Case Report - (2022) Volume 17, Issue 4
Primary ovarian retroperitoneal serous cystadenoma primarily diagnosed as ovarian torsion managed laparoscopically: Case Report
Nada Alayed1, Khalid Akkour1, Rana Al Ohaly1, Fady Alakeel2, Amany Abuhassan2, Ahmed Sherif Abdel Hamid AS1,3* and Mohamed Mahmoud Abdelaziz4Received: 09-Nov-2022, Manuscript No. gpmp-22-79688; Editor assigned: 11-Nov-2022, Pre QC No. P-79688; Reviewed: 20-Nov-2022, QC No. Q-79688; Revised: 23-Nov-2022, Manuscript No. R-79688; Published: 29-Dec-2022
Abstract
Introduction: The site of pathology is the unique about this case, ovary is an intraperitoneal structure, in this case the ovary was retroperitoneal and there was ovarian serous cystadenoma (1st case in literature), Serous cystadenoma arises retroperitoneal but to the best of our knoweldge we didnot find any cases in literature describing primary Ovarian serous cystadenoma.
Case presentation: The patient is virgin, 26 years old presented with history of ovarian cyst of 3-month duration and acute lower abdominal pain, on examination there was tender lower abdomen, ultrasound was done revealing ovarian cyst with limited study of abdominal doppler. Provisional diagnosis of ovarian torsion that was managed laparoscopically by retroperitoneal cyst adenectomy clarifying a very unusual site of the ovary.
Conclusion: Take home lesson MRI should be mandatory for any ovarian cyst in Virgin patients and laparoscopists must have experience with dangerous retroperitoneal space to avoid injury of ureter and great vessels
Keywords
Retroperitoneal; Ovarian serous cystadenoma; Laparoscope; Ovarian torsion; Case report
Introduction
Primary retroperitoneal serous cystadenoma is quite uncommon with only very small number of cases reported in the literature. The cause of such cysts is not well understood, but theoretically they may represent embryological remnant of the urogenital system along with epithelial and mesothelial tissues [1].
Recurrent ovarian serous cystadenoma are also rare and sometimes present in ovarian remnants after salpingo-oophorectomy [2]. In this case the patient has a primary ovarian serous adenoma.
Case Presentation
A patient 26 years old, virgin, single presented to ER complaining of severe lower abdominal colicky pain of 2 days duration. The patient gave a history that she had ovarian cyst of 3-month duration but the primary concern and fear of the patient not to remove ovary for fertility reason. On review of previous investigations, it revealed left ovarian benign cyst, normal Doppler and normal tumor markers. The patient refused to do MRI in the past as she was confirmed that it is a benign cyst. No relevant past medical or surgical or family history. On examination upon admission, the patient was vitally stable, abdominal examination revealed left lower abdominal tenderness, rigidity and rebound tenderness. PV not done as the patient is virgin. Abdominal ultrasound revealed cystic mass in left adnexa measuring 9x6 cm but the vascularity of ovary was not adequately assessed by abdominal doppler as the patient is virgin. Her lab preoperative investigations were normal tumor markers and negative pregnancy test. The provisional diagnosis was left ovarian torsion vs complicated ovarian cyst. Plan was to proceed for laparoscopy for left ovarian de-torsion and cystectomy.
During laparoscopy after safe entry; a 10x10 cm left retroperitoneal cyst with no apparent left ovary (Fig. 1.) the primary consultant notified the gyneoncologist on call who came and scrubbed due to critical position of retroperitoneal cyst and its approximate to great iliac vessels and ureter, Opening of the peritoneum to enter into the retroperitoneal space , the cyst was dissected then a whitish appearance of the cyst that brought the suspicion it is ovarian in nature (Fig. 2.), we punctured the cyst to drain the fluid then ovarian cystectomy was done. Identification of the left ureter was done (Fig. 3.). The cyst was sent for histopathology which revealed ovarian serous cystadenoma (Fig. 4a & b.). The postoperative period passed smoothly, the patient was happy with the procedure because her fear of oophorectomy. She came after one week to do ultrasound which was free with no recurrence, no adverse or unanticipated events happened postoperatively.
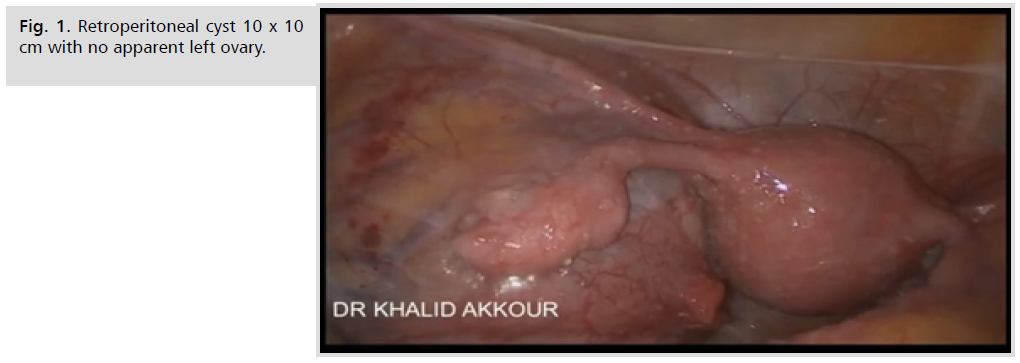
Fig 1. Retroperitoneal cyst 10x10 cm with no apparent left ovary.
