Research Article - (2023) Volume 0, Issue 0
Laparo-endoscopic single-site surgery vs. conventional multi-port laparoscopy in presumed benign ovarian cystectomy: A randomized controlled trial
Alaa M. Atef, Alaa El Feky, Ahmed Tharwat, Mahmoud Nabil Abd-Allah* and Amr Helmy YehiaReceived: 21-Apr-2023, Manuscript No. gpmp-23-122502; Editor assigned: 23-Apr-2023, Pre QC No. P-122502; Reviewed: 04-May-2023, QC No. Q-122502; Revised: 19-May-2023, Manuscript No. R-122502; Published: 01-Jun-2023
Abstract
Background: Single Port Laparoscopic Surgery (SPLS) is a novel technique quickly recognized worldwide.
Aim: This study aimed to evaluate the postoperative consequences of Laparo-endoscopic Single-Site Surgery (LESS) relative to conventional laparoscopy in the presumed benign ovarian cysts.
Methods: Seventy women diagnosed with benign ovarian pathology attending Ain Shams University Maternity Hospital between January 2020 and December 2022 were divided into two equal groups. Thirty-five patients underwent LESS surgery, while the other 35 (control group) underwent conventional multiport laparoscopic surgery. We analyzed the demographic characteristics of the patients, including age, BMI, Parity, and history of previous abdominal surgery. We analyzed operative outcomes, mainly the postoperative pain in the first 24 hours. In addition to operative time, intraoperative blood loss, and postoperative hospital stay.
Results: Our results revealed that the demographic characteristics of the patients and the postoperative VAS pain score had no statistically significant difference between the two groups in the 6-hour, 12-hour, and 24-hour (P>0.05). Consequently, the consumption of additional analgesics (ketolac, 10 mg/tablet) during the first postoperative week was non-significantly lower in the LESS group compared to the Multiport group. Only 2 cases (5.7%) in the LESS group required additional port insertion due to extensive pelvic adhesions. The operative time was (49.3 ± 15 min) and (41.8 ± 18 min) and the operative blood loss was (78 ± 20 ml) and (69 ± 18.5 ml) in the LESS group and the Multiport group, respectively, with no statistically significant difference between the two groups (P>0.05). There was no statistically significance difference between the two groups in the postoperative hospital stay.
Conclusion: The LESS technique for ovarian cystectomy is feasible, safe, and equally effective compared to the conventional technique with a short learning curve.
Keywords
Laparoscopic surgery; Ovarian cyst
Introduction
Benign ovarian masses are one of the most common gynecologic problems. Laparoscopic surgery has become superior to laparotomy as it results in shorter recovery with less hospital stay, reduced postoperative pain, better cosmesis, and minimal complications [1].
In conventional laparoscopy, three or four ports are used for successful laparoscopic surgery. In the past few decades, there has been a significant change in the preferred surgical approach from laparotomy to laparoscopy in gynecology. The development of new and advanced instruments has made it easier to perform complex procedures. Recently, there has been a focus on reducing the number and size of laparoscopic incisions, with the ultimate goal of having no visible scars. Laparoendoscopic Single-Site Surgery (LESS), also known as single-incision laparoscopy, involves using one small skin incision instead of multiple incisions for laparoscopic surgical procedures [2,3].
In 1991, Pelosi and Pelosi introduced a new technique for laparoscopic hysterectomy with bilateral salpingo-oophorectomy. The technique, called single umbilical puncture laparoscopy, involved using only one puncture in the umbilicus. The surgical outcomes have shown that this technique is both safe and effective [4].
Laparoendoscopic Single-Site Surgery (LESS) has many benefits over conventional laparoscopy as better cosmesis using only one multichannel port in addition to reducing risks associated with multiple punctures. However, there were some limitations for cystectomy due to technical problems resulting from having too many instruments in a small space hindering each other mobility. That’s why it failed to gain too much popularity [3,4]. Recently, advanced specifically designed laparoscopic cameras and flexible endoscopies have overcome these single-port laparoscopic technical problems [5].
Objective
The objective of our study is to assess the postoperative results of laparo-endoscopic single-site medical procedures compared with traditional laparoscopy in assumed benign ovarian pathology.
Materials and Methods
Our research is a clinical trial that involved 70 women diagnosed with Benign Ovarian Pathology (PBOP), which was conducted at Ain Shams University Maternity Hospital between January 2020 and December 2022. The study was approved by the ethical committee of the Faculty of Medicine at Ain Shams University (FMASU) and registered in clinicaltrials.gov NCT04788498.
The study enrolled women between 18 and 45 years of age with a BMI less than 35 kg/m2 who had a surgical indication for a presumed benign ovarian pathology. The inclusion criteria were simple ovarian cysts (>7 cm - <15 cm) that persisted for over 90 days or symptomatic patients with complicated cysts such as hemorrhage or torsion.
We excluded patients who had previously undergone midline laparotomies, had chronic pelvic pain, endometriosis, PID, or had a RMI (Risk of Malignancy Index) score of more than 200. Moreover, women who did not have a native umbilicus that made entry into a single port challenging were also excluded. Additionally, any contraindications to laparoscopy, general anesthesia, or painkillers were also considered as exclusion criteria.
All women who were included underwent a thorough evaluation of their personal medical and surgical history, as well as a pelvic examination. Additionally, all patients were subjected to a transvaginal or pelvic ultrasound, along with blood tests such as CBC and CA 125 to calculate RMI. Prior to the surgery, all patients underwent a preoperative anesthesia consultation, which took place the day before the surgery.
