Case Report - (2022) Volume 17, Issue 4
Successful continuation of heterotropic pregnancy after surgically management of cornual pregnancy: A case report and literature review
Mohamed I Taema*, Ibrahim Ali and Amr SobhyReceived: 12-Nov-2022, Manuscript No. gpmp-22-79683; Editor assigned: 14-Nov-2022, Pre QC No. P-79683; Reviewed: 26-Nov-2022, QC No. Q-79683; Revised: 08-Dec-2022, Manuscript No. R-79683; Published: 29-Dec-2022
Abstract
Heterotopic pregnancy is the presence of an intrauterine gestational sac in addition to presence of an ectopic pregnancy. Its incidence is very rare but has increased with the use of ART, reaching up to 1% of these cases. Currently there are no clear guidelines regarding the management of heterotopic pregnancy, but agreed is excision of the ectopic pregnancy, conservation of the intrauterine pregnancy. In this case report, a 41 year old woman previous 3 CS pregnant at 6 weeks by ICSI presented with acute abdomen, diagnosed as heterotropic where cornual pregnancy was excised through laparotomy and conservation of intrauterine pregnancy and then follow up till delivery.
Conclusion: Heterotropic pregnancy has increased nowadays and cornual ectopic need special experience to face such surgical challenge.
Keywords
Heterotropic pregnancy; Ectopic pregnancy
Introduction
Heterotopic pregnancy is the presence of an intrauterine gestational sac in addition to presence of an ectopic pregnancy. Its incidence is very rare where in spontaneous pregnancy , it is approximately 1/30000 (1/10000 to 1/50000) but now-a-days this incidence has increased due to assisted reproductive techniques (ART) to be ranging from 1/100 to 1/360 [1]. A cornual ectopic pregnancy is a life-threatening condition with a mortality rate 6-7 times higher than that of the tubal ectopic pregnancy [2].
Case Presentation
The patient is 41 years old, G4 para 3 all by Caesarean sections all were females, she is pregnant on ICSI due to male factor (second marriage) , her embryo transfer was 15 February 2022, after missing her period, her pregnancy was confirmed by pregnancy test. She had lower abdominal pain and vaginal spotting, on examination the vital data were stable, abdominal examination revealed tenderness, rigidity with rebound tenderness all over lower abdomen. Pelvic examination revealed severe cervical motion tenderness, a Transvaginal scan (Fig. 1.) revealed 2 gestational sacs, one intrauterine with CRL 87 mm equivalent to 6 weeks + 6 days with positive fetal life and second sac was abnormally eccentric, intramurally embedded at the left cornu not related to the fundal endometrium with clearly visualized plane of cleavage with noted Serosal bulge over the sac. The gestation sac revealed smooth outline & show double wall sign, positive fetal life CRL equivalent to 6 weeks and 4 days and left corpus luteum cyst measuring 3.1x 3cm. Complementary 3D ultrasound scan was done revealing the same findings (Fig. 2.). .A provisional diagnosis of heterotropic pregnancy and the decision for immediate laparotomy and excision of the left cornual ectopic pregnancy together with partial salpingectomy were discussed with the patient and explaining to her that she might abort the normal sac and explained to her that laparoscopy was difficult due to prev ous multiple laparotomies. The patient signed the informed consent and preoperative preparation was alone.
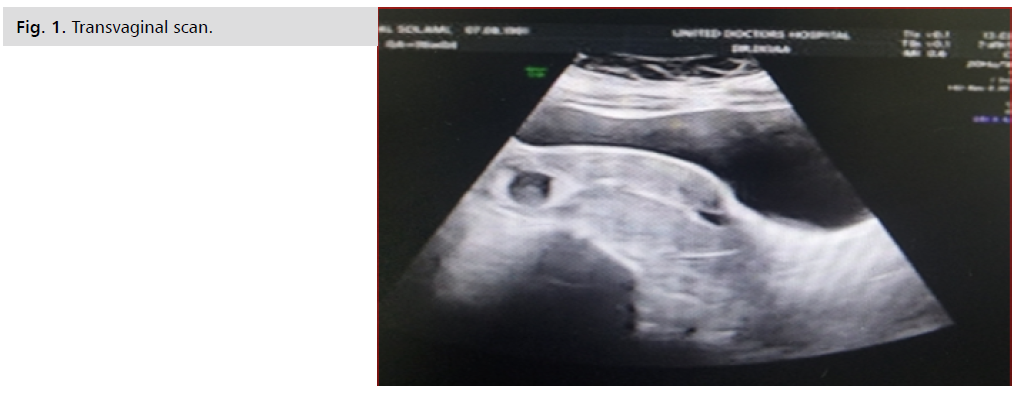
Fig 1. Transvaginal scan.
