Original Article - (2021) Volume 16, Issue 3
Role of 'Angle of Progression' in Prediction of Vaginal Delivery in Primiparous Women
Mohamed Ahmed Elkadi, Maida Ramadan Ewida* and Ahmed Mohammed ZenhomReceived: 17-Aug-2021 Published: 28-Sep-2021
Abstract
Background: In the recent years, there has been a definite increase in the ratio of caesarean sections. A caesarean section entails a bigger threat to the health and life of the woman giving birth compared to natural childbirth. Since the trend of increasing ratio of caesarean sections is an alarming one. Transperineal ultra-sonography (TPU) has been suggested to be a useful tool for monitoring labor progress and for predicting the mode of delivery. The angle of progression (AOP) is a parameter obtained by measuring the angle between the long axis of the symphysis pubis and a line extending from its most inferior edge tangentially to the fetal skull.
Objective: This study aims at evaluating the role of measuring the ‘angle of progression’ (AOP) at the onset of the active phase of labor in prediction of vaginal delivery in primiparous women.
Patients and Methods: Study Design: A diagnostic test accuracy study (prospective). Study setting: Department of obstetrics and gynecology at Ain Shams University Maternity Hospital (labour ward). Study time: Between May 2020and May 2021. Study population: Pregnant women attended Ain Shams University Maternity Hospital with the following criteria:
Results: This diagnostic test accuracy prospective study was conducted at Ain Shams University Maternity Hospital starting from May 2020 to evaluate the role of measuring the angle of progression (AOP) at the onset of the active phase of labor in prediction of vaginal delivery in 56 full term primiparous women. Statistical analysis of our results showed that vaginal delivery was in more than nine tenths (51 vs. 5) of the studied cases and no significant differences according to mode of delivery were detected between studied women regarding maternal age, BMI, fetal gestational age and fetal weight. Also, rupture of membranes was non-significantly more frequent in cases that delivered vaginally while station of fetal head, cervical dilatation, cervical effacement and angle of progression were significantly higher in cases that delivered vaginally. We can deduce that, angle of progression had significant high diagnostic performance; station of fetal head had significant moderate diagnostic performance, while cervical dilatation and cervical effacement had significant low diagnostic performance. Finally, angle of progression ≥97.0° had highest diagnostic characteristics, followed by station ≥0.0 station followed by cervical dilatation ≥5 cm and cervical effacement ≥75%. Different cut points had their sensitivity & NPV higher than their specificity & PPV.
Conclusion: In prediction of progress of spontaneous vaginal delivery in primiparous women, transperineal ultra-sonographic angle of progression with cutoff value ≥97.0° had highest predictive and diagnostic value, followed by station of fetal head ≥0.0 followed by cervical dilatation ≥5 cm and cervical effacement ≥75%. On the other hand rupture of amniotic membranes, maternal age, BMI, fetal gestational age and fetal weight had no significance in delivery progress prediction.
Keywords
Angle of progression; Transperineal sonography
Introduction
In the recent years, there has been a definite increase in the ratio of caesarean sections. A caesarean section entails a bigger threat to the health and life of the woman giving birth compared to natural childbirth. Since the trend of increasing ratio of caesarean sections is an alarming one [1].
Currently, the internal digital vaginal exam is the basis for the assessment of stage and progress of labor. However, there is much evidence that palpation performed during childbirth is inaccurate and does not allow for precise determining the progression of head in the birth canal and that it is prone to a high number of errors in the evaluation of position and lie of the presenting part in both the first and second stage of labor [2].
Transperineal sonography (TPU) has been suggested to be a useful tool for monitoring labor progress and for predicting the mode of delivery. The angle of progression (AOP) is a parameter obtained by measuring the angle between the long axis of the symphysis pubis and a line extending from its most inferior edge tangentially to the fetal skull [3].
AOP measured by transperineal ultrasound just after full cervical dilatation is determined were shown to be useful in predicting spontaneous vaginal delivery [4].
It has been shown that the AOP measurement, using transperineal sonography, is an easily preformed and reproducible method with little inter- and intra-observer variability [3].
