Research Article - (2022) Volume 17, Issue 2
Received: 15-Mar-2022, Manuscript No. gpmp-22-57304; Editor assigned: 18-Mar-2022, Pre QC No. P-57304; Reviewed: 21-Mar-2022, QC No. Q-57304; Revised: 28-Mar-2022, Manuscript No. R-57304; Published: 04-Apr-2022
Objectives: Cesarean section (CS) rate has increased, which much more highlighted the importance of post-CS pain control. Among various post-CS-pain controls, we here attempted to determine which is better, the ultrasound-guided trans-muscular quadratus lumborum nerve block (QLB) vs. transversus abdominis nerve block (TAP) during CS and in the early postoperative period regarding pain relief, comfort, and respiratory functions.
Patients and Methods: This prospective study was conducted at Ain Shams University hospitals for 6 months from June to December 2020. Participants were total 50 patients undergoing elective CS, who were divided into two groups (n=25; each); group QLB and TAP. Group QLB: bilateral ultrasound-guided QLB; Group TAP: bilateral ultrasound- guided TAP; with both groups having received each (QLB or TAP) after induction of regional anesthesia (0.25% bupivacaine (25ml) + normal saline (1ml)).
Results: QLB, compared with TAP, showed the followings: significantly lower total NSAID dose, non-significantly less frequent opioid consumption, significantly shorter onset of mobilisation, and non- significantly less frequent nausea and vomiting. Postoperative allergic, psychogenic and local complications were not observed.
Conclusion: QLB might be effective than TAP at CS.
Women with Cesarean delivery present a unique set of challenges for anesthetists after surgery. These motivated women want to be alert, relaxed, and mobile to take care of their children. Opioids are initially required as part of a multimodal analgesic regimen to achieve effective analgesia. However, opioids are associated with dose- dependent adverse effects, including nausea vomiting, pruritus, sedation, and respiratory depression [1-2].
The transverse abdominis plane (TAP) block is a peripheral nerve block designed to anesthetize the nerves supplying the anterior abdominal wall (T6 to L1). It was first described in 2001 by Rafi [3].
TAP block is an efficient way of providing postoperative analgesia in patients with midline abdominal wall incisions. Its analgesic efficacy over the first 48 postoperative hours following cesarean delivery has been confirmed [2].
Blanco is the first one described QL block in 2007. The main advantage of QL Block compared to the transverse abdominal plane (TAP) block is the extension of the local anesthetic agent beyond the transversus abdominis plane to the thoracic paravertebral space. Greater spread of local anesthetic agents may result in extensive analgesia and prolonged action of the local anesthetic solution injected. Previous studies have shown that both TAP block and QL Block may reduce opioid requirements in the postoperative period. However, studies comparing trans-muscular quadratus lumborum and transversus abdominis plane blocks are limited in number [4].
This work aims to study the analgesic efficacy of ultrasound-guided bilateral trans-muscular quadratus lumborum block (QLB) compared with bilateral transversus abdominis plane (TAP) block on postoperative period regarding pain control, total opioid given in the first 24-hour post-operative, VAS score and first time to ask for analgesia in patients undergoing Cesarean section under spinal anesthesia.
After approval of the anesthesiology department and scientific and ethical committees, this prospective randomized clinical trial study was conducted in Ain Shams University Hospitals.
Fifty pregnant female patients scheduled for elective cesarean section, under spinal anesthesia were included in this study. The patients' age was ranged from 21 to 45 years and with the American Society of Anesthesiologists (ASA) Class-I and II.
At the end of the surgery, patients were randomized using a random number table and the use of a closed envelopes technique to receive either quadratus lumborum block (Group QLB), or TAP (transversus abdominis plane) block (Group TAP) each group constitutes of 25 patients.
Group TAP: bilateral injection of 0.25% bupivacaine (25ml) with normal saline (1ml) between the internal oblique and transversus abdominis muscles.
Group QL Block: Bilateral injection of 0.25% bupivacaine (25ml) with normal saline (1ml) at the posterior border of the quadratus lumborum muscle.