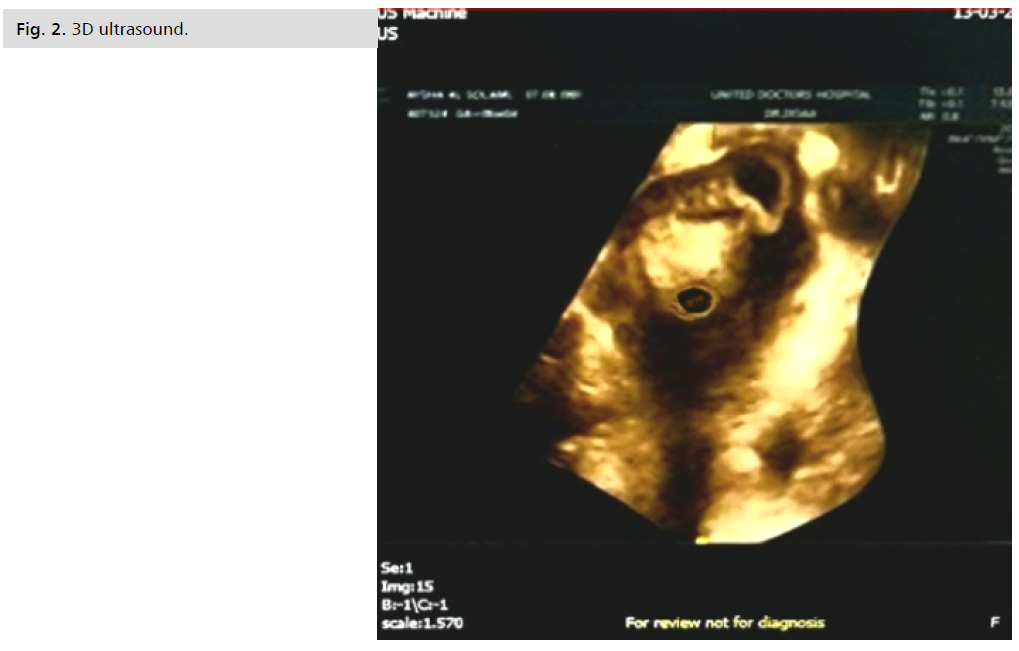
Fig 2. 3D ultrasound.
On laparotomy; left cornual ectopic pregnancy with bulging serosa 5 x 4 cm (Fig. 3. ), bilateral uterine artery temporary occlusion was done using foley catheter through a bilateral small opening in broad ligament, then burse string suture by vicryl 0 just below the cornual bulge to decrease the bleeding. Excision of the left cornual pregnancy then closure in a continuous manner by vicryl 0 suture. Partial left salpingectomy and ovarian cystectomy was done 2nd day post-operative the patient hemoglobin was 11.2 gm/ dl.
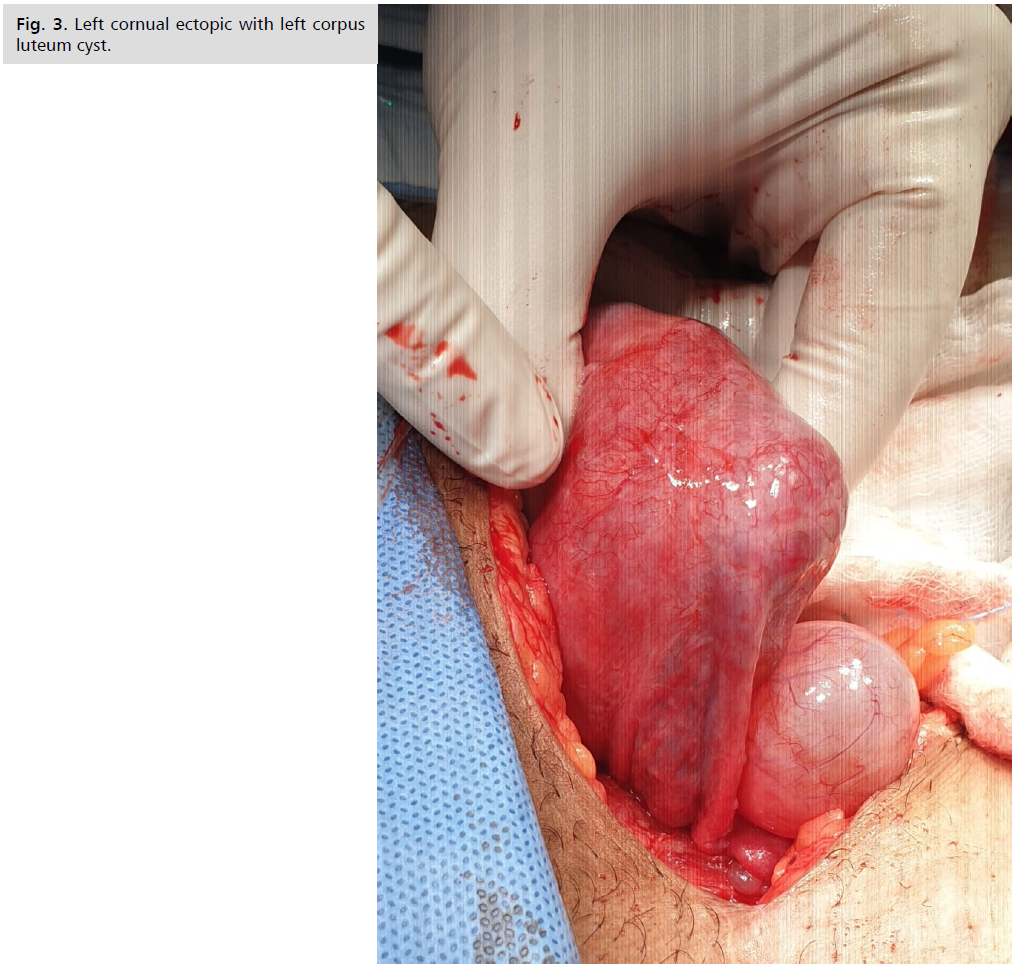
Fig 3. Left cornual ectopic with left corpus luteum cyst.
According to the patient wish, she passed his first postoperative week in the hospital and left after removal of sutures. The pathology slides revealed chorionic villi; fragments of amniotic membrane admixed with myometrial tissue and decidualized endometrial fragments. Myometrial infiltration by intermediate trophoblasts was noticed. Some areas of the myometrium were observed closely related to chorionic villi after discharge she was kept on vaginal progesterone 400 mg once daily before bed time. She had her regular antenatal visits till week 36 where she had premature contractions and delivered a healthy boy by repeat CS.
Discussion and Literature Review
Heterotopic pregnancy is the presence of an intrauterine gestational sac in addition to presence of an ectopic pregnancy. Its incidence is very rare where in spontaneous pregnancy, it is approximately 1/30000 (1/10000 to
