginal locations in 52.6%. Lateral endometriosis is not a rare finding, is prevalence of around 15% [29,30].
In past decades, MRI descriptions focused on posterior and anterior compartment locations of endometriosis [31]. However, the first MRI report of lateral endometriosis was published in 2012 with the description of parametrial involvement [29]. In 2019, Poupon and co-authors published a nomogram predicting the complication risk using the Enzian classification by differentiating three groups of patients with endometriosis [32].
The sensitivity and specificity of preoperative MRI for predicting moderate or severe endometriosis was 0.84, and 0.81, respectively, with an overall accuracy of 0.83 [15].
Bazot, et al. [29] showed a very good accuracy of MRI compared to surgical findings in parametrial endometriosis with a highly experienced radiologist. They reported a sensitivity (83.3%), specificity (98.6%) and accuracy (96.4%).
In the meta-analysis of Nisenblat, et al. [33] found that MRI cannot be systematically acquired as a triage test to diagnose endometriosis but it is recommended preoperatively by various guidelines as [8,12,34] as preoperative counseling and the strategy of surgery relied on accurate mapping of DE.
Bader and Taj-Aldean [16] used additional imaging tools for separating these adenomyosis from fibroids. They established a significant difference in the ADC values among fibroid and adenomyosis. The adenomyosis mean ADC was (0.75 × 10-3 mm2/s) and fibroid mean ADC was (0.63 × 10-3 mm2/s). They used three b factors of (0, 400, and 600 s/mm) of a 1.5 T scanner. The three b values method may be accurate because it minimized the effect of perfusion effect [16].
Kilickesmez, et al. [35] and Erdem, et al. [36] reported that DWI for adenomyosis and leiomyomas is very significantly not only for pathologies but also for normal myometrium.
Alborzi, et al. [37] compared between ultrasound and MRI of 555 women with rectal endometriosis. They documented sensitivity, specificity, accuracy, PPV, NPV, PLR and NLR were, respectively, 69.55%, 91.30%, 70.4%, 11.48%, 99.46%, 8.0 and 0.3 compared to 51.37%, 79.17%, 52.53%, 6.64%, 98.26%, 2.47 and 0.6 for MRI.
Mabrouk, et al. [30] and Alborzi, et al. [37] found that transvaginal ultrasound (TVS) is accurate in the detection of superficial endometriosis than deep lesion. Furthermore, both MRI and US had same sensitivity, specificity and accuracy in the detection of DE. However, based on 1360 patients referred to a tertiary center who examined by TVUS, lateral endometriosis was incidentally discovered on surgery in 31.2% of cases [30].
Alborzi, et al. [37] concluded TVS should be used as a first-line modality for detection of rectal endometriosis, due to greater availability, better accuracy and cheap.
The results of the present study revealed that DE was prevalent in our sample; therefore, the Kappa (k) statistic of MRI findings vs. US findings revealed that diagnosis of endometriosis by MRI had better agreement (k= 0.835) than US (k= 0.378) with significant difference, (p= 0.012). This is in consistent with inter-reader agreement Thomassin-Naggara, et al. [15] report an excellent kappa (0.88).
The UBESS represent the only ultrasound classification assigning stages depend on the anticipated levels of the complexity of the surgical procedures [38], which classified as I, II and III, that correlating with three levels of surgical complexity according to the RCOG [39]. Moreover, the rASRM classification of MRI is the most widely used classification for evaluating pelvic endometriosis [40].
TVS is considered the first line endometriosis imaging modality because of its availability and cheap. However, MRI is superior to TVS in detection and characterization of lesions because it is better resolute of soft tissues, low operator dependence and capability to imaging a large volume of the pelvis and consequently information of surgery planning [41].
Thomassin-Naggara and co-authors reported that the accuracy of MRI in detection of endometriosis was 97.3% for the senior radiologist and 96.7% for the junior radiologist [15]. Because of differences in imaging sequences and system, therefore, the reader should exercise caution and a need for standardization of protocols to allow for reproducibility among imaging sites and vendors [16].
Abdelghany, et al. [23] showed that most of the cases attained high signal intensity in T1WI (p=0.009) and low signal intensity in T2WI (p=0.029) which are significant in the detection of endometriosis, while DWI (p= 0.218) and ADC (p= 0.162) have no significant value. They concluded that MRI has a high role in detection of endometriosis and complete evaluation of different pelvic compartments. These are similar to our observations in Figs. 2-7.