Exclusion Criteria: Systemic diseases as HTN, renal ds, liver ds, cardiac ds, DM. (Vulnerable groups with vasculopathy which can exacerbate occurrence of hematoma & abscess). HTN (Vasculopathy which can lead to hematoma). Cardiac disease (Vasculopathy on anticoagulant which can lead to hematoma). DM (decrease systemic and local immunity which can lead to abscess at injection site). Liver disease (defective clotting factors). History of allergy to the medications used in the study. American Society of Anesthesiologists (ASA) class ≥ III. Patients further refusal to participate in the study. Contraindications to regional anesthesia (including coagulopathy and local infection. Psychiatric disorder. Morbid obesity (BMI: >40kg/m2). Pregnant women going for an emergency Cesarean section.
Sample Size: Sample size will be calculated using STATA program, setting the type-1 error (α) at 0.05 and the power (1-β) at 0.8.Result from previous study Oksuz et al. [5] showed that the postoperative pain score at 2 hour will be 0.12± 0.33 in QL block versus 0.64±0.7 in TAP block. Calculation according to these values produced a sample size of 25 cases per group A and B taking in consideration 20% drop out rate.
Preoperative Settings: Routine preoperative assessment was done to all patients before operation, including history, clinical examination, and laboratory investigations (complete blood picture, kidney function tests, liver function tests, prothrombin time, and partial thromboplastin time). All patients were informed about the study design and objectives as well as tools and techniques. Informed consent was signed by every patient before inclusion in the study. All patients were informed about the analgesic regimen and were instructed on how to express pain intensity with the use of the Visual Analogue Scale (VAS); 10 cm marked line in which 0=no pain, 10 cm = the worst imaginable pain.
Monitoring: Basic monitoring including, electrocardiogram (ECG), pulse oximetry (SpO2), non- invasive blood pressure (NIBP, was applied to all patients, starting before anesthesia till the end of surgery and then recovery. On arrival of the patients to the operative room, electrocardiography, non-invasive blood pressure, and pulse oximetry had been applied. Baseline parameters such as systolic blood pressure (SBP), diastolic blood pressure (DBP), heart rate (HR), and oxygen saturation (SpO2) had been also recorded. Intravenous (IV) line was inserted and IV lactated Ringer had been started. For the three groups, spinal anesthesia was performed using a spinal needle of 25-G under complete aseptic conditions, All participants had received spinal anesthesia using hyperbaric 0.5% bupivacaine 12 mg and fentanyl 25 µg. Intraoperative antiemetics were not be routinely administered, but if required, ondansetron 4 mg I.V. was to be the first line. At the end of surgery (skin closure) either block was performed under complete aseptic precautions using an ultrasound machine with a high-frequency linear probe covered with sterile sheath (Sonoscape® SSI 6000, Chinawith12 6 MHz high-frequency linear probe) and 100 mm needle (B- Braun Medical Inc., Bethlehem, PA, USA). The 1st group received the TAP block, and the 2nd group received the QL Block. Then, the patients were transferred to the PACU.
Ultrasound-guided Transversus Abdominis Plane (TAP) Block Technique: The probe was located between the iliac crest and the lower costal margin in the anterior axillary line at the level of the umbilicus, and the layers of the abdominal wall were identified (external oblique, internal oblique, and transverse abdominis muscles). The in-plane technique was used, and the tip of the needle was inserted between the internal oblique and transverse abdominis muscles. After negative aspiration, (0.25% bupivacaine (25ml) with normal saline (1ml) per side) was injected without exceeding the toxic dose of 3 mg/kg. The same technique was performed on the other side.
Ultrasound-guided Trans-muscular Quadratus Lumborum (QL) Block Technique: The patients were positioned supine with a lateral tilt to perform the block, and the transducer was placed at the level of the anterior superior iliac spine and was moved cranially until the three abdominal wall muscles were identified. The external oblique muscle was followed postero-lateral until its posterior border had been visualized (hook sign), leaving underneath the internal oblique muscle, like a roof over the QL muscle. The probe was tilted down to identify a bright hyperechoic line that represents the middle layer of the thoracolumbar fascia. The needle was inserted in- plane from anterolateral to posteromedial. The needle tip was placed between the thoracolumbar fascia and the QL muscle, and after negative aspiration, the correct position of the needle had been proved by injection of 5 mL of normal saline to confirm the space with a hypoechoic image and hydrodissection. An injection of (0.25% bupivacaine (25ml) with normal saline (1ml) per side) was applied without exceeding the toxic dose of 3 mg/kg and the same technique was performed on the other side.
