Research - (2024) Volume 19, Issue 2
Received: 03-Jun-2024, Manuscript No. gpmp-24-143577; Editor assigned: 04-Jun-2024, Pre QC No. P-143577; Reviewed: 17-Jun-2024, QC No. Q-143577; Revised: 21-Jun-2024, Manuscript No. R-143577; Published: 28-Jun-2024
Background: It’s a miscarriage in which the fetus didn’t form or is no longer developing, but the placenta and embryonic tissues are still in uterus.
Objectives: To identify the risk factors that women miss abortions. To find out the association between Risk factors for missed abortion for women and demographic characteristics of women.
Methodology: Descriptive study design was conducted though out the present study for period from 25/November/2022 end 1/February/2023. The self-administrative report procedure and the designed questionnaire were used to gather data. Statistical Package for Social Science (IBM SPSS) version 25 was used to examine the data using both descriptive and inferential statistical techniques.
Results: The results of the study indicate that that most of sample within age group 20-30 years. Graduated from Bachelor's degree or above lived in urban, unemployed. (59.7) of the sample lose pregnancy in the second month of pregnancy. (50.6) from sample become pregnant for first time. (64.9) from sample had history of abprtion for first time. Most of the women with missed miscarriage were due to unknown causes and CMV and passive smoking. The results showed there is no relationship was statistically between missed miscarriage and sociodemograghic data.
Conclusion: In this study, the most common cause of missed miscarriage was CMV infection, as well as smoking, unknown causes, and surgical history. Statistically there is no relationship between facors of missed abortion and sociodemographic data.
Abortion; Pregnancy; Miscarriage
Early pregnancy complications are frequently associated with miscarriage; estimates place the number of miscarriages at 12%–15% of all pregnancies [1-5]. When an embryo or fetus dies before 12 weeks of gestation and remains in the uterus without a normal discharge, it is referred to as a missed abortion, also known as an untimely abortion [6,7]. Ten to twenty percent of spontaneous abortions are missed abortions, which are a specific kind of spontaneous abortion. Twenty to twenty percent of women have spontaneous abortions [8-10]. The incidence rate of missed abortions has clearly been rising in recent years [11-13], which has had a negative impact on patients' physical and mental well-being as well as their families' and society's happiness. The stop of fetal or embryonic development is a characteristic of missed abortion.. There is either no bleeding or very little, and the cervix is closed. Between 10 and 14 weeks of gestation, 2% of singleton pregnancies result in a missed abortion [14]. Undoubtedly, women who needed reproductive assistance suffered a great physical and psychological setback when their abortion was missed. Early detection of women who were at a high risk of missing an abortion was therefore essential and this might help provide a theoretical foundation for the implementation of clinical interventions to avoid missed abortions. Early pregnancy loss has been linked to fetal heart rate, yolk sac diameter, progesterone, Estradiol (E2), Gestational Sac Diameter (GSD), Crown-Rump Length (CRL), and human chorionic gonadotropin (HCG) [1,15,16]. Furthermore, it has been determined that the predictive value of mGSD-CRL for the outcome of early pregnancy in IVF treatments [17]. We therefore carried out this study in an effort to more thoroughly investigate, through statistical analysis, any potential high risk factors associated with the development of missed abortions. Ideally, this will greatly aid in identification and intervention.
Study population
Women who are 19-46 years old, pregnant, and have less than 20 weeks of gestation. All pregnant women who were included in study diagnosed as miss abortion. A cross-sectional study was done in the wards of Bint Al-Huda teaching Hospital in the city of Nasiriyah, Southern Iraq to determine the risk factors for missed abortion. For this investigation, a purposeful (non-probability) sample was chosen. To create a representative sample of (77) women who had missed abortions, the researcher employed a purposive sample. The sample was chosen by the researcher using the following criteria: Sample of study Inclusion (All Women at pregnant age, women with missed abortion only, women who were accepted to cooperated in this study). Exclusion criteria (women with non-missed abortion, women not agree to cooperative in this study).