Seventy eligible women were randomly divided into two equal groups, namely Group A and Group B. Group A consisted of 35 patients who underwent LESS (laparoendoscopic Single-Site Surgery) while Group B consisted of 35 patients who underwent conventional multiport laparoscopic surgery. The randomization process was carried out by using a computer random sequence generator. Sequentially numbered opaque sealed envelopes were used for randomization, and each envelope contained the method of intervention according to the random sequence. The envelopes were opened on the day preceding the surgery.
Surgical technique
All patients received 1 gram of intravenous third-generation cephalosporins (Ceftriaxone®) one hour before undergoing Laparoscopy. After induction of general anesthesia and endotracheal intubation, the patient was positioned in the dorsal lithotomy position with their legs upheld in stirrups with a Trendelenburg tilt. Then, a uterine manipulator (Cohen cannula) was placed through the uterine cervix to mobilize the uterus and adnexal mass during surgery. The surgeries were performed or supervised by the same surgeon who had expertise in the specific area of intervention.
In group A (LESS surgery group); Abdominal access was achieved using the modified Hasson technique. This involved creating a single 2 cm vertical intra-umbilical incision, followed by a sharp incision of the subcutaneous tissue and rectus fascia. Then, the peritoneum was incised using Metzenbaum scissors. A SILS Port (Covidien®) with three access channels was inserted through the incision using a Heaney clamp. To create a carbon dioxide pneumoperitoneum, the pressure was set at 15-20 mmHg. A 10 mm rigid video laparoscope was used along with two classical non-articulating straight laparoscopic instruments. If there was insufficient surgical movement for dissection, cutting, or coagulation due to crowding of the instruments, the surgeon would change the placement of the instrument or their position from the lateral side of the patient to the patient's head. Finally, the fascia was closed using vicryl 1 interrupted stitches.
In Group B, a conventional multiport laparoscopy was performed using a three-port system. The main port was inserted through the umbilicus while two accessory ports were inserted on the left and right lower quadrant region. After gaining entry, whether through single port or multiports, the pelvis was carefully assessed to avoid any other pelvic pathology. Once the cyst was aspirated, a divergent traction technique was used to remove the cyst from the ovarian wall. Bipolar energy was applied to ensure hemostasis if necessary. After the cystectomy, the ovary was left unstitched. Finally, the tubal patency was evaluated by trans-cervical infusion of methylene blue, as needed.
All interventions, including the operator and first assistant, surgical procedures, anesthetic method, and even instruments used, were similar between the two groups, except for the number and sizes of port entry points.
Both groups of patients were allowed to have clear oral fluids after they had recovered from anesthesia, and were able to begin a soft diet on the first day after surgery. Postoperative pain was managed using parenteral non-steroidal anti-inflammatory drugs (Ketorolac®, 30 mg) every 8 hours on the day of the surgery and oral non-steroidal anti-inflammatory drugs (ketolac®, 10 mg) every 8 hours from the first postoperative day. Additional analgesia was provided as requested. Patients were discharged once they had resumed their normal activities, and if there were no complications.
Study outcomes
The primary outcome of the study was to evaluate the level of pain experienced by patients within the first 24 hours after surgery using a Visual Analog Scale (VAS Score) ranging from 0 (no pain) to 10 (unbearable pain). The VAS Score was recorded at 6, 12, and 24 hours postoperatively. Data collection was done blindly by an independent specialist who was not aware of the group allocation. Participants were first assessed at the hospitalization unit and later contacted via phone for a follow-up assessment after a week.
Secondary outcomes
Operative time was defined as the duration from the beginning of the skin incision to the completion of the trocar site skin closure.
The intra-operative blood loss by calculating amount of blood in the suction bottle after subtraction of fluids used for peritoneal lavage (in mL) in addition to postoperative hemoglobin drop.
The requirement for conversion to laparotomy in the two groups.
The need to add an extra trocar in the two groups.
Postoperative hospital stay.
The utilization of extra analgesics and the number of tablets consumed by a phone call seven days after the intervention.
The postoperative complications (e.g., port site infection, ileus and hematoma of the abdominal wall).
The cosmetic appearance of the post-surgery scar was evaluated on both day 1 and day 7 using the Patient and Observer Scar Assessment Scale (POSAS). This scale includes two numerical scales that assess the signs and symptoms of healing. It consists of a patient scale and an observer scale, each containing six items rated from 1 to 10. A score of 1 represents ordinary skin, while a score of 10 represents the worst possible scar. The total score is calculated by adding the patient and observer scores and ranges from 6 to 60. The patient scale assesses scar-related pain, itching, color, stiffness, thickness, and regular skin, while the observer scale assesses vascularity, pigmentation, thickness, relief, pliability, and surface area [6].
Collection and processing of the data: A Case Report Form (CRF) will be used to collect prospective data on the day of the intervention and subsequently for the intervention's aftereffects. To ensure that they were eligible, the participants underwent preoperative evaluation. Data were collected during the perioperative period up to 24 hours after the intervention, as well as on day 7 and one month after the intervention. The CRF was updated with the patient-provided data at 2, 4, and 6 hours after the intervention, as well as phone-obtained data at 24 hours, seven days after the procedure, and one month after the procedure during the postoperative consultation.
Statistical analysis: MedCalc© version 