Research - (2024) Volume 19, Issue 3
Study the change of BMI and follow-up of lipid profile in obese patients before and after laparoscopic sleeve gastroectomy and liposuction
Karrar Sadeq Khudhair1*, Estabraq Kwaeri Al-Wasiti1, Anees K. Nile2, Ammar S.Al Khafaji3 and Baneen Ali Naji4Received: 02-Sep-2024, Manuscript No. gpmp-24-148213; Editor assigned: 03-Sep-2024, Pre QC No. P-148213; Reviewed: 14-Sep-2024, QC No. Q-148213; Revised: 21-Sep-2024, Manuscript No. R-148213; Published: 30-Sep-2024
Abstract
Background: Obesity is a chronic and debilitating disease that has become a global epidemic. People who are obese have increased morbidity, mortality and reduced Life Expectancy (LE) when compared to those with healthy weight. The medical therapy has achieved great progress. However, many patients still exposed to the complications of the disease. Laparoscopic Sleeve Gastrectomy (LSG) causes weight loss and metabolic improvement. While Liposuction (LS) is the most commonly performed cosmetic surgical procedure worldwide. Matrix Metalloproteinases (MMPs) are involved in physiological and pathological complications of obesity or metabolic syndrome through the degradation and remodeling of the extracellular matrix (ECM) molecules. Leptin and ghrelin play a significant role on the energy balance, food intake and body weight regulation.
Objectives: Measure the levels of lipid profile and BMI before and after Liposuction and laparoscopic sleeve gastrectomy in obese women. Methods A case study of 40 women with age range (18-60 years) was included in this study and the BMI more than 30 kg/m2. All surgeries were performed by the different team and were completed as scheduled according to the standard protocols. All patients were scheduled to return for a follow-up visit with their surgeon one month. Follow-up evaluations included estimation of lipid profile.
Results: After one month for both LSG and LS the result observed there were high significantly differences between the LSG and LS in BMI before and after operation respectively (44.27 ± 5.36 kg/m2 vs. 32.93 ± 3.48 kg/m2, 39.9315 ± 5.123, 31.557 ± 3.314 kg/m2) (p=0.0001). In current study the level of cholesterol, TG, LDL and VLDL there were decrease significantly in LSG but no significant difference in level of these parameters in LS. While there was no significant difference in HDL level in both LSG and LS. The correlation between parameters in post-LSG revealed a positive correlation between BMI and MMP-9 concentration, total cholesterol with LDL, TG with VLDL and leptin with MMP-9 concentration when compared with post LS that showing a positive correlation between BMI with MMP-9 concentration, total cholesterol with HDL and LDL, TG with VLDL, ghrelin with VLDL and leptin with MMP-9 concentration.
Conclusion: From the result of the current study the LSG have a highly effective treatment for obese women to loss body weight in contrast with LS, because the LS consider as a cosmetic surgery and have a localized effective of the body.
Keywords
BMI; LSG; LS; Lipid profiles
Introduction
Obesity is linked with elevated risk of Non-Communicable Diseases (NCDs). An increasing trend in obesity prevalence since the early 1980s has posed a significant population health burden across the globe while obesity prevalence varies by region and country. Country-specific trends in obesity are generally tracked using longitudinal panel or repeated cross-sectional data, with the highest-quality studies using measured anthropometry [1]. Currently, 30% of the world’s population is overweight or obese. By 2020, it is estimated that over 60% of the world’s population will be overweight or obese. Estimates suggest that the prevalence of severe obesity in 2030 will be 11%, roughly twice the current prevalence. Obesity disproportionately affects minorities, single mothers, and lower socioeconomic groups. In addition, the rate of obesity within the adolescents is escalating [2].