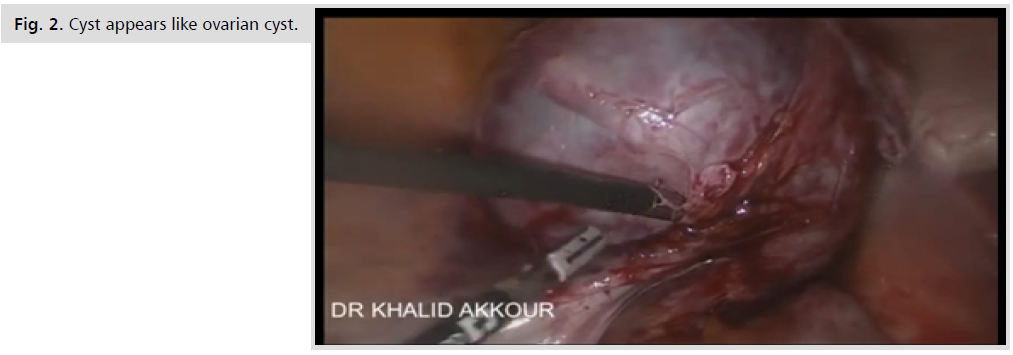
Fig 2. Cyst appears like ovarian cyst.
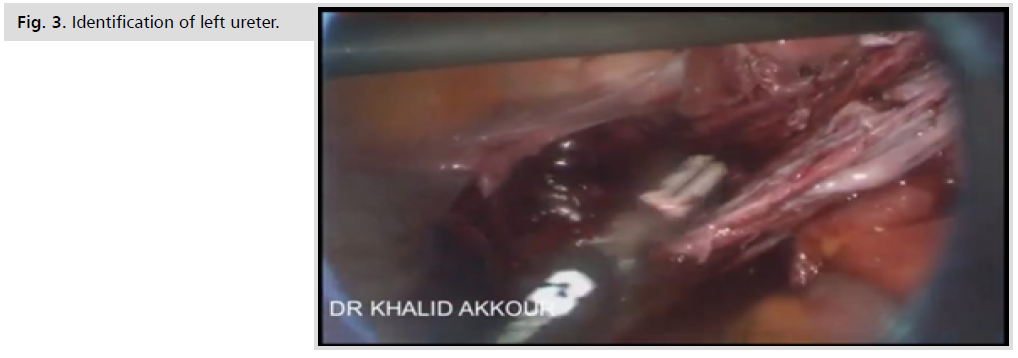
Fig 3. Identification of left ureter.
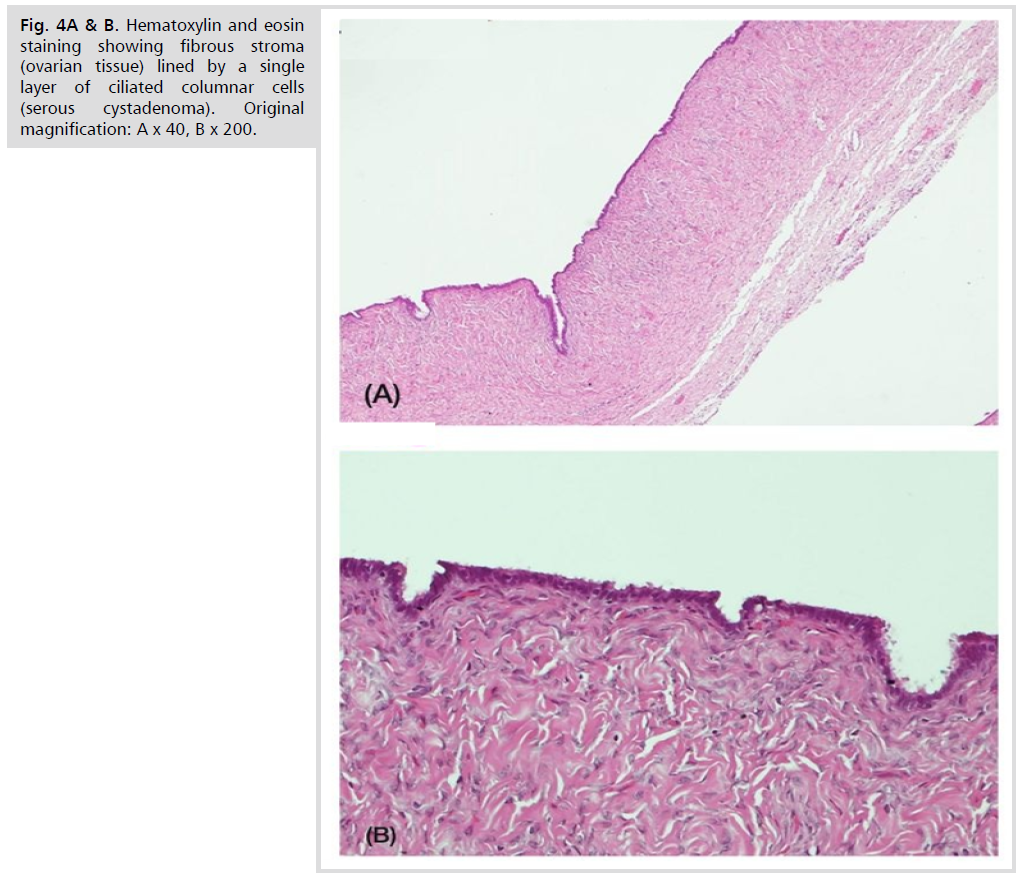
Fig 4. Hematoxylin and eosin staining showing fibrous stroma (ovarian tissue) lined by a single layer of ciliated columnar cells (serous cystadenoma). Original magnification: A x 40, B x 200.