Postoperative settings: After the patient was discharged from the operating room, the visual analogue scale (VAS) was used to assess the postoperative pain; If VAS ≥3 postoperatively, IV increment of pethidine 50 mg diluted in 5 ml saline was given. IF side effects including, hypotension (systolic arterial pressure <90 mmHg), arrhythmia, bradycardia (HR <50 beats/min), nausea or vomiting, or any other complications, were to be recorded. Atropine 0.5 mg would be given in response to bradycardia, 20 ml per kg lactated Ringer would be given in response to hypotension.
If local anesthetic toxicity occurred:
Resuscitation: Standard procedures and supportive care. If there is evidence of cardiotoxicity, immediate intubation and ventilation is necessary to prevent hypoxaemia, hypercarbia and acidosis. Treat ventricular dysrhythmias with sodium bicarbonate (1 – 2mmol/kg up to 100mmol) IV every 1-2 minutes until perfusing rhythm; can use amiodarone; AVOID calcium channel blockers, beta blockers, local anaesthetics. Treat seizures with benzodiazepines. Treat hypotension with intravenous normal saline 20mL/kg followed by inotropes if required; AVOID vasopressin. Intravenous lipid emulsion (see below – antidotes). Recovery from local-anaesthetic induced cardiac arrest may take > 1hr [6].
Data collection
Heart rate (HR) and systolic (SBP) and diastolic blood pressure (DBP) will be measured upon arrival to the PACU and after 30 min, then every hour if the patients remain in the PACU. In the surgical ward, vital signs (HR, SBP, DBP) as well as pain intensity will be assessed every 2 hours during the first 6 hours and then every 6 hours there for 24 hours postoperatively. All patients will receive ketorolac 30 mg IM every 8h. It will start immediately postoperatively in the PACU. The total doses of pethidine used postoperatively per patient (rescue analgesia) were recorded for 24 h. The severity of postoperative pain was assessed using the Visual Analogue Scale (VAS will be evaluated postoperatively and every 2 hours during the first 6 hours and then every 6 hours for the next 24 hours postoperatively). Duration of postoperative analgesia (the time from recovery to the first given dose of pethidine). The number of patients needed rescue analgesia.
Statistical methods
The collected data were coded, tabulated, and statistically analyzed using IBM SPSS statistics (Statistical Package for Social Sciences) software version 22.0, IBM Corp., Chicago, USA, 2013. Quantitative normally distributed data described as mean±SD (standard deviation) after testing for normality using Shapiro-Wilk test, then compared using independent t-test if normally distributed. Qualitative data described as number and percentage and compared using Chi square test and Fisher’s Exact test for variables with small expected numbers. The level of significance was taken at P value < 0.050 is significant, otherwise is non-significant.
Tab. 1. shows that there is no significant differences between the studied groups regarding demographic characteristics; maternal age, BMI and parity as well as neonatal gestational age and operation duration. Tab. 2. Shows postoperative pain perception at hours 2, 4, 6, 8, 12 and 24 was significantly lower in QL Block group than TAB group. Tab. 3. shows time to first rescue analgesia was significantly longer in QL Block group than TAB group. Tab. 4. shows total NSAID dose was significantly lower in QLB group than TAB group. Tab. 5. and Fig. 1. shows opioid consumption was non-significantly less frequent in QL Block group than TAB group. Tab. 6. shows onset of mobilisation was significantly shorter in QL Block group than TAB group. Tab. 7. shows that postoperative nausea and vomiting were non-significantly less frequent in QL Block group than TAB group. Postoperative allergic, psychogenic and local complications not recorded in the studied groups.
| Variables | Measures | QLB (N=25) | TAB (N=25) | P-value |
|---|---|---|---|---|
| Age (years) | Mean ± SD | 25.8 ± 2.4 | 25.4 ± 2.6 | ^0.648 |
| Range | 21.0 – 31.0 | 21.0 – 30.0 | ||
| BMI (kg/m2) |
Mean ± SD | 27.1 ± 1.3 | 27.5 ± 1.4 | ^0.367 |
| Range | 25.1 – 29.4 | 25.0 – 29.5 | ||
| Parity | Nulli | 10 (40.0%) | 10 (40.0%) | #0.999 |
| Parous | 15 (60.0%) | 15 (60.0%) | ||
| GA (weeks) |
Mean ± SD | 39.3 ± 0.9 | 39.2 ± 0.9 | ^0.510 |
| Range | 38.0 – 41.0 | 38.0 – 41.0 | ||
| Operation duration (minutes) | Mean ± SD | 43.1 ± 3.4 | 43.2 ± 4.5 | ^0.944 |
| Range | 37.0 – 49.0 | 35.0 – 53.0 |
Tab. 1. Demographic characteristics of the studied groups.