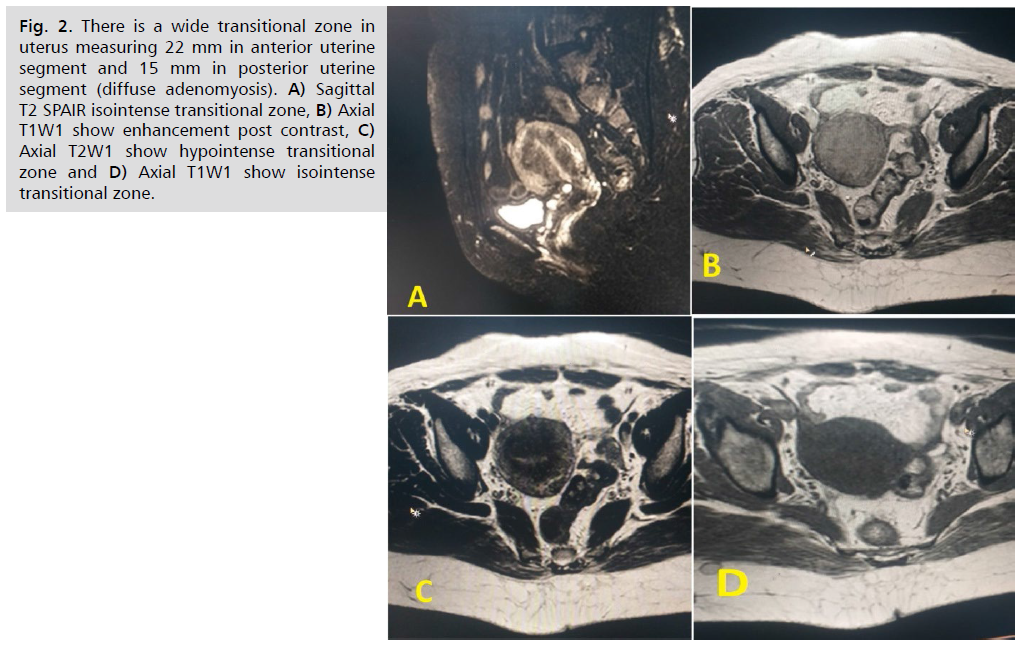
Fig. 2. There is a wide transitional zone in uterus measuring 22 mm in anterior uterine segment and 15 mm in posterior uterine segment (diffuse adenomyosis). A) Sagittal T2 SPAIR isointense transitional zone, B) Axial T1W1 show enhancement post contrast, C) Axial T2W1 show hypointense transitional zone and D) Axial T1W1 show isointense transitional zone.
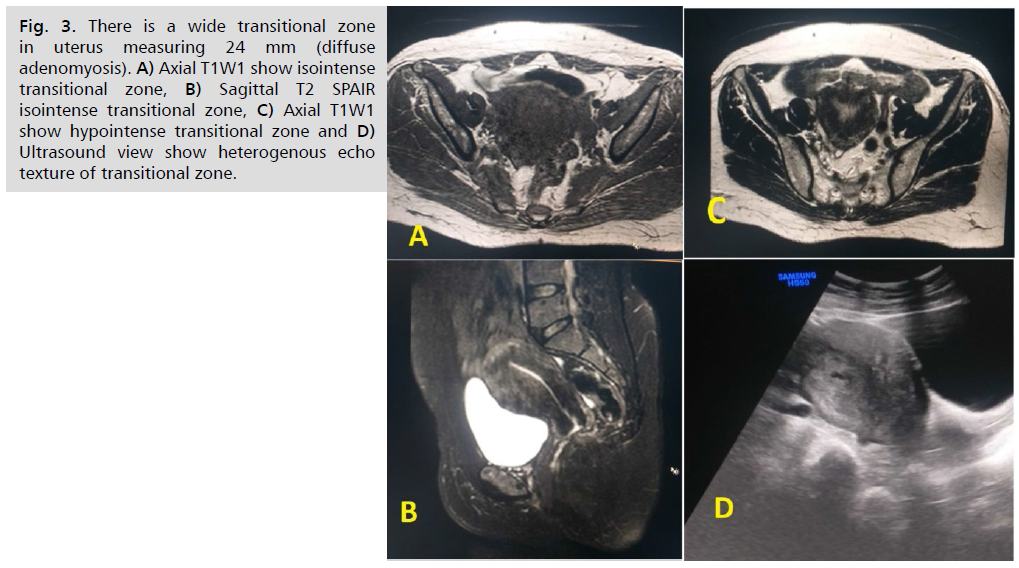
Fig. 3. There is a wide transitional zone in uterus measuring 24 mm (diffuse adenomyosis). A) Axial T1W1 show isointense transitional zone, B) Sagittal T2 SPAIR isointense transitional zone, C) Axial T1W1 show hypointense transitional zone and D) Ultrasound view show heterogenous echo texture of transitional zone.