Data collection
Data collected through face to face interview. Each subject completed a questionnaire survey which included personal data (age, residence, occupation, family income, and education level), reproductive data which included (number of pregnancies, number of time abortion, period of pregnancies), risk factors of missed abortion which included (history Previous chronic diseases, history of caesarean section, history of ectopic pregnancy, recurrent miscarriage, history of drug, history of smoking, passive of smoking, History of pelvic surgery, Any other disease, type of disease if present). It started from the 25/November/2022 end 1/February/2023, each interview took approximately (15-20) minutes to complete questionnaire form. The interviewing is carried out with each study sample who participated in the study.
Ethical consideration
Before beginning any interview, the researchers gave each woman a rundown of the study's objectives. Before any data was collected, each study sample gave their verbal consent. Women were given the assurance that the data would only be used for research and that the study would be anonymous, voluntary, and confidential.
Statistical analysis
The Statistical Package for the Social Sciences (SPSS version 24:0) was used to code the data and enter them into a computer for analysis. With regard to categorical variables, percentages and frequencies were used, and the Chi-square test was applied to demonstrate that mothers' knowledge, attitudes, and specific background information were significantly correlated. P<0.05 was employed as the threshold for significance.
Fig. 1. show distribution of sample (77) according to age of sample and Tab.1. shows the distribution of sample (77) according to level of education, residence occupation. As show in Tab. 2. highest of percent (39.0%) were in Bachelor, While (5.2%) Illiterate and Read Write from Education. About residence, highest of percent (74%) were in age Urban, While 20 (26%) Rural from residence. Regarding to occupation highest of percent (68.8%) Unemployed were in, While (31.2%) employed from occupation. The result of Tab. 3. show majority of pregnant women was in second month from pregnancy (59.7%), while (50.6%) had history of pregnant for first time and (64.9%) had history of abortion for first time. The result of Tab.4. show most of women had history for Passive smoking (55.8) and (50.6%) from sample found with CMV. (64.4%) found with unknown causes and (26%) had history of surgery and (24.6) found with placental thrombosis. Statistically revealed there is no association between socio-demographic data with risk factors for missed abortion.
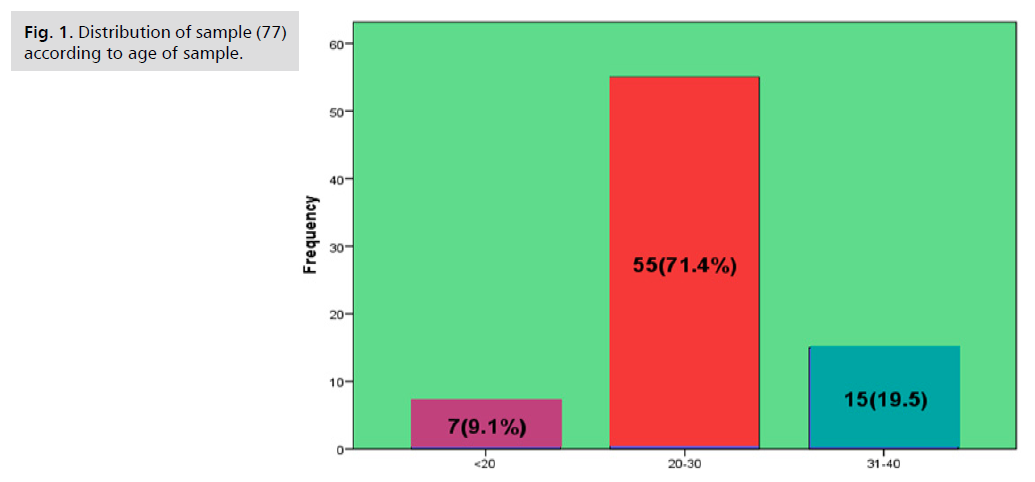
Fig 1. Distribution of sample (77) according to age of sample.