Morbid or grade III obesity is assigned as a body mass index (BMI) above 40 m/kg2 and characterized by a dramatic increase in the risks of comorbidities such as diabetes, Cardiovascular (CV) diseases, Obesity-Hypoventilation Syndrome (OHS), and cancers. Moreover, morbid obesity was linked to an elevated hazard of psychic disorders such as depression and anxiety. Although diet, lifestyle modifications, and pharmacologic therapy are common options for the treatment of adiposity [3]. In the case of bariatric surgery, the major drive for weight loss is the post-operative establishment of a state of profound negative energy balance, leading to the long-term restoration of peripheral insulin sensitivity. The sustained reductions in energy intake post-surgery primarily depend upon the reduction of hunger and induction of satiety [4]. This may relate to either early post-prandial distention of a reduced-capacity upper gastrointestinal pouch sending satiety signals through the afferent vagal pathways, or to the modulation of hunger and satiety signaling networks in subcortical brain areas regulating energy intake. The latter mechanism involves an augmented post-prandial secretion of satiety-inducing gut peptides such as Glucagon-Like Peptide 1 (GLP-1), Peptide YY (PYY) and Oxyntomodulin (OXM), combined with a diminished secretion of orexigenic hormones such as ghrelin and possibly altered leptin signaling in the hypothalamus [5]. Additional factors promoting weight loss after bariatric surgery include increased total energy expenditure and enhanced meal-induced thermogenesis, post-surgical changes in gut microbiota and altered bile acid physiology [6].
The Sleeve Gastrectomy (SG) has become the most commonly performed bariatric operation in the United States. The SG was originally the first stage of the duodenal switch, but has become used as a primarily standalone procedure. It is less technically challenging than a Roux-en-Y Gastric Bypass (RYGB) and some data suggests that it has less perioperative complications than a RYGB [7]. The Sleeve Gastrectomy (SG) is the most efficient method of obesity treatment. Many studies have shown that bariatric surgery not only helps patients achieve long-term weight loss but also removes obesity-related complications, including T2DM and high blood pressure. It has been demonstrated that weight-loss by laparoscopic sleeve gastrectomy leads to a 40%–65% reduction in excess weight [8]. Sleeve gastrectomy is reported to be effective both in the reduction of adipose tissue mass and in the improvement of the obesity-associated co-morbidities [9]. Liposuction is the most commonly performed cosmetic surgical procedure worldwide. Originally designed to correct unaesthetic superficial and deep deposits of subcutaneous fat, it produces highly satisfactory silhouette contouring when performed by appropriately trained operators using properly selected technologies for well-selected patients and anatomical areas [10].
Material and Methods
The study design
A case study of 40 women with age range (18-60 years) was included in this study and the BMI more than 30 kg/m2. This study was pre-experimental pretest-posttest design; it was carried out in department of Chemistry and Biochemistry / Collage of Medicine / Al-Nahrain University, -Al Mustanseria Hospital Private, Baghdad Teaching Hospital, Al Imamain Al Kadhimain Teaching and Alkafeel Specialty Hospital. The Inclusion Criteria: Age of obese patients (18-60) years with BMI more than 30 kg/m2 and Apparently health well (physically and mentally). Exclusion Criteria: Known case of inflammation anywhere depending on the CRP.
Blood sample collection and storage
10 ml of blood sample for biochemical analysis will be taken before one hour and after one month of Liposuction and sleeve gastrectomy procedure.
The Preparation of serum sample occurs in 3 stages:
- Seven milliliters of blood samples will be left for 20 minutes at room temperature.
- After coagulation, sera will be separated by centrifugation at 3000 rpm for 10 min.
- Sera will be aspirated and divided into small aliquots and stored at -80◦C until used.
Statistical analysis
The version twelve of the computer program, SPSS, which has been utilized for data analysis. the data have been represented as mean standard deviation (± Sd). they were estimated differences among groups via using T test with the P value (i.e. the least significant difference) has been found for the comparison amongst the groups, and the results have been considered to have statistical significance at (p ≤ 0.05).
Results
Demographic Characteristics of Laparoscopic Sleeve Gastrectomy (LSG) and Liposuction (LS) groups
The mean age of the female subjects who underwent LSG surgery was 34.45 ± 10.4 years, with a range of 18 to 54 years. This was not significantly different from that of the women who underwent LS, with a mean age of 31.65 ± 5.54 years, and a range of 23 to 40 years. As illustrated in Fig. 1., this finding is consistent with the observed difference in the age distribution between the two groups. The majority of patients undergoing LSG were women (70%), with a higher proportion of women in the LS group (100%) than in the LSG group. As illustrated in Tab. 1., the BMIs of the LSG and LS groups differed, with the former having a mean BMI of 44.27 ± 5.36 kg/m2 and the latter a mean BMI of 32.93 ± 3.48 kg/m2.
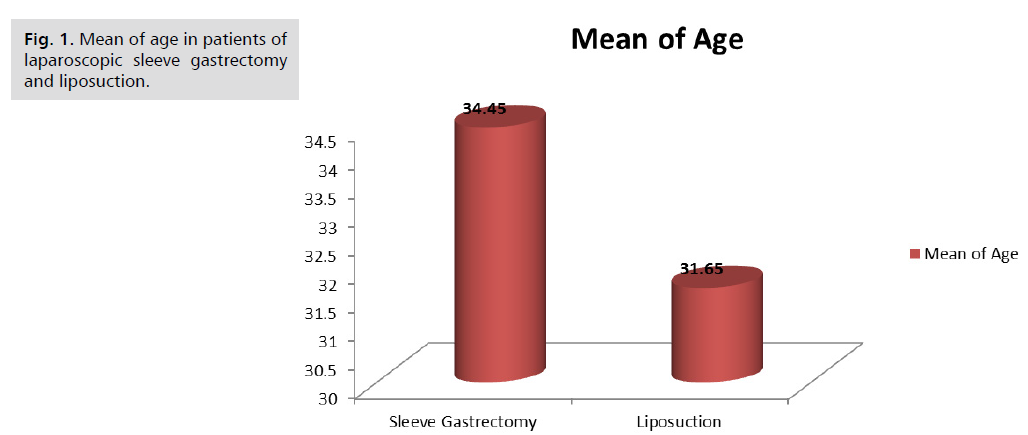
Fig. 1. Mean of age in patients of laparoscopic sleeve gastrectomy and liposuction.
| Variables | SG N=20 |
LS N=20 |
P value |
|---|---|---|---|
| Age (years) Mean ± SD Range |
34.45 ± 10.43 18 – 54 |
31.65 ± 5.54 23 – 40 |
0.2957 |
| BMI (kg/m2) Mean ± SD Range |
44.278 ± 5.369 35.32 – 53.75 |
32.934 ± 3.488 27.14 – 38.46 |
0.0001** |
Tab. 1. Demographic characteristics of the women.
Serum cholesterol level in study groups
Serum cholesterol concentration in patients underwent (LSG) and (LS) operations were show in Tab. 2. A highly significant reduction in Serum cholesterol concentration in (LSG), while there was no significant in (LS). The main Serum cholesterol was in pre and post (LSG) was 187.10 ± 30.071 mg/dl and 158.35 ± 14.702 mg/dl respectively, while the main cholesterol level was in pre and post (LS) 181.55 ± 37.888 mg/dl and 181.1 ± 31.848 mg/dl respectively (Tab. 2.).
| Type of operation | Pre-operation Mean ± SD |
Post-Operation Mean ± SD |
P value |
|---|---|---|---|
| laparoscopic Sleeve Gastrectomy | 187.10 ± 30.071 | 158.35 ± 14.702 | 0.0005 *** |
| Liposuction | 181.55 ± 37.888 | 181.1 ± 31.848 | 0.9678 |
Tab. 2. Cholesterol level in (mg/dl) of patients.
Serum triglyceride level in study groups
Serum triglyceride concentration in patients underwent (LSG) and (LS) operations were show in Tab. 3. A significant reduction in Serum triglyceride concentration in (LSG), while there was no significant in (LS). The main Serum triglyceride was in pre and post (LSG) was 135.25 ± 61.244 mg/dl and 98.40 ± 30.245 mg/dl respectively, while the main triglyceride level was in pre and post (LS) 101.85 ± 30.030 mg/dl and 101.9 ± 28.304 mg/dl respectively (Tab. 3.).
| Type of operation | Pre-operation Mean ± SD |
Post-Operation Mean ± SD |
P value |
|---|---|---|---|
| laparoscopic Sleeve Gastrectomy | 135.25 ± 61.244 | 98.40 ± 30.245 | 0.0208 * |
| Liposuction | 101.85 ± 30.030 | 101.9 ± 28.304 | 0.9957 |
Tab. 3. Triglyceride level in (mg/dl) of patients.
Serum HDL cholesterol level in study groups
Tab. 4. expresses the results of serum HDL cholesterol for both (LSG) and (LS) operations. There were no significant differences among comparison of (LSG) and (LS) pre and post operations. The main serum HDL cholesterol was in pre and post (LSG) 44.70 ± 7.342 mg/dl and 42.15 ± 6.587 mg/dl respectively, while the main HDL cholesterol was in pre and post (LS) 41.55 ± 7.444 mg/dl and 40.65 ± 5.274 mg/dl respectively (Tab. 4.).
| Type of operation | Pre-operation Mean ± SD |
Post-Operation Mean ± SD |
P value |
|---|---|---|---|
| Laparoscopic Sleeve Gastrectomy | 44.70 ± 7.342 | 42.15 ± 6.587 | 0.2549 |
| Liposuction | 41.55 ±7.444 | 40.65 ± 5.274 | 0.6616 |
Tab. 4. HDL Cholesterol level in (mg/dl) of patients.
Serum LDL cholesterol level in study groups
Serum LDL cholesterol concentration in patients undergoing (LSG) and (LS) operations were show in Tab. 5. A significant differences decrease in Serum LDL cholesterol concentration in (LSG), while there was no significant in (LS). The main Serum LDL cholesterol was in pre and post (LSG) was 94.20 ± 18.303 mg/dl and 78.95 ± 14.702 mg/dl respectively, while the main LDL cholesterol level was in pre and post (LS) 91.95 ± 21.984 mg/dl and 88.1 ± 20.698 mg/dl respectively (Tab. 5.).
| Type of operation | Pre-operation Mean ± SD |
Post-Operation Mean ± SD |
P value |
|---|---|---|---|
| Laparoscopic Sleeve Gastrectomy | 94.20 ± 18.303 | 78.95 ± 14.702 | 0.0061 ** |
| Liposuction | 91.95 ± 21.984 | 88.1 ± 20.698 | 0.5719 |
Tab. 5. LDL Cholesterol level in (mg/dl) of patients.
Serum VLDL cholesterol level in study groups
Serum VLDL cholesterol concentration in patients underwent (LSG) and (LS) operations were show in Tab. 6. A significant differences decrease in Serum VLDL cholesterol concentration in (LSG), while there was no significant in (LS). The main Serum VLDL cholesterol was in pre and post (LSG) was 27.015 ± 12.235 mg/dl and 19.685 ± 6.071 mg/dl respectively, while the main VLDL cholesterol level was in pre and post (LS) 20.32 ± 6.001 mg/dl and 20.55 ± 5.797 mg/dl respectively (Tab. 6.).
| Type of operation | Pre-operation Mean ± SD |
Post-Operation Mean ± SD |
P value |
|---|---|---|---|
| Laparoscopic Sleeve Gastrectomy | 27.015 ± 12.235 | 19.685 ± 6.071 | 0.0214 * |
| Liposuction | 20.32 ± 6.001 | 20.55 ± 5.797 | 0.9026 |
Tab. 6. VLDL Cholesterol level in (mg/dl) of patients.
Discussion
The present study recorded 40 patients have sleeve gastrectomy and liposuction between March 2021 to December 2021; the patients were divided into two groups. Group (A) twenty patients have sleeve gastrectomy , six(6) patients were males (30%), and fourteen (14) patients were females (70%). The mean age of patients was 44.27 ± 5.36 and BMI 44.278 ± 5.369 kg/m2. Group (B) twenty patients have liposuction all of them were females (100%) the mean age of patients was 31.65 ± 5.546 and BMI 32.934 ± 3.488 kg/m2 . Habib, et al., observed the total of 15 overweight and obese (BMI 26–35 kg/m2) premenopausal women found the main of age 31.27 ± 5.69 [11]. Also other authors Ghafoor, et al., showed the total 124 females with mean of age 37 ± 10.1 [12]. Interestingly, at the short term follow-up (one month postoperative follow-up), this data were entirely in line with other studies data showing that the LSG were have positive effect reduction on the TC , TG , LDL-c and VLDL while the LS have no significant difference on the lipid profile as showed in Tab. 2.-6. respectively. Up to date, there is little mid- and long-term information available about the metabolic effects of LSG, TOVAR et al., observed reduction in the triglyceride levels and the cardiovascular risk predictor triglyceride/HDL ratio and increased HDL levels after surgery and maintained them under normal ranges for at least two years [13]. As recently reviewed by Griffo, et al., reduce fasting and postprandial triglycerides and increase HDL cholesterol levels also increase HDL cholesterol levels follow-up one year after LSG [14], Vigilante, et al., observed a significant increment of HDL and level of LDL, TG, and non-HDL-C in patients with adequate weight loss one year after surgery [15].
The result of present study agree with Bettini, et al., reported a significant decrease of total cholesterol values (p<0.001), low density lipoprotein-cholesterol values (p<0.001) and triglycerides values (p=0.007) during eighteen months after surgery [16]. These results do not agree with another study by Zaki, et al., showed a significant change in HDL also, there were a no significant change in levels of TC and LDL post-operatively [17]. The results of previous studies on the metabolic effects of liposuction are not conclusive. The present study evaluate the effects of liposuction in the different region in women with body mass index 32.93 ± 3.48 kg/m2 on the parameters of enzymes and lipid profile as well as the hormones that may affect the metabolism of adipose tissue. The results of the present study showing that removing amount of abdominal subcutaneous fat by liposuction does not significantly affect the levels TC, HDL-c, LDL-c, TG and VLDL. Perhaps this is due to altered pathophysiology associated with lipodystrophy syndrome as opposed to the general population represented by studies conducted to date. Swanson (2011) showed preoperative high level of triglycerides in 36.8% of patients who have liposuction [18]. In previous studies the prior to the prospective clinical study by Swanson that look at changes in lipid profile associated with liposuction, have showing incongruent results and are mostly small groups (9–15 patients), which limit its statistical significance and are predominantly in obese female patients [19,20].
Gallardo, et al., after three months showed a significantly decrease in LDL and triglyceride values (P 0.04 and P 0.03), while there were no significant change in total cholesterol, VLDL and HDL-c (Ramos-Gallardo, Verdin, et al. 2013). Also Lubkowska, et al., found in 27 women at age 40.75 ± 13.67 years and BMI=25.9 ± 4.13 kg/m2 no significant changes in the lipid profile of the subjects were found [21]. While Doucas, et al., reported in 35 patients with deranged preoperative triglycerides (P=0.004), cholesterol (P=0.001), and LDL cholesterol (P=0.017) showed a significant decrease (P < 0.05) in postoperative levels [22].
Conclusion
The results of the present study indicate the abdominal liposuction considered a clinical therapy for obesity which removes large amounts of subcutaneous fat by liposuction in women with obesity may have cosmetic benefits, but the procedure does not significantly reduction in lipid profile.
Authors' Contribution
(A) Study Design · (B) Data Collection . (C) Statistical Analysis · (D) Data Interpretation · (E) Manuscript Preparation · (F) Literature Search · (G) No Fund Collection
References
- Inoue Y, Qin B, Poti J, et al. Epidemiology of obesity in adults: latest trends. Curr Obes Rep. 2018;7:276-288.
- Andolfi C, Fisichella PM. Epidemiology of obesity and associated comorbidities. J Laparoendosc Adv Surg Tech. 2018;28(8):919-924.
- Salman MA, El-Ghobary M, Soliman A, et al. Long-term changes in leptin, chemerin, and ghrelin levels following Roux-en-Y gastric bypass and laparoscopic sleeve gastrectomy. Obes Surg. 2020;30:1052-1060.
- Münzberg H, Laque A, Yu S, et al. Appetite and body weight regulation after bariatric surgery. Obes Rev. 2015;16:77-90.
- Behary P, Tharakan G, Alexiadou K, et al. Combined GLP-1, oxyntomodulin, and peptide YY improves body weight and glycemia in obesity and prediabetes/type 2 diabetes: a randomized, single-blinded, placebo-controlled study. Diabetes Care. 2019;42(8):1446-1453.
- Akalestou E, Miras AD, Rutter GA, et al. Mechanisms of weight loss after obesity surgery. Endocr Rev. 2022;43(1):19-34.
- Clapp B, Wynn M, Martyn C, et al. Long term (7 or more years) outcomes of the sleeve gastrectomy: a meta-analysis. Surg Obes Relat Dis. 2018;14(6):741-747.
- Choromańska B, Myśliwiec P, Łuba M, et al. A longitudinal study of the antioxidant barrier and oxidative stress in morbidly obese patients after bariatric surgery. Does the metabolic syndrome affect the redox homeostasis of obese people?. J Clin Med. 2020;9(4):976.
- Jamialahmadi T, Nematy M, Bo S, et al. Associations between pre-bariatric high-sensitivity c-reactive protein and post-surgery outcomes. Diagnostics. 2021;11(4):721.
- Francesco S, Nicolò B, Michele PG, et al. From liposuction to adipose-derived stem cells: indications and technique. Acta Biomed. 2019;90(2):197.
- Habib H, Abd Alazeem S, Abd Alazeem N. Fasting insulin level changes after large volume liposuction. Egyptian J Hosp Med. 2018;73(3):6243-6251.
- Ghafoor L, Entezari V, Fallah A, et al. Lipoabdominoplasty and the leptin hormone. Ann Med Surg. 2021;68.
- Ruiz-Tovar J, Oller I, Tomas A, et al. Midterm impact of sleeve gastrectomy, calibrated with a 50-Fr bougie, on weight loss, glucose homeostasis, lipid profiles, and comorbidities in morbidly obese patients. Am Surg. 2012;78(9):969-974.
- Griffo E, Cotugno M, Nosso G, et al. Effects of sleeve gastrectomy and gastric bypass on postprandial lipid profile in obese type 2 diabetic patients: a 2-year follow-up. Obes Surg. 2016;26:1247-1253.
- Vigilante A, Signorini F, Marani M, et al. Impact on dyslipidemia after laparoscopic sleeve gastrectomy. Obes Surg. 2018;28:3111-3115.
- Bettini S, Segato G, Prevedello L, et al. Improvement of lipid profile after one-anastomosis gastric bypass compared to sleeve gastrectomy. Nutrients. 2021;13(8):2770.
- Zaki MK, Al-Jefri OH, Kordi RE, et al. Correlation of bariatric surgery effect on lipid profile among obese patients. Cureus. 2021;13(9).
- Swanson E. Prospective clinical study reveals significant reduction in triglyceride level and white blood cell count after liposuction and abdominoplasty and no change in cholesterol levels. Plast Reconstr Surg. 2011;128(3):182e-97e.
- Samdal F, Birkeland KI, Ose L, et al. Effect of large-volume liposuction on sex hormones and glucose-and lipid metabolism in females. Aesthetic Plast Surg. 1995;19:131-135.
- Giese SY, Bulan EJ, Commons GW, et al. Improvements in cardiovascular risk profile with large-volume liposuction: a pilot study. Plast Reconstr Surg. 2001;108(2):510-519.
- Lubkowska A, Chudecka M. The effects of small-volume liposuction surgery of subcutaneous adipose tissue in the gluteal-femoral region on selected biochemical parameters. Int J Environ Res Public Health. 2019;16(18):3298.
- Doucas G, Liakos D, Koonin SD. The effect of lipectomy/liposuction on lipid profiles in antiretroviral drug-induced lipodystrophy syndrome. Plast Reconstr Surg. 2020;8(10):e3171.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Author Info
Karrar Sadeq Khudhair1*, Estabraq Kwaeri Al-Wasiti1, Anees K. Nile2, Ammar S.Al Khafaji3 and Baneen Ali Naji42Department of Clinical Laboratories, College of Applied Medical Science, Kerbala University, Kerbala, Iraq
3Department of Pharmacy, Al-Zahrawi University College, Karbala, Iraq
4Al-Zahraa University for Women, Karbala, Iraq
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.