1/50000) but nowadays this incidence has increased due to assisted reproductive techniques (ART) to be ranging from 1/100 to 1/360 [1].
Other risk factors for Heterotopic pregnanacy are pelvic inflammatory disease, pelvic surgery, and previous damage or pathology to fallopian tube [4]. Our patient did not have any of these risk factors and got pregnant spontaneously, which makes this case very rare and hard to be detected.
In 95% of cases, the ectopic pregnancy is located in the fallopian tube, but it can also be found in other sites as cervix, scar from a previous cesarean section, the interstitial segment of a fallopian tube, ovary, peritoneal, or abdominal cavity. The apparent increase in the incidence of nontubal ectopic pregnancies (EP) including Heterotopic pregnancy may be attributed to the higher number of pregnancies after in vitro fertilization treatment [3]. Our case described a case of an EP in the left fallopian tube.
The symptoms of Heterotopic pregnancy are nonspecific. Heterotopic Pregnancy can be asymptomatic in 24% of cases. symptoms may be presented as Abdominal pain (the most frequent symptom), vaginal bleeding and
hypovolemic shock. Vaginal bleeding and hypovolemic shock often indicate the rupture of the Ectopic Pregnancy and require urgent treatment [5]. Our patient was admitted to the emergency room complaining of the pain in the abdomen and vaginal spotting.