Discussion
Primary retroperitoneal serous cystadenoma (PRSC) is an extremely uncommon lesion of retroperitoneum. Very few case reports of this entity have been described in the literature [1]. No Cases has been described among these cases to be ovarian, only few cases of mucinous cystadenoma and dermoid cyst were described [3].
In the case report of Mouri et al, they operated 78 years old lady with right retroperotonial cyst 28 x 17 cm displacing the bowel and loops of intestine to the left Pathology revealed a benign serous cystadenoma with tubal metaplasia with no ovarian tissue found [4].
In the case report of Popkharitov et al., a 28 yeaar old woman had recurrent abdominal pain of 6 month duration; a retroperitoneal cyst 15x15 cm was diagnosed in the lateral left retroperitonium adjacent to kidney. The pathology revealed serous cystadenoma with border line foci with no ovarian tissue found [5].
The limitation of this study is that patient did not perform MRI which could diagnose the retroperitoneal cyst from the start. The strength of the study is the competence of gyneoncologist consultant who performed the good dissection in the retroperitoneal apace and completed the cystectomy without injury to vessels or ureter.
Conclusion
The take away lesson from this rare from our point of view is that MRI is to be obligatory in any virgin patient to diagnose any ovarian cyst and laparoscopists must have experience with dangerous retroperitoneal space to avoid injury of ureter and great vessels.
Ethics
Written informed consent was obtained from the patient for publication of this case report and all accompanying images.
No Ethical review Board is needed in our hospital to publish case reports.
Consent for Publication
The patient gave informed written consent to publish the case and photos of laparoscope.
Data Statement
Data including video of laparoscope and patient mobile number available upon request.
Conflict of Interest
The authors have no conflicts of interest to declare.
Funding
This study received no financial support.
Acknowledgement
Not applicable.
Authors Contribution
(A) Study Design · (B) Data Collection . (C) Statistical Analysis · (D) Data Interpretation · (E) Manuscript Preparation · (F) Literature Search · (G) No Fund Collection
References
- Chen F, Jiang K. Giant Primary Retroperitoneal Serous Cystadenoma: A Rare Entity Mimicking Multiple Neoplastic and Nonneoplastic Processes. Arch Pathol Lab Med. 2020;144(4):523-528.
- Campoy CN, Ocon FM. 376 Ovarian remnant syndrome and recurrent ovarian serous cystadenoma. Eur J Obstet Gynecol Reprod Biol. 2022;270:e22-23.
- Gotoh K, Konaga E, Arata A, et al. A case of primary retroperitoneal mucinous cystadenocarcinoma. Acta Med Okayama. 1992;46(1):49-52.
- Mori A, Changela K, Alhankawi D, et al. A giant primary retroperitoneal serous cystadenoma: case report and review of retroperitoneal cysts. Surg J. 2017;3(01):e32-e37.
- Popkharitov A, Matev A, Popkharitov T, et al. Primary retroperitoneal serous cystadenoma with borderline malignancy: a case report and review of the literature. Trakia J Sci. 2013;4:368-73.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Author Info
Nada Alayed1, Khalid Akkour1, Rana Al Ohaly1, Fady Alakeel2, Amany Abuhassan2, Ahmed Sherif Abdel Hamid AS1,3* and Mohamed Mahmoud Abdelaziz42Department of Pathology, College of medicine, King Saud University, Riyadh, Saudi Arabia
3Department of Obstetrics and Gynecology, Faculty of medicine, Ain Shams University, Cairo, Egypt
4King Khalid University hospital, King Khalid university, Saudi Arabia
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.