| Variables | F | % |
|---|---|---|
| Level of education | ||
| Ilitrate | 4 | 5.2 |
| Read and write | 4 | 5.2 |
| Primary school | 12 | 15.6 |
| Secondary school | 19 | 24.7 |
| Bachelor's degree or above | 30 | 39 |
| MSC and above | 8 | 10.4 |
| Residence | ||
| Rural | 20 | 26 |
| Urban | 47 | 74 |
| Occupation | ||
| Employed | 24 | 31.2 |
| Unemployed | 53 | 68.8 |
| Income | ||
| Enough | 28 | 36.4 |
| Not enough | 20 | 26 |
| Parely enough | 29 | 37 |
| Total=77 | ||
Tab. 1. Distribution of sample (77) according to level of education, residence, occupation and income.
| Reproductive data | F | % |
|---|---|---|
| Pregnancy period | ||
| First month | 6 | 7.8 |
| Second month | 46 | 59.7 |
| Third month | 25 | 32.5 |
| No. of pregnancy | ||
| First time | 39 | 50.6 |
| Second time | 12 | 15.6 |
| Third time | 11 | 14.3 |
| Fourth time | 8 | 10.4 |
| Fife time | 4 | 5.2 |
| More than six | 3 | 3.9 |
| No. of abortion | ||
| First time | 50 | 64.9 |
| Second time | 14 | 18.2 |
| Third time | 6 | 7.8 |
| Fourth time | 5 | 6.5 |
| Fifth time | 1 | 1.3 |
| More than sixth time | 1 | 1.3 |
Tab. 2. Distribution of sample (77) according to reproductive data.
| Risks factors for missed abortion | F | % |
|---|---|---|
| History of C/S | ||
| Yes | 20 | 26 |
| No | 55 | 71.4 |
| History of chronic diseases | ||
| Yes | 3 | 3.9 |
| No | 74 | 26 |
| History of drug | ||
| Yes | 3 | 3.9 |
| No | 74 | 96.1 |
| History of ectopic pregnancy | ||
| Yes | 0 | 0 |
| No | 77 | 100 |
| History of active smoking | ||
| Yes | 0 | 0 |
| No | 77 | 100 |
| Passive of smoking | ||
| Yes | 43 | 55.8 |
| No | 34 | 44.2 |
| Recurrent abortion | ||
| Yes | 9 | 11.7 |
| No | 68 | 88.3 |
| Surgical history | ||
| Yes | 0 | 0 |
| No | 77 | 100 |
| Any other disease | ||
| Yes | 1 | 1,3 |
| No | 76 | 98,7 |
| Rh incompatible | ||
| Yes | 8 | 10.4 |
| No | 69 | 89.5 |
| Type of disease | ||
| CMV | 39 | 50.6 |
| Toxoplasmosis | 7 | 9.1 |
| Placental thrombosis | 19 | 24.6 |
| Cervical incompetence | 1 | 1.3 |
| Un know causes | 50 | 64.9 |
| Twin pregnancy | 1 | 1.3 |
| Chronic disease | 1 | 1.3 |
| Sub placental hemorrhage | 2 | 2.6 |
| Placenta abruption | 2 | 2.6 |
| Vit. D3 deficiency | 2 | 2.6 |
| Methotrexate drug | 1 | 1.3 |
Tab. 3. Distribution of sample (77) according to risk factor for missed abortion.
| Socio-demographic variable | Value | df | P-value |
|---|---|---|---|
| Age | 34.932 | 30 | 0.245 |
| Residence | 16.580 | 15 | 0.345 |
| Level of education | 81.185 | 75 | 0.293 |
| Monthly income | 31.46 | 30 | 0.393 |
| Occupation | 14.470 | 15 | 0.490 |
Tab. 4. Association between socio-demographic data with risks factors for missed abortion.