The AOP has the potential to predict spontaneous vaginal delivery and the duration of the second stage of labor which may be useful in counseling patients and managing their labor [5].
We have previously shown that nulliparous women with a pre-labor wide AOP (≥95⁰) have high rate of successful vaginal delivery compared to those with a narrower angle [3].
Aim of the Work
This study aims at evaluating the role of measuring the ‘angle of progression’ (AOP) at the onset of the active phase of labor in prediction of vaginal delivery in primiparous women.
Patients and Methods
Study design: A diagnostic test accuracy study (prospective)
Study setting: Department of obstetrics and gynecology at Ain Shams University Maternity Hospital (labour ward)
Study time: Between May 2020and May 2021
Study population: Pregnant women attended Ain Shams University Maternity Hospital with the following criteria.
Inclusion criteria: Primiparous women. At the onset of the active phase of labor (defined as cervical dilatation ≥ 3 cm and cervical effacement ≥ 80%. Viable singleton pregnancy. Term pregnancy (37 – 41+6 weeks of gestation). Vertex presentation with occiput anterior position.
Exclusion criteria: Women with extremes of estimated fetal weight (sonographic estimated fetal weight < 2.5 kg or > 4 kg). Women undergoing induction of labor as the progression of labour may be affected and the progress of labor may not be normal. Women with chronic or acute fetal compromise because in the majority of cases normal vaginal delivery may be of a risk for the fetus. Multi-fetal pregnancy. Preterm pregnancies <37 weeks. Women refused to participate or continue the study.
Sampling method: Systemic random sample.
Sample size: 56 women.
Sample size justification: Sample size was calculated, setting the power (1-β) at 0.8 and the type-1 error (α) at 0.05. Data from a previous similar study [6] showed that AUC for AOP in prediction of vaginal elivery was 0.902. Therefore, 38 women who delivered vaginally were needed to find such an accuracy. Among primiparous women, who were at the onset of the active phase of labor, and assuming a rate of 20% of Cesarean section for failure of progress and a rate of 15% of Cesarean section for evident or suspected intrapartum fetal compromise, a minimal sample size of 56 women was needed.
Ethical considerations: Participating women signed informed written consent after thorough explanation of the details and purpose of the current study. Women had the right to withdraw from the study at any phase without being adversely impacted regarding the medical care she should receive. The study protocol was approved by the Ethical Research Committee of Obstetrics and Gynecology Department and Faculty of Medicine, Ain Shams University.
Study interventions and procedures:
All cases were subjected to:
Complete history taking: Personal, obstetric, medical surgical, etc.
General examination: Vital signs, BMI, etc.
Obstetric examination: Fundal, abdominal and pelvic grips
Pelvic examination:
• Cervix: Dilatation, effacement (length), consistency and position.
• Fetal head: Position and station.
• Fetal membranes: Intact or ruptured.
Trans-perineal ultrasound (TPU):
• Occiput anterior position was confirmed by visualization of the fetal cerebellum or cervical spine.
• Head station was determined.
• AOP was measured:
The ultrasound probe was located between the labia below the pubic symphysis in a mid-sagittal position. A sagittal view of the long axis of the pubic symphysis was obtained by a small lateral movement of the transducer, at the same plane, and a sagittal view of the leading position of the fetal head was determined. A line was drawn between the calipers placed at the two ends of the long axis of the pubic symphysis. A second line was drawn from the distal point of the pubic symphysis tangentially to the fetal skull contour. AOP was the angle between these two lines. The TPU scan was performed using the curved ultrasound probe with frequency 3.5 – 5 MHz of Samsung-Medison SonoAce X6 set (Fig. 1.).