| Time | Measures | QLB (N=25) | TAB (N=25) | ^P-value | Effect size Mean ± SE 95% CI |
|---|---|---|---|---|---|
| Hour-2 | Mean ± SD | 0.6 ± 0.5 | 2.0 ± 1.4 | <0.001* | -1.4 ± 0.3 |
| Range | 0.0 – 1.0 | 0.0 – 4.0 | -2.0 – -0.9 | ||
| Hour-4 | Mean ± SD | 0.6 ± 0.5 | 2.2 ± 1.5 | <0.001* | -1.6 ± 0.3 |
| Range | 0.0 – 1.0 | 0.0 – 4.0 | -2.3 – -1.0 | ||
| Hour-6 | Mean ± SD | 3.4 ± 0.5 | 3.9 ± 0.7 | 0.006* | -0.5 ± 0.2 |
| Range | 3.0 – 4.0 | 3.0 – 5.0 | -0.8 – -0.1 | ||
| Hour-8 | Mean ± SD | 2.5 ± 0.5 | 3.3 ± 1.1 | 0.003* | -0.8 ± 0.2 |
| Range | 2.0 – 3.0 | 2.0 – 5.0 | -1.2 – -0.3 | ||
| Hour-12 | Mean ± SD | 2.2 ± 0.9 | 3.0 ± 0.9 | 0.004* | -0.8 ± 0.3 |
| Range | 1.0 – 4.0 | 2.0 – 4.0 | -1.3 – -0.3 | ||
| Day-24 | Mean ± SD | 0.6 ± 0.5 | 2.2 ± 1.5 | <0.001* | -1.6 ± 0.3 |
| Range | 0.0 – 1.0 | 0.0 – 4.0 | -2.3 – -1.0 |
Tab. 2. Postoperative pain percep- tion (VAS-10) among the studied groups.
| Measures | QLB (N=25) | TAB (N=25) | ^P-value | Effect size Mean ± SE 95% CI |
|---|---|---|---|---|
| Mean ± SD | 6.6 ± 1.0 | 4.7 ± 1.6 | <0.001* | 1.9 ± 0.4 |
| Range | 5.0 – 8.0 | 2.0 – 7.0 | 1.2 – 2.7 |
Tab. 3. Time to first rescue anal- gesia (hours) among the studied groups.
| Measures | QLB (N=25) | TAB (N=25) | ^P-value | Effect size Mean ± SE 95% CI |
|---|---|---|---|---|
| Mean ± SD | 47.2 ± 9.8 | 59.2 ± 15.8 | 0.002* | -12.0 ± 3.7 |
| Range | 40.0 – 60.0 | 40.0 – 80.0 | -19.5 – -4.5 |
Tab. 4. Total NSAID dose (mg) among the studied groups.
| Findings | QLB (N=25) | TAB (N=25) | §P-value | Effect size Relative risk 95% CI |
|---|---|---|---|---|
| Needed | 0 (0.0%) | 1 (4.0%) | 0.999 | Not applicable |
| Not needed | 25 (100.0%) | 24 (96.0%) |
Tab. 5. Opioid consumption among the studied groups.
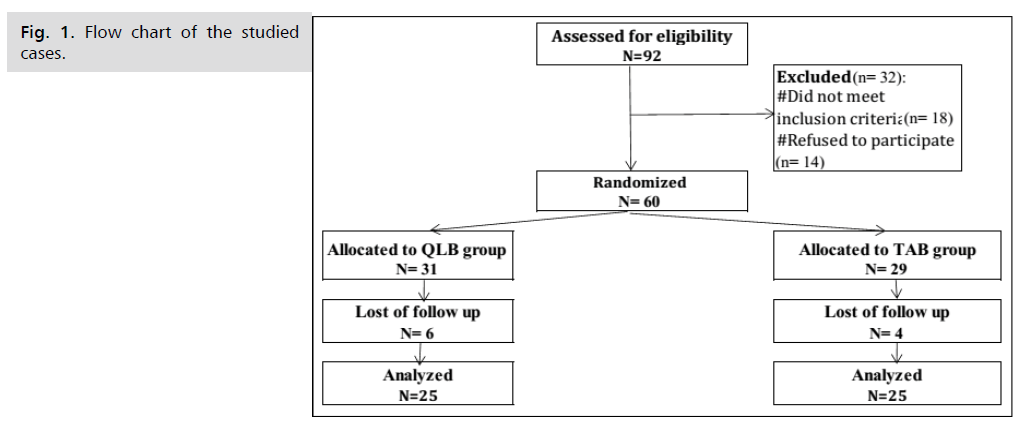
Fig 1: Flow chart of the studied cases.