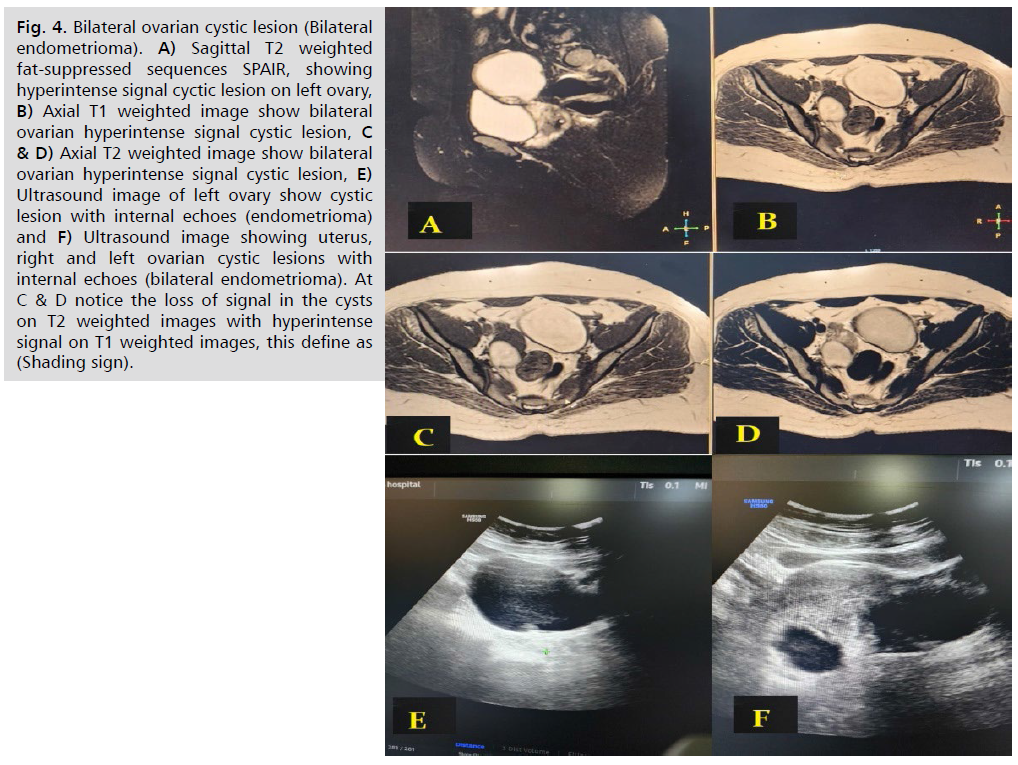
Fig. 4. Bilateral ovarian cystic lesion (Bilateral endometrioma). A) Sagittal T2 weighted fat-suppressed sequences SPAIR, showing hyperintense signal cyctic lesion on left ovary, B) Axial T1 weighted image show bilateral ovarian hyperintense signal cystic lesion, C & D) Axial T2 weighted image show bilateral ovarian hyperintense signal cystic lesion, E) Ultrasound image of left ovary show cystic lesion with internal echoes (endometrioma) and F) Ultrasound image showing uterus, right and left ovarian cystic lesions with internal echoes (bilateral endometrioma). At C & D notice the loss of signal in the cysts on T2 weighted images with hyperintense signal on T1 weighted images, this define as (Shading sign).