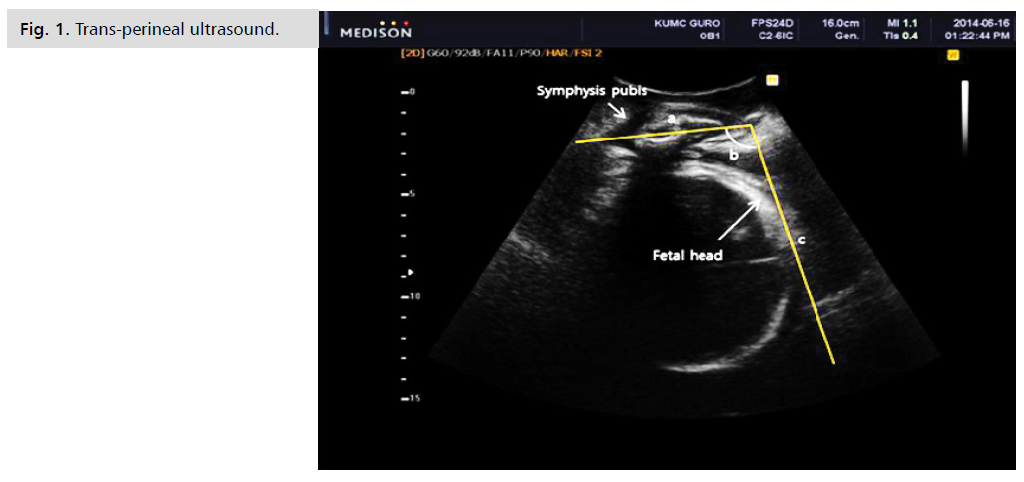
Figure 1: Trans-perineal ultrasound.
The scans were performed by one of three sonographers with at least 3-year experience in performing TPU scan (Fig . 1.).
• Head station and AOP were measured at the onset of active phase of labor and at the second stage of labor.
Outcomes:
Primary outcome: A rate of vaginal delivery.
Secondary outcome: Cutoff value of AOP to predict vaginal delivery and its clinical validity.
Statistical analysis
Statistical analysis was performed using MedCalc® version 7.0, setting the significance level at 0.05. Data were presented in terms of mean and standard deviation (for numeric normally-distributed variables), median and interquartile range (for numeric non-normally-distributed variables) or frequency and percentage (for categorical variables). Receiver operator characteristics (ROC) curves were constructed for measuring the predictability of AOP for vaginal delivery in included women. Predictability was presented in terms of sensitivity, specificity, positive and negative predictive values.
Statistical package
Data entry and statistical analysis of the collected data was performed by the use of a reliable genuine software program.
Results
Tab. 1. shows that maternal (age & BMI) and fetal (gestational age& weight) characteristics among the studied cases.
| Variables | Mean ± SD | Range |
|---|---|---|
| Maternal | ||
| Age (years) | 24.3 ± 4.6 | 17.0–37.0 |
| BMI (kg/m2) | 28.9 ± 3.2 | 23.0–36.0 |
| Fetal | ||
| Gestational age (weeks) | 38.6 ± 1.2 | 37.0–41.0 |
| Fetal weight (kg) | 3.1 ± 0.4 | 2.5–3.9 |
| Total = 56 | ||
Tab. 1. Maternal and fetal characteristics among the studied cases.
Tab. 2. shows that predictors of mode of delivery; rupture of membranes, station, cervical dilatation, cervical effacement and angle of progression.
| Variables | N | % |
|---|---|---|
| Rupture of membranes | 22 | 39.3 |
| Median (1st−3rd IQ) | Range | |
| Station | 0.0 (-1.0−1.0) | -2.0−2.0 |
| Mean ± SD | Range | |
| Cervical dilatation (cm) | 5.8 ± 1.4 | 4.0–9.0 |
| Cervical effacement (%) | 71.6 ± 11.1 | 50.0–100.0 |
| Angle of progression (°) | 107.5 ± 10.7 | 88.0–127.0 |
| Total=56. IQ: Interquartiles | ||
Tab. 2. Predictors of mode of delivery among the studied cases.
Tab. 3. shows that vaginal delivery was in more than nine tenths of the studied cases.
| Variables | N | % |
|---|---|---|
| Normal vaginal delivery | 51 | 91.1 |
| Cesarean delivery | 5 | 8.9 |
| Total=56 | ||
Tab. 3. Mode of delivery among the studied cases.