The early diagnosis of an ectopic pregnancy is possible due to a combination of serum measurements β- hCG and ultrasound. A doubling time of serum β-h CG of 66% was previously used in the early 80s. Following that a doubling time of 53% and more recently 35% or more, over a 48hours period, was suggested. Another concept in the early diagnosis of ectopic pregnancies is the discriminatory zone with levels 1500–2000 mIU/mL, or more recently a conservative level 3500 mIU/mL was suggested [6]. Unfortunately, in Heterotopic Pregnancy, both concepts; the discriminatory zones and the doubling time, commonly used in early diagnosis of ectopic pregnancy, are unhelpful, leads to an increased risk of misdiagnosis, with a third to half of Heterotopic Pregnancy cases thus presenting late and have already ruptured before a diagnosis was reached. The level of serum β- hCG in Heterotopic Pregnancy represents the combination of both the intrauterine level (mainly) and extrauterine pregnancy one and are unlikely to be of clinical use for the diagnosis of a Heterotopic Pregnancy. Furthermore, visualizing both intrauterine and extrauterine fetal heart activity although can be diagnostic but unfortunately is rare [7]. In this case, both a serum β-hCG measurement and transvaginal US were done at the emergency room, and Heterotopic Pregnancy was suspected because both embryos were visualized and one of them was outside the uterus.
Although ultrasound remains the main imaging modality in ectopic and Heterotopic pregnancies, a subset of patients may need further imaging using MRI (magnetic resonance imaging) to provide additional information. In a review of 1737 patients exposed to first trimester MRI exposure, as compared with non- exposure, there was no associated increased risk of harmful effect on the fetus or in early childhood of up to four years of age, this includes the risk of stillbirth or neonatal death within twenty-eight days of birth and any congenital anomaly, neoplasm, vision and hearing loss. In contrast, Gadolinium MRI during pregnancy was associated with an increased risk of stillbirth and neonatal death and a broad spectrum of rheumatological, inflammatory, or infiltrative skin conditions [8]. Ultrasound remains the best imaging modality option in pregnancy. MRI in selected patients, has
another advantage due to its excellent soft tissue contrast without using of ionizing radiation. Findings on MRI include: dilation of the tube and wall enhancement, tubal hematoma, hematoma of the adnexa, and a gestational saclike structure [8].
Treatment options include: expectant management, surgical management (either laparoscopy or laparotomy), and ultrasound-guided embryo aspiration with or without embryo-killing drugs. Treatment depends on the patient’s condition, the size and site of an Ectopic Pregnancy, previous pregnancies, the viability of intrauterine and extrauterine pregnancy, and the expertise of the treating physicians [9].
Expectant management can be selected in asymptomatic patients where the unruptured ectopic embryo has a limited craniocaudal length with no cardiac activity and a decreasing β-hCG level [10].
Any treatment for Heterotopic Pregnancy should aim to target the ectopic pregnancy, selectively, without any harm to the ongoing intrauterine pregnancy. With this concept in mind, using systemic methotrexate is contraindicated with a viable intrauterine pregnancy. Local treatment options have thus been suggested to avoid the use of systemic agents in Heterotopic pregnancy, and these include local injection of potassium chloride (KCL) and hyperosmolar glucose [11].
Although local injections of these agents avoid surgery the risk of treatment failures and subsequent surgery and salpingectomy is high, reaching 55%, making them not an attractive option in the context of Heterotopic Pregnancy with the other pregnancy in the tube. These modalities, however, may have a place in ectopic pregnancies with no coexisting intrauterine pregnancy, scar pregnancies or in Heterotopic Pregnancy where the extrauterine sac is in an unusual location as in cervical or corneal types [12].
For hemodynamically unstable patients or with any signs indicating the rupture of extrauterine pregnancy, emergency surgery is strongly recommended. The advantage of surgical treatment is the ability to completely remove an Ectopic Pregnancy, but there might be a higher abortion rate of an intrauterine embryo. In their study, Li J-B et al. found that the total abortion rate was 26.56% in all Heterotopic Pregnancy patients and the abortion rate in surgery management group was 25.93%. About 60–70% of Heterotopic Pregnancy cases result in live childbirth with outcomes similar to that of singleton pregnancies [9]. In our case, we performed an urgent laparotomy as the patient has multiple cesarean sections and left salpingectomy was done. The postoperative period was successful with normal growth of the IU embryo and continuation of pregnancy till week 36 where she had premature contractions and delivered a healthy boy by repeated CS.