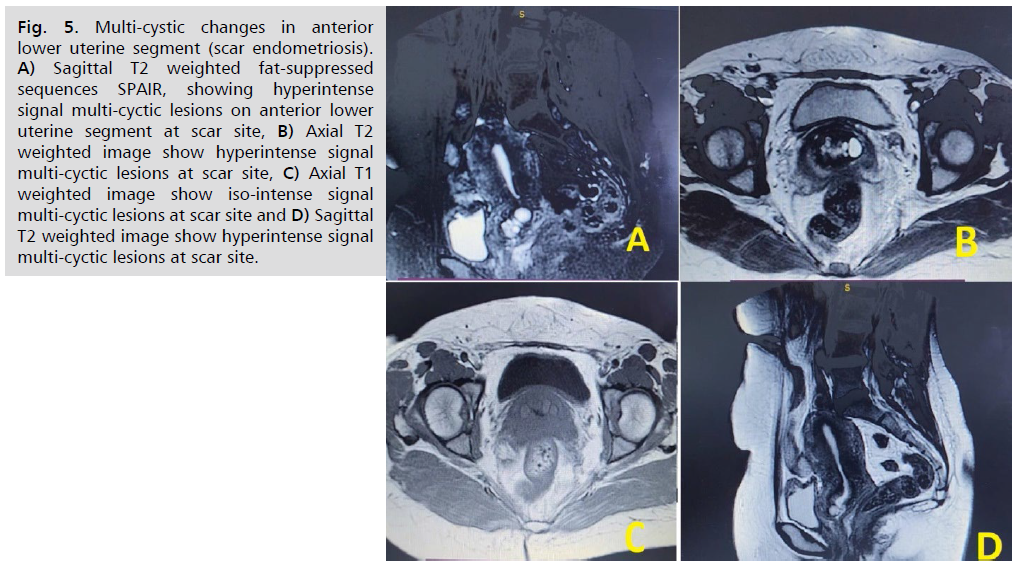
Fig. 5. Multi-cystic changes in anterior lower uterine segment (scar endometriosis). A) Sagittal T2 weighted fat-suppressed sequences SPAIR, showing hyperintense signal multi-cyctic lesions on anterior lower uterine segment at scar site, B) Axial T2 weighted image show hyperintense signal multi-cyctic lesions at scar site, C) Axial T1 weighted image show iso-intense signal multi-cyctic lesions at scar site and D) Sagittal T2 weighted image show hyperintense signal multi-cyctic lesions at scar site.
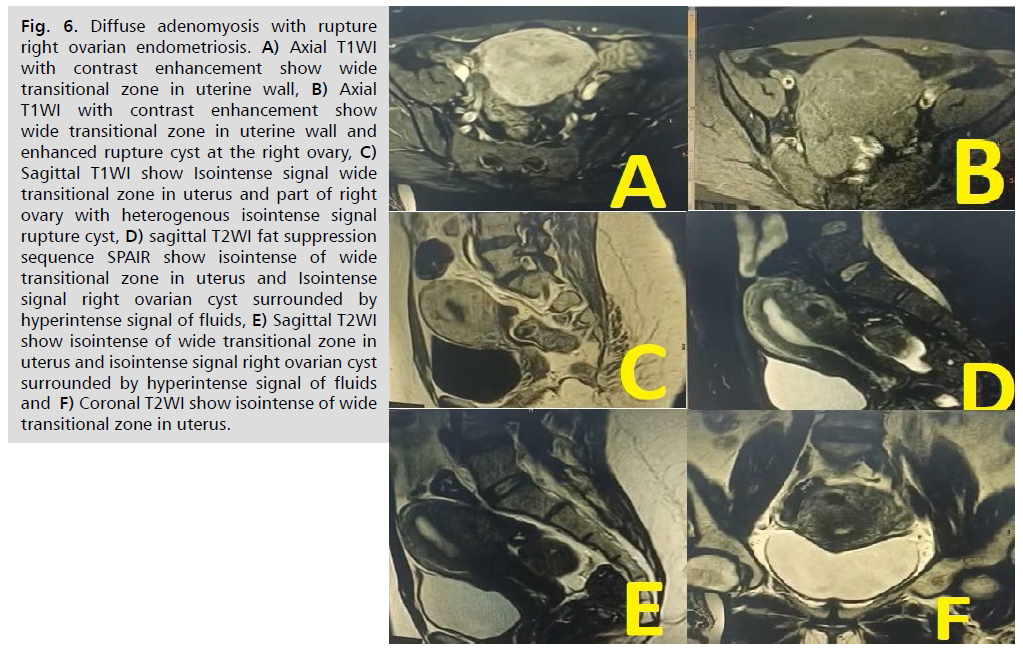
Fig. 6. Diffuse adenomyosis with rupture right ovarian endometriosis. A) Axial T1WI with contrast enhancement show wide transitional zone in uterine wall, B) Axial T1WI with contrast enhancement show wide transitional zone in uterine wall and enhanced rupture cyst at the right ovary, C) Sagittal T1WI show Isointense signal wide transitional zone in uterus and part of right ovary with heterogenous isointense signal rupture cyst, D) sagittal T2WI fat suppression sequence SPAIR show isointense of wide transitional zone in uterus and Isointense signal right ovarian cyst surrounded by hyperintense signal of fluids, E) Sagittal T2WI show isointense of wide transitional zone in uterus and isointense signal right ovarian cyst surrounded by hyperintense signal of fluids and F) Coronal T2WI show isointense of wide transitional zone in uterus.