Sociodemographic characteristics
Missed abortion, normally presenting without symptoms of threatened abortion such as abdominal pain and vaginal bleeding, was a kind of spontaneous abortion, which were frequently diagnosed using ultrasonography. In this study, we analyzed the data of 77 women diagnosed with missed abortion in order to fully establish the possible risk factors for missed abortion, and provide evidence for early identification and intervention for patients with high risk of missed abortion. Finding of this study indicate the highest percentage (71.4%) of study sample are at age (20- 30) years from age, as shows in Fig. 1. In previous studies, it was believed that advanced Age was found to be a significant risk factor for missed abortions, which may be related to the corpus luteum and ovarian function declining with age (19-20). But earlier research also showed that becoming older did not significantly increase the incidence of spontaneous abortion [18-20]. Of them, 26% were rural residents and 74% were urban residents. We made pregnancy termination hypotheses while accounting for women's regional dispersion. Women in urban areas have more abortions than in rural areas. Socially disorganized villages, neighbourhoods characterized by socioeconomic deprivation, may offer few of the maternal and If contextual variables at the district level contribute to the risk of termination pregnancy, there are reproductive health supports that normally assist mothers in developing the physical, social, and emotional competences needed to attain their full potential for health and well-being. Regarding education, (39%) of study participants had a bachelor's degree or higher. More precisely, compared to women with less education, educated women are less likely to have terminated a pregnancy in the past. These findings contradict those of another study that suggested women with greater levels of education are more likely to undergo an induced abortion [21]. In terms of occupation, (68.8%) of the sample did not have a job, whilst 24 (31.2%) did. This information contradicts a study that suggested there could be a number of reasons why working women are more likely than non-working women to have their pregnancies terminated [22]. Of the sample, (37%) had a sufficient monthly income. This result conflicts with a prior study that found women in greater socioeconomic status had a higher likelihood of terminating their pregnancies [23].
Reproductive data
This part will discuss reproductive data in women with missed abortion relying on the statistical results found by researchers in the studies. Finding of study show majority of women in second month from Pregnancy become pregnant for first time with history of abortion one time. This data agree with study who revealed that in the first trimester was a high risk factor for missed abortion active early pregnancy [18].
Risk factors
Also in this study we find majority of women had history of passive of smoking, majority of women had unknown cause, CMV, history of surgery and placental thrombosis from sample. Statistically revealed there is no association between socio-demographic data with risk factors for missed abortion as show in Tab. 3. In the end, the information about missed abortion continues to be completely unclear. Finally, we hope that this research will benefit researchers in conducting future studies on missed abortion.
The results of the study showed that the most of the study sample had unknown causes and that the majority of the women who missed abortions were between the ages of 20 and 30. Were bachelor's degree holders who thought the model response was suitable? The majority of the sample's participants were unemployed, and the majority of the women were pregnant or in the second month of their pregnancies. According to the findings, there is no statistically significant correlation. The correlation of socio-demographic information with reproductive information and risk variables showed that there is no statistically significant correlation between socio-demographic information and missed abortion.
Complete prenatal care and care is the best way to prevent pregnancy complications and problems. These include (not smoking, consuming caffeine, drinking alcohol, not to be exposed to environmental waste, early diagnosis and appropriate treatment of infections. Many abortions occur due to chronic diseases that affect the pregnant mother, so they must be prevented by diagnosing and treating them before pregnancy. When the mother encounters difficulties in maintaining the pregnancy, it is accompanied by the appearance of signs such as (absent of signs of pregnancy). This means that there is a possibility of missed abortion, but it is not a confirmation of a miscarriage. Therefore, a pregnant mother who has any of the signs or symptoms associated with the threat of miscarriage should see her specialist doctor immediately.
The authors express particular thanks to doctors and staff in Bint Al-Huda teaching Hospital for our assist. Finally, we thank all women that participate to complete this study.
(A) Study Design · (B) Data Collection . (C) Statistical Analysis · (D) Data Interpretation · (E) Manuscript Preparation · (F) Literature Search · (G) No Fund Collection
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.