Tab. 4. shows that no significant differences according to mode of delivery regarding maternal (age& BMI) and fetal (gestational age& weight) characteristics.
| Variables | Vaginal (N=51) |
Cesarean (N=5) |
P-value |
|---|---|---|---|
| Maternal | |||
| Age (years) | 24.3 ± 4.4 | 24.4 ± 7.1 | ^0.980 |
| BMI (kg/m2) | 28.9 ± 3.2 | 28.4 ± 3.3 | ^0.728 |
| Fetal | |||
| Gestational age (weeks) | 38.6 ± 1.2 | 38.4 ± 1.5 | ^0.742 |
| Fetal weight (kg) | 3.1 ± 0.3 | 3.0 ± 0.5 | ^0.550 |
| ^Independent t-test, #Chi square test, & Fisher's Exact test | |||
Tab. 4. Comparison according to mode of delivery regarding maternal and fetal characteristics.
Tab. 5. shows that rupture of membranes was non-significantly more frequent in cases that delivered vaginally. Station, cervical dilatation, cervical effacement and angle of progression were significantly higher in cases that delivered vaginally.
| Variables | Vaginal (N=51) |
Cesarean (N=5) |
P-value |
|---|---|---|---|
| Rupture of membranes | 21 (41.2%) | 1 (20.0%) | §0.638 |
| Station | 0.0 (1.0−1.0) | -1.0 (-2.0−-1.0) | #0.006* |
| Cervical dilatation (cm) | 5.9 ± 1.4 | 4.6 ± 0.9 | ^0.044* |
| Cervical effacement (%) | 74.4 ± 10.5 | 64.0 ± 11.4 | ^0.040* |
| Angle of progression (°) | 108.9 ± 10.0 | 92.8 ± 5.5 | ^0.001* |
| ^Independent t-test. #Mann Whitney test. §Fisher's Exact test | |||
Tab. 5. Comparison according to mode of delivery regarding different predictors.
Tab. 6. shows that in predicting vaginal delivery; angle of progression had significant high diagnostic performance, station had significant moderate diagnostic performance, while cervical dilatation and cervical effacement had significant low diagnostic performance.
| Factors | AUC | SE | P | 95% CI | Cut off |
|---|---|---|---|---|---|
| Station | 0.857 | 0.075 | 0.009* | 0.710−1.000 | ≥0.0 |
| Cervical dilatation (cm) | 0.780 | 0.099 | 0.040* | 0.587−0.974 | ≥5.0cm |
| Cervical effacement (%) | 0.749 | 0.125 | 0.048* | 0.504−994 | ≥75.0% |
| Angle of progression (°) | 0.925 | 0.055 | 0.002* | 0.817−1.000 | ≥97.0° |
| AUC: Area Under Curve. SE: Standard Error. CI: Confidence Interval. *Significant | |||||
Tab. 6. Diagnostic performance of different vaginal delivery predictors.
Tab. 7. shows that in predicting vaginal delivery; angle of progression ≥97.0° had highest diagnostic characteristics, followed by station ≥0.0 station. Different cutpoints had their sensitivity& NPV higher than their specificity & PPV.