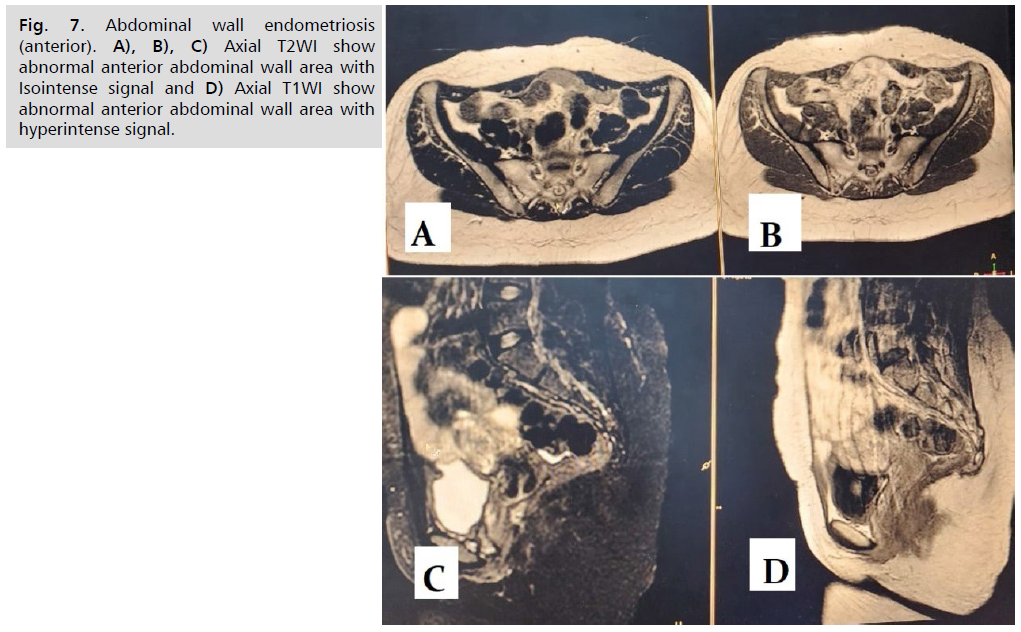
Fig. 7. Abdominal wall endometriosis (anterior). A), B), C) Axial T2WI show abnormal anterior abdominal wall area with Isointense signal and D) Axial T1WI show abnormal anterior abdominal wall area with hyperintense signal.
Abdelghany, et al. [23] noticed that most lesions appeared intense (65.5%) in T1WI and hypointense (48.3%) in T2WI with significant difference (p < 0.05). Abo-Gamra, et al. [25] concluded that the endometriotic lesions diagnostic MRI findings are hyperintense signal in T1W1 and intermediate or hyposignal intensity in T2W1.
Endometriosis diagnosis depends on the laparoscopy, plus histopatholologic confirmation which are an invasive procedures with several complications and false-negative findings. Authors suggested to raising literatures supporting the values of imaging modalities to elevating the diagnostic accuracy of ovarian and deep endometriosis [26].
Conclusion
Younger age women are the most commonly detection with endometriosis. The common MRI findings of endometriosis include anterior segment lesion, stage III, moderately severe, deep seated, large cystic, bilateral and densely adhesion. The most common findings of US are homogeneous slow-level echoes sign and thick-walled cystic appearance. Statistically, the diagnosis of endometriosis by MRI had better agreement than US.