Luteal phase support postoperatively in these cases remains controversial. There have yet to be research works that suggest that use of progesterone in these conditions would increase the live birth rate. E. Weedin et al. conducted a survey to evaluate progesterone supplementation using in non-ART (assisted reproductive techniques) infertility treatments and revealed that the empiric use of lutealphase progesterone supplementation in these treatments is widespread among clinicians even though there is lack of evidence to support its benefit [13]. The use of progesterone is also prevalent in women suffering from bleeding in early pregnancy who suspect that the bleeding occurs as a result of low progesterone. Nonetheless, many studies have not found a significantly higher incidence of live births when progesterone is prescribed for women with first trimester bleeding and no other risk factors as a prophylaxis for miscarriage [14]. However, for women who have both a history of previous miscarriage and bleeding in the first trimester, progesterone can have benefit in reducing the risk of miscarrying a fetus [15]. Even though in our case, the patient had no history of miscarriages, vaginal progesterone was prescribed for luteal phase support as a safety warranty for this complicated case.
What is new in this case is successful continuation of heterotropic pregnancy after surgically management of cornual pregnancy.
Conclusion
The continuation of this pregnancy should not less us neglect the fact that IVF doctors should be cautious in not transferring more than one embryo as heterotropic pregnancy has increased nowadays which may lead to serious complications.
Ethics
Written informed consent was obtained from the patient for publication of this case report and all accompanying images. No Ethical review Board is needed in our hospital to publish case reports.
Consent for Publication
Patient gave written consent for publication.
Data Statement
Data including video of laparoscope and patient mobile number available upon request.
Conflict of Interest
The authors have no conflicts of interest to declare.
Funding
This study received no financial support.
Acknowledgements
Not applicable.
References
- Chen L, Sun W, Hao L, et al. Successfully Managing Cornual Heterotopic Pregnancy: A Case Report and Literature Review. Chinese Chin Med Sci J. 2021;36(2):161-170.
- Tufan C, Georgescu C, Bohiltea R, et al. Cornual Heterotopic Pregnancy–a Rare Cause for Haemorrhagic Shock. Maedica. 2015;10(4):357.
- Oron G, Tulandi T. A pragmatic and evidence-based management of ectopic pregnancy. J Minim Invasive Gynecol. 2013;20(4):446-454.
- Yu Y, Xu W, Xie Z, et al. Management and outcome of 25 heterotopic pregnancies in Zhejiang, China. Eur J Obstet Gynecol Reprod Biol. 2014;180:157-161.
- Nabi U, Yousaf A, Ghaffar F, et al. Heterotopic pregnancy-a diagnostic challenge. Six case reports and literature review. Cureus. 2019;11(11).
- Barnhart KT, Guo W, Cary MS, et al. Differences in Serum Human Chorionic Gonadotrophin Rise in Early Pregnancy by Race and Value at Presentation. Obstet Gynecol. 2016;128(3):504.
- Soares C, Maçães A, Veiga MN, et al. Early diagnosis of spontaneous heterotopic pregnancy successfully treated with laparoscopic surgery. BMJ Case Rep. 2020;13(11).
- Ray JG, Vermeulen MJ, Bharatha A, et al. Association between MRI exposure during pregnancy and fetal and childhood outcomes. Jama. 2016;316(9):952-961.
- Li JB, Kong LZ, Yang JB, et al. Management of heterotopic pregnancy: experience from 1 tertiary medical center. Medicine. 2016;95(5).
- Baxi A, Kaushal M, Karmalkar HK, et al. Successful expectant management of tubal heterotopic pregnancy. J Hum Reprod Sci. 2010;3(2):108.
- Hutchinson M, Chan C. Laparoscopic management of ruptured heterotopic pregnancy after intrauterine insemination. CMAJ. 2016;188(17-18):E525-E527.
- Li Q, Xu H, Wang Y, et al. Ultrasound-guided local methotrexate treatment for cesarean scar pregnancy in the first trimester: 12 years of single-center experience in China. Eur J Obstet Gynecol Reprod Biol. 2019;243:162-167.
- Weedin E, Kort J, Quaas A, et al. Progesterone supplementation for luteal phase support in non-assisted reproductive technology treatments-prevalence of use and practice patterns among infertility specialists. Fertil Steril. 2016;106(3):e326-e327.
- Coomarasamy A, Devall AJ, Cheed V, et al. A randomized trial of progesterone in women with bleeding in early pregnancy. N Engl J Med. 2019;380(19):1815-1824.
- Haas DM, Hathaway TJ, Ramsey PS. Progestogen for preventing miscarriage in women with recurrent miscarriage of unclear etiology. Cochrane Database Syst Rev. 2019(11).
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Author Info
Mohamed I Taema*, Ibrahim Ali and Amr SobhyCopyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.