| Characters | Value | 95% CI | Value | 95% CI |
|---|---|---|---|---|
| Station ≥0.0 | Cervical dilatation ≥5 cm | |||
| Sensitivity | 80.4% | 66.9%–90.2% | 82.4% | 69.1%–91.6% |
| Specificity | 80.0% | 28.4%–99.5% | 60.0% | 14.7%–94.7% |
| DA | 80.4% | 67.6%–89.8% | 80.4% | 67.6%–89.8% |
| Youden's index | 60.4% | 23.7%–97.1% | 42.4% | 0.0%–86.5% |
| PPV | 97.6% | 87.4%–99.9% | 95.5% | 84.5%–99.4% |
| NPV | 28.6% | 8.4%–58.1% | 25.0% | 5.5%–57.2% |
| LR+ | 4.02 | 0.69–23.32 | 2.06 | 0.70–6.07 |
| LR- | 0.25 | 0.12–0.50 | 0.29 | 0.12–0.74 |
| LR | 16.40 | 1.65–163.21 | 7.00 | 1.02–48.16 |
| Kappa | 0.333 | 0.054–0.613 | 0.260 | 0.000–0.560 |
| Cervical effacement ≥75% | Angle of progression ≥97.0° | |||
| Sensitivity | 49.0% | 34.8%–63.4% | 92.2% | 81.1%–97.8% |
| Specificity | 80.0% | 28.4%–99.5% | 80.0% | 28.4%–99.5% |
| DA | 51.8% | 38.0%–65.3% | 91.1% | 80.4%–97.0% |
| Youden's index | 29.0% | 0.0%–66.7% | 72.2% | 36.3%–108.0% |
| PPV | 96.2% | 80.4%–99.9% | 97.9% | 88.9%–99.9% |
| NPV | 13.3% | 3.8%–30.7% | 50.0% | 15.7%–84.3% |
| LR+ | 2.45 | 0.42–14.47 | 4.61 | 0.80–26.65 |
| LR- | 0.64 | 0.38–1.07 | 0.10 | 0.03–0.28 |
| LR | 3.85 | 0.40–36.82 | 47.00 | 4.19–527.19 |
| Kappa | 0.089 | 0.00–0.225 | 0.568 | 0.234–0.902 |
| CI: Confidence Interval, YI: Youden's Index, DA: Diagnostic Accuracy, PPV: Positive Predictive Value, NPV: Negative Predictive Value, LR+: Positive Likelihood Ratio, LR-: Negative Likelihood Ratio, LR: Diagnostic Odds Ratio | ||||
Tab. 7. Diagnostic performance of vaginal delivery predictors’ cut-points.
Discussion
Trans-perineal ultrasonography (TPU) has been proposed as a valuable method for tracking labor progress and predicting birth mode [7]. One of the most promising sonographic findings, the angle of progression (AOP), has been demonstrated to be beneficial in predicting spontaneous vaginal birth and identifying the duration of the second stage of labor, which may be valuable in counseling and managing patient’s labor [8].
This diagnostic test accuracy prospective study was conducted at Ain Shams University Maternity Hospital starting from May 2020 to evaluate the role of measuring of the angle of progression (AOP) at the onset of the active phase of labor in prediction of spontaneous vaginal delivery in 56 full term primiparous women. Regarding mode of delivery; statistical analysis of our results showed that vaginal delivery was in more than 90% (51 vs. 5) of the studied cases and no significant differences according to mode of delivery were detected between study women regarding maternal age, BMI, fetal gestational age and fetal weight.
Brunelli et al. [8] study aimed to evaluate the role of fetal head station, as measured by the angle of progression, in the prediction of persistent occiput posterior position and the mode of delivery in the second stage of labor. They recruited 63 nonconsecutive series of women with posterior occiput position diagnosed by transabdominal ultrasound in the second stage of labor. For each woman, a transperineal ultrasound was performed to measure the angle of progression at rest. They compared the angle of progression between women who delivered fetuses in occiput anterior position and those with persistent occiput posterior position at delivery. They agreed with current study and stated that there was no significant difference between study women in parity and gestational age at delivery regarding mode of delivery.
Minajagi et al. [9] assessed the ability of the AOP measured by transperineal ultrasound to predict the mode of delivery in nulliparous women before the onset of labor. A prospective observational study was conducted at a single tertiary care hospital, on 120 nulliparous women who had presented to the antenatal clinic at ≥ 38 weeks of gestation but not in labor having fetal head station above 0. AOP was measured using transperineal ultrasonography and compared among the women having Caesarean section (CS) due to labor dystocia and vaginal delivery (VD). They agreed with current study and stated that among 120 nulliparous women, 92 (76.67%) women delivered vaginally and 28 (23.33%) underwent caesarean section due to labor arrest. No significant statistical difference between maternal age, body mass index (BMI) of the patients, GA at delivery (weeks) and birth weight (grams) was observed among the two groups.