Ethical Approval
The study was approved by The Medical Ethical Committee of College of Medicine, University of Babylon.
Conflict of Interest
None.
Funding
None.
References
- Harada T. Endometriosis: A mysterious disease. Endometriosis: Pathogenesis and Treatment. 2014:3-6.
- Peterson CM, Johnstone EB, Hammoud AO, et al. Risk factors associated with endometriosis: Importance of study population for characterizing disease in the ENDO Study. Am J Obstet Gynecol. 2013;208:451-e1.
- Naji TS, Al-Rubae SH, Turki KM. The association between hormonal variation, antioxidant status and oxidative stress in Iraqi women with endometriosis. J Faculty Med Baghdad. 2016;58:192-196.
- Al-Rubae SH. Studies on hormonal changes, homocysteine and lipids profile in Iraqi women with infertility. J Tech. 2012;25.
- Abdul-Rasheed OF, Farid YY. Development of a new high performance liquid chromatography method for measurement of coenzyme Q10 in healthy blood plasma. Saudi Med J. 2009;30:1138-1143.
- Sasson IE, Taylor HS. Stem cells and the pathogenesis of endometriosis. Ann N Y Acad Sci. 2008;1127:106-115.
- Stewart CJR, Ayhan A, Fukunaga M, et al. Endometriosis and related conditions. In: WHO Classification of Tumours Editorial Board, ed. WHO classification of tumours female genital tumours, 5th ed. Lyon: IARC Lib Cataloguing-in-Pub Data. 2020:169-174.
- Bazot M, Daraï E. Diagnosis of deep endometriosis: Clinical examination, ultrasonography, magnetic resonance imaging, and other techniques. Fertil Steril. 2017;108:886-894.
- Bazot M, Lafont C, Rouzier R, et al. Diagnostic accuracy of physical examination, transvaginal sonography, rectal endoscopic sonography, and magnetic resonance imaging to diagnose deep infiltrating endometriosis. Fertil Steril. 2009;92:1825-1833.
- Tanaka YO, Okada S, Yagi T, et al. MRI of endometriotic cysts in association with ovarian carcinoma. Am J Roentgenol. 2010;194:355-361.
- Vimercati A, Achilarre MT, Scardapane A, et al. Accuracy of transvaginal sonography and contrast‐enhanced magnetic resonance‐colonography for the presurgical staging of deep infiltrating endometriosis. Ultrasound Obstet Gynecol. 2012;40:592-603.
- Bazot M, Bharwani N, Huchon C, et al. European Society of Urogenital Radiology (ESUR) guidelines: MR imaging of pelvic endometriosis. Eur Radiol. 2017;27:2765-2675.
- Bazot M, Daraï E, Benagiano GP, et al. ENDO_STAGE magnetic resonance imaging: Classification to screen endometriosis. J Clin Med. 2022;11:2443.
- Working group of ESGE, ESHRE, and WES, Keckstein J, Becker CM, et al. Recommendations for the surgical treatment of endometriosis. Part 2: deep endometriosis. Hum Rep Open. 2020;2020:hoaa002.
- Thomassin-Naggara I, Lamrabet S, Crestani A, et al. Magnetic resonance imaging classification of deep pelvic endometriosis: Description and impact on surgical management. Hum Rep. 2020;35:1589-600.
- Bader SJ, Taj-Aldean KA. Role of Diffusion Weighted Imaging (DWI) of MRI Study in differentiation between adenomyosis and fibroids of the uterus in Al-Hilla Teaching Hospital. Med J Babylon. 2017;14:606-615.
- Garcia L, Isaacson K. Adenomyosis: Review of the literature. J Minim Invasive Gynecol. 2011;18:428-437.
- Vercellini P, Viganò P, Somigliana E, et al. Adenomyosis: Epidemiological factors. Best Pract Res Clin Obstet Gynaecol. 2006;20:465-477.
- Khan AT, Shehmar M, Gupta JK. Uterine fibroids: Current perspectives. Int J Womens Health. 2014:95-114.
- Guo Y, Cai YQ, Cai ZL, et al. Differentiation of clinically benign and malignant breast lesions using diffusion‐weighted imaging. J Magn Reson Imaging. 2002;16:172-178.
- Koh DM, Collins DJ. Diffusion-weighted MRI in the body: Applications and challenges in oncology. Am J Roentgenol. 2007;188:1622-1635.