| Measures | QLB (N=25) | TAB (N=25) | ^P-value | Effect size Mean ± SE 95% CI |
|---|---|---|---|---|
| Mean ± SD | 2.8 ± 0.9 | 4.2 ± 1.0 | <0.001* | -1.4 ± 0.3 |
| Range | 1.0 – 4.0 | 2.0 – 6.0 | -1.9 – -0.9 |
Tab. 6. Onset of mobilisation (hours) among the studied groups.
| Complications | QLB (N=25) | TAB (N=25) | §P-value | Effect size Relative risk 95% CI |
|---|---|---|---|---|
| Nausea | 1 (4.0%) | 3 (12.0%) | 0.609 | Not applicable |
| Vomiting | 0 (0.0%) | 1 (4.0%) | 0.999 | Not applicable |
| Allergic | 0 (0.0%) | 0 (0.0%) | Not applicable | Not applicable |
| Psychogenic | 0 (0.0%) | 0 (0.0%) | Not applicable | Not applicable |
| Local | 0 (0.0%) | 0 (0.0%) | Not applicable | Not applicable |
Tab. 7. Postoperative complications among the studied groups.
Many modalities are available for the control of postoperative pain, which includes systemic or neuraxial opioids, NSAIDs, and epidural analgesia. These methods have their own complications [2,7-9].
So our goal to achieve postoperative satisfaction regarding the pain with the least side effect as associated with opioid (vomiting up to respiratory depression) and so by achieving well pain control the mother then can take care of her child and herself and move early postoperatively [2].
In the past few years, the transversus abdominis plane (TAP) block has been increasingly used for postoperative pain relief after CS surgery. As a part of a multimodal analgesic regimen, the TAP block results in less analgesic consumption and less pain after CS surgery in comparison with the usual opioids alone [10].
The main advantage of QL Block compared to the transverse abdominal plane (TAP) block is the extension of the local anesthetic agent beyond the transversus abdominis plane to the thoracic paravertebral space. Greater spread of local anesthetic agents may result in extensive analgesia and prolonged action of the local anesthetic solution injected. Previous studies have shown that both TAP block and QL Block may reduce opioid requirements in the postoperative period [4].
Quadratus lumborum (QL) block is an inter-fascial block providing effective visceral and somatic analgesia rather than TAP block [11].
During this study, ninety two patients were assessed for eligibility and 50 patients were included in the study (25 in each group). Of all eligible patients, 18 patients were excluded from the study based on the inclusion criteria and 14 patients refused to participate in of the study.
Ultimately, the analysis was based on the data of 25 patients in TAP block group and 25 in the QL block group.
This exploratory study was conducted to explore the analgesic efficacy of the ultrasound-guided transmuscular quadratus lumborum block (QLB) compared to the transversus abdominis plane (TAP) post-cesarean section period in terms of pain relief, comfort and improved respiratory function.
In this study, the effect of quadratus lumborum block and transversus abdominis plane block result of decreased incidence and severity of postoperative pain (VAS) resulting in a decrease in incidence and degree of sedation and opioid total requirement.
The present study showed that the quadratus lumborum block was more efficient than the tansversus abdominis plane block. The first rescue for analgesia (pethidine), total pethidine consumption and pain scores (visual analog scale) indicated that the superiority of the QL block technique affected the TAP block technique. The patients of group TAB had higher pain scores and were the first to ask for rescue analgesia; therefore, they had highest total pethidine consumption in the first 24 hours postoperatively in comparison to patients of group QL Block.