Gillor et al. [10] assessed whether pre-labor measurement of the angle of progression (AOP) can assist in predicting a successful vaginal birth after cesarean in women without a previous vaginal birth. A prospective observational cohort study performed in a single tertiary center including women at term with a single previous cesarean delivery (CD), without prior vaginal births, who desire a trial of labor. Transperineal ultrasound was used to measure the AOP before the onset of labor. They disagreed with current study and stated that of the 111 women included in the study, 67 (60.4%) had a successful vaginal birth after CD. Comparisons between women revealed statistically significant differences clinically estimated fetal weight. A lower clinically estimated fetal weight (EFW) were shown to be more favorable with a VBAC that might be due to different study methods.
Pérez et al. [11] investigated the role of the angle of progression (AOP) in the prediction of vaginal delivery and establish a cut-off value. This prospective observational study was conducted at department of obstetrics and gynecology, university hospital Parc Taulí, Sabadell, Barcelona, Spain on 101 pregnant women were included in this prospective study. They were admitted in labor and had singleton cephalic presentations and full-term pregnancies. AOP was measured at admission time. They were in line with current study and stated that they did not observe significant differences in maternal age, maternal body mass index, gestational age at delivery, weight of newborns or neonatal outcomes between study women regarding mode of delivery. Spontaneous vaginal delivery occurred in 72 (71%) women, instrumental delivery in 19 (19 %) and cesarean section in 10 (10%).
Marsoosi et al. [6] investigated the role of the angle of progression (AOP) in the prediction of vaginal delivery. In this prospective study that was carried out at Shariati University Hospital (Tehran University of Medical Sciences), they followed 70 singleton pregnant women. AOP was measured at admission time and also at the beginning of the second stage immediately after digital examination. They agreed with current study and stated that sixty-five (92.9%) women had vaginal delivery (59 women spontaneously and six women with vacuum) and five (7.1%) women had cesarean section due to failure to progress to the second stage of labor. There were no significant differences between study women’s demographic characteristics regarding mode of delivery.
Regarding mode of delivery different predictors; statistical analysis of our results showed that rupture of membranes was non-significantly more frequent in cases that delivered vaginally. Station of fetal head, cervical dilatation, cervical effacement and angle of progression were significantly higher in cases that delivered vaginally. Angle of progression had significant high diagnostic performance; station of fetal head had significant moderate diagnostic performance, while cervical dilatation and cervical effacement had significant low diagnostic performance.
Brunelli et al. [8] study agreed with current study and stated that the angle of progression was found to be the only independent predictor that predict the mode of delivery (odds ratio, 0.849; 95% confidence interval, 0.775–0.0930; P<.001).
Minajagi et al. [9] agreed with current study and stated that a statistically significant higher mean value of AOP (100.7 ± 6.9°) was observed in females who delivered vaginally compared to the females having caesarean section (91.7 ± 6.1°) with a P-value < 0.01 indicating that AOP is wider in females delivering vaginally but they disagreed with current study and stated that station of fetal head was non-significantly different in cases that delivered vaginally that might be due to different study methods and women criteria.
Marsoosi et al. [6] agreed with current study and stated that in the first stage of labor, AUC for the prediction of vaginal delivery were 87.5% (95% confidence interval [CI], 77.9–97.1; P = 0.005) for the AOP and 85.5% (95% CI, 75.2–95.6; P = 0.009) for digital assessment of fetal station. Therefore, in the first stage of labor, AOP was a better indicator for the prediction of vaginal delivery compared with digital assessment of fetal station but they disagreed with current study and stated that in the second stage of labor, AUC for prediction of vaginal delivery were 90.2% (95%CI, 81–99.3; P=0.003) for AOP and 94.9% (95%CI, 89.1–100; P=0.001) for digital assessment of fetal station, so in the second stage of labor, digital assessment of fetal station showed a better prediction of vaginal delivery that might be due to different sample size in comparison with current study.
Regarding diagnostic performance of vaginal delivery predictors’ cut points; angle of progression ≥97.0° had highest diagnostic characteristics, followed by station ≥0.0 station followed by cervical dilatation ≥5 cm and cervical effacement ≥75%. Different cut points had their sensitivity& NPV higher than their specificity& PPV.
Brunelli et al. [8] study disagreed with current study and stated that the area under the receiver operating characteristics curve was 0.731 (95% confidence interval, 0.594–0.869) with an estimated best cutoff range of 121.5° (sensitivity of 72% and specificity of 67%). Women who underwent cesarean delivery had significantly narrower angle of progression than women who had a vaginal delivery (113.5°±8.1 vs 128.0°±10.7; P<.001). The area under the receiver operating characteristics curve for the prediction of cesarean delivery was 0.866 (95% confidence interval, 0.761–0.972) that might be due to different women criteria and study methods.
Solaiman et al. [12] evaluated the women’s acceptance to the transperineal ultrasound (TPUS) compared with digital transvaginal examination, and its ability to predict the mode of delivery in prolonged labor. This study was conducted at the obstetrics and gynecology emergency ward in a single tertiary center Hospital. The study was prospective and included 28 pregnant ladies in a prolonged active phase of first or second stages of labor and followed them till delivery. TPUS was used to measure the fetal head–perineum distance (FHPD) and the angle of fetal head descent. They disagreed with current study and stated that The area under the curve for predicting the vaginal delivery was 91% (95% CI, 59–99%) regarding the angle of fetal head progression. By using a cutoff value of 115°, 91% of the women delivered vaginally (sensitivity 93%, specificity 84%, positive predictive value (PPV) 87%, negative predictive value (NPV) 91%, positive likelihood ratio (LR) 6.06, and negative LR 0.08).
Minajagi et al. [9] agreed with current study and stated that the area under the ROC curve for the prediction of vaginal delivery was 0.818 (P < 0.001), cut off AOP value of 96° derived from the ROC curve predicted the possibility of vaginal delivery among nulliparous women. An AOP ≥ 96° measured before the onset of labor had a sensitivity of 85%, a specificity of 86%, a positive predictive value of 94.7%, and a negative predictive value of 54.53%, for the prediction of vaginal delivery at term in nulliparous women.
Gillor et al. [10] agreed with current study and stated that the median AOP was significantly narrower in women who eventually underwent a CD than in those who delivered vaginally. An AOP >980 (derived from a receiver operating characteristic curve) was associated with a successful vaginal birth after CD in 87.5% of women.
Chan et al. [13] assessed measuring of angle of progression by transperineal ultrasonography to predict successful instrumental and cesarean deliveries during prolonged second stage of labor. A prospective observational study was conducted among women with singleton term pregnancies with prolonged second stage of labor at Kwong Wah Hospital, Hong Kong, China. Transabdominal and transperineal ultrasonography were performed to determine fetal head position and AoP, respectively, both at rest and during uterine contraction with pushing. They disagreed with us and stated that median AoP was 153.0° in the instrumental group versus 139.0° in the cesarean group at rest (P<0.001) and 182.5° in the instrumental group versus 156.5° in the cesarean group during contraction (P<0.001). The best predictive cut-off AoP for successful instrumental delivery was 138.7° at rest (sensitivity 86.2%, specificity 51.9%) and 160.9° during contraction (sensitivity 87.1%, specificity 74.1%) that might be due to different study methods.
Pérez et al. [11] weren’t in line with current study and stated that the average angle of progression was 129,4° (SD 19.9). In vaginal deliveries, it was 131.9° compared to 107.5° in cesarean sections (p<0.001). There were no differences between spontaneous vaginal delivery (141.4°, SD15.4) and assisted vaginal delivery (142.4°, SD 13), however no instrumental deliveries were performed in current study. The ROC curve for the descent angle for vaginal delivery showed an area under the curve (AUC) of 0.85 (95% confidence interval [CI], 0.77-0.92). The value of the angle of descent that optimizes the curve was 125° (S 67.1%, E 100%). There was not a cesarean section with an angle greater than 125°.
Marsoosi et al. [6] differed from current study and stated that the AUC was estimated to be 90.2% (P=0.003) and based on this curve, the cut-off point of 113° was chosen to categorize the women into two groups: <113° and ≥113°. The sensitivity of this cut-off was 90.8% and the false positive value was 40% that might be due to different sample size in comparison with current study.
The strengths of current study were due to every effort was made to ascertain that all follow-up data were correct, and only complete information was included in data analysis. All clinical assessment, sonographic measurement, deliveries and assessment of study outcomes were done by the same team.
The limitations of current study were due to COVID 19 pandemic, relatively small sample size and digital and ultrasound examiners should be unaware of each other’s results.
Conclusion
In prediction of progress of spontaneous vaginal delivery in primiparous women, transperineal ultra-sonographic angle of progression with cutoff value ≥97.0° had highest predictive and diagnostic value, followed by station of fetal head ≥0.0 followed by cervical dilatation ≥5 cm and cervical effacement ≥75%. On the other hand rupture of amniotic membranes, maternal age, BMI, fetal gestational age and fetal weight had no significance in delivery progress prediction.
References
- Ciaciura-Jarno M, Cnota W, Wójtowicz D, et al. Evaluation of selected ultrasonography parameters in the second stage of labor in prediction mode of delivery. Ginekol Polska. 2016; 87(6):448-53.
- Molina FS and Nicolaides KH. Ultrasound in labor and delivery. Fetal Diagn Ther. 2010; 27(2): 61-67.
- Gillor M, Vaisbuch E, Zaks S, et al. Transperineal sonographic assessment of angle of progression as a predictor of successful vaginal delivery following induction of labor. Ultrasound Obstet Gynecol. 2017; 49(2): 240-45.
- Kameyama S, Sato A, Miura H, et al. Prediction of spontaneous vaginal delivery by transperineal ultrasound performed just after full cervical dilatation is determined. J Med Ultrason. 2016; 43(2): 243-48.
- Bibbo C, Rouse CE, Cantonwine DE, et al. Angle of progression on ultrasound in the second stage of labor and spontaneous vaginal delivery. Am J Perinatol. 2018; 35(04):413-20.
- Marsoosi V, Pirjani R, Mansouri B, et al. Role of ‘angle of progression’in prediction of delivery mode. J Obstet Gynaecol Res. 2015; 41(11): 1693-99.
- Kamel R, Negm S, Montaguti E, et al. Reliability of transperineal ultrasound for the assessment of the angle of progression in labor using parasagittal approach versus midsagittal approach. J Matern Fetal Neonatal Med. 2019: 1-6.
- Brunelli E, Youssef A, Soliman EM, et al. The role of the angle of progression in the prediction of the outcome of occiput posterior position in the second stage of labor. Am J Obstet Gynecol 2021; 81-89.
- Minajagi PS, Srinivas SB, Hebbar S. Predicting the mode of delivery by angle of progression (AOP) before the onset of labor by transperineal ultrasound in nulliparous women. Curr Women's Health Rev. 2020; 16(1):39-45.
- Gillor M, Levy R, Barak O, et al. Can assessing the angle of progression before labor onset assist to predict vaginal birth after cesarean?: A prospective cohort observational study. J Matern Fetal Neonatal Med. 2020: 1-8.
- Pérez SP, Seguer JJ, Pujadas AR, et al. Role of intrapartum transperineal ultrasound: angle of progression cut-off and correlation with delivery mode. Clin Obstet Gynecol Reprod Med. 2017; 3(4):1-4.
- Solaiman SA, Atwa KA, Gad AA, et al. Transperineal ultrasound of fetal head progression in prolonged labor: women’s acceptance and ability to predict the mode of delivery. Egypt J Radiol Nucl Med. 2020; 51(1):1-9.
- Chan VY, Lau WL, So MK, et al. Measuring angle of progression by transperineal ultrasonography to predict successful instrumental and cesarean deliveries during prolonged second stage of labor. Int J Gynaecol Obstet. 2019; 144(2):192-98.
Author Info
Mohamed Ahmed Elkadi, Maida Ramadan Ewida* and Ahmed Mohammed ZenhomCopyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.