- Nouri B, Arab M, Nasiri M. Endometriosis: Clinical, magnetic resonance imaging and pathologic findings. J Obstet Gynecol Cancer Res. 2023;8:484-490.
- Abdelghany HS, Abdelsamie MA, Shaheen KI, et al. The clinical importance of magnetic resonance imaging with diffusion weighted images in diagnosis and treatment planning of endometriosis. Minia J Med Res. 2021;32:13-20.
- Mason BR, Chatterjee D, Menias CO, et al. Encyclopedia of endometriosis: A pictorial rad-path review. Abdom Radiol. 2020;45:1587-1607.
- Abo-Gamra SH, Abd-Elhafez AS, Thabet MA. Role of magnetic resonance imaging in diagnosis of Endometriosis. Egypt J Hosp Med. 2018;72:5067-5071.
- Jaramillo-Cardoso A, Shenoy-Bhangle A, Garces-Descovich A, et al. Pelvic MRI in the diagnosis and staging of pelvic endometriosis: Added value of structured reporting and expertise. Abdom Radiol. 2020;45(6):1623-1636.
- de Resende JA, Cavalini LT, Crispi CP, et al. Risk of urinary retention after nerve‐sparing surgery for deep infiltrating endometriosis: A systematic review and meta‐analysis. Neurourol Urodyn. 2017;36(1):57-61.
- Zilberman S, Ballester M, Touboul C, et al. Partial colpectomy is a risk factor for urologic complications of colorectal resection for endometriosis. J Minim Invasive Gynecol. 2013;20:49-55.
- Bazot M, Jarboui L, Ballester M, et al. The value of MRI in assessing parametrial involvement in endometriosis. Hum Rep. 2012;27:2352-2358.
- Mabrouk M, Raimondo D, Arena A, et al. Parametrial endometriosis: The occult condition that makes the hard harder. J Minim Invasive Gynecol. 2019;26:871-876.
- Bazot M, Darai E, Hourani R, et al. Deep pelvic endometriosis: MR imaging for diagnosis and prediction of extension of disease. Radiol. 2004;232:379-389.
- Poupon C, Owen C, Arfi A, et al. Nomogram predicting the likelihood of complications after surgery for deep endometriosis without bowel involvement. Eur J Obstet Gynecol Reprod Biol: X. 2019;3:100028.
- Nisenblat V, Bossuyt PM, Farquhar C, et al. Imaging modalities for the non‐invasive diagnosis of endometriosis. Cochrane Database Syst Rev. 2016;2:CD009591.
- Collinet P, Fritel X, Revel-Delhom C, et al. Management of endometriosis: CNGOF/HAS clinical practice guidelines–Short version. J Gynecol Obstet Hum Reprod. 2018;47:265-274.
- Kilickesmez O, Bayramoglu S, Inci E, et al. Quantitative diffusion-weighted magnetic resonance imaging of normal and diseased uterine zones. Acta Radiol. 2009;50:340-347.
- Erdem G, Celik O, Karakas HM, et al. Microstructural changes in uterine leiomyomas and myometrium: A diffusion-weighted magnetic resonance imaging study. Gynecol Obstet Invest. 2009;67:217-222.
- Alborzi S, Poordast T, Askary E, et al. Evaluation and comparison of the accuracy of transvaginal ultrasound and MRI for the diagnosis of deep rectal endometriosis: A cross‐sectional study. Int J Gynaecol Obstet. 2023;161:586-593.
- Menakaya U, Reid S, Lu C, et al. Performance of ultrasound‐based endometriosis staging system (UBESS) for predicting level of complexity of laparoscopic surgery for endometriosis. Ultrasound Obstet Gynecol. 2016;48(6):786-795.
- Royal College of Obstetricians and Gynaecologists (RCOG). Classification of laparoscopic procedures per level of difficulty.
- Tuttlies F, Keckstein J, Ulrich U, et al. ENZIAN-score, a classification of deep infiltrating endometriosis. Zentralbl Gynakol. 2005;127:275-281.
- Bartlett DJ, Burkett BJ, Burnett TL, et al. Comparison of routine pelvic US and MR imaging in patients with pathologically confirmed endometriosis. Abdom Radiol. 2020;45:1670-1679.
Author Info
Zahraa Abdulhussein Katea* and Kassim Amir Hadi Taj Al-DeanCopyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.