The results of the current study were consistent with the conclusion of Blanco and his colleagues [4] found that the quadratus lumborum block produces more prolonged analgesia than the TAP block. Besides, their results have shown that the adoption of QLB as a default technique may significantly reduce opioid use and adverse effects following cesarean delivery. It also agreed with the conclusion of Verma and his coworkers [11] in 2019 that QLB block had an efficacy advantage in blocking visceral and somatic pain so mimic spinal anesthesia and prolonged anesthesia up to 72 hours after a cesarean section of the TAP block.
Also, Öksüz and his colleagues [5] compared QL and TAP blocks for postoperative pain relief following lower abdominal surgery in children. The results of their study showed that the QL block provided more effective pain relief compared to the TAP block and did not have adverse effects.
The case report, conducted by Elsharkawy and his colleagues compared the previous QL block with the TAP block in a patient undergoing subtotal colectomy through a midline incision extending from above the umbilicaus to the pubic symphysis. This patient experienced a consistent sensory blockage in the distribution of the corresponding dermatomes for approximately 48 hours on the side of the QL block.; However, the TAP block on the contra- side did not cover the entire length of the incision. It has been shown that QL block can cause sensory blockage and analgesia along mid-and lower thoracic dermatomes, and can prolong analgesia in the case of appropriately selected abdominal surgery [12].
The results of the current study were agreed with the conclusion of Murouchi and his colleagues [13]. They found that the effect of a single injection QL block with 20 mL of ropivacaine could spread to T7-T12 and could last for about 24 hours, which means that the duration of analgesia was way longer for QL block than for TAP block when applied to laparoscopic ovarian surgery.
In his case report about ultrasound-guided quadratus lumborum block as a postoperative pain control in laparotomy, Kadam [14] Reduced pain scores and the opioid requirement for duodenal tumor excision within the first 24 hours post-laparotomy. However, Opioid use was similar to the first day following a continuous TAP block for major abdominal surgery with supraumbilical or infraumbilical incisions; this study was performed on twenty patients with Kadam and Field [15]. The similarity between the case report and the study in the day-one opioid consumption maybe because he compared one patient who was given a single-injection quadratus block to ten patients who received continuous TAP block.
Also in a study conducted by Kupiec and her colleagues on 88 women going for CS showed that 1st group who received TAP block guided by ultrasound result a significant decrease in Tramadol take and even less pain intensity which measured by VAS score in the first 12 hours postoperative in comparison to the 2nd group which manged by Patient Controlled Analgesia method but there were no significant differences between two groups regarding hemodynamics changes [16].
On the other side, Canakci and his colleagues studied the comparison between the epidural anesthesia versus TAP block on 80 females undergoing elective CS concluded the visual analog scale (VAS) scores of The epidural anesthesia group were significantly lower compared to that of the TAP group in the first 24 hours postoperative and they consider the golden standard to achieving post-cesarean analgesia
[17] and Aditianingsih and his colleagues studied the analgesic effect of repeated Quadratus Lumborum block versus continuous epidural analgesia after laparoscopic nephrectomy regarding the total dose of opioid and hemodynamics changes and postoperative nausea and vomiting and showed the QLB had the same total amount of opioids versus epidural analgesia needed to control the pain in 65 patients in the first 24 hours postoperative and no difference in the incidence of postoperative nausea and vomiting compared to the continuous epidural analgesia [18].
Belavy et al. [2] results were agreed with our results in that there was a trend towards less nausea in the active group with no difference in patients reported vomiting.
The strength points of this study is that it evaluated the postoperative pain which is very common in practice as pain relief not only relieves the physical distress of the mother but also improves the quality of care of the newborn., the randomized design, and the objective measurement of postoperative pain.The limitations of the study are worthy of mention including relatively smaller sample size relative to the previous studies, not being a multicentric study and this represents a significant risk of publication bias .
Also, some important outcomes were missing, such as differentiation between visceral and somatic pain, effect of TAP block on breastfeeding, and its effect on the incidence of chronic pain after cesarean delivery. Further limitations include differences in TAP block technique and doses of local anaesthetics used.
Quadratus lumborum block was the most effective technique in providing analgesia after cesarean section without associated hemodynamic instability in comparison to transversus abdominis plane block and even more time covering to rescue opioid. The block has opioid-sparing effects, reduces antiemetic use, and improves satisfaction with pain relief.
(A) Study Design · (B) Data Collection . (C) Statistical Analysis · (D)Data Interpretation · (E)Manuscript Preparation· (F) Literature Search · (G) Funds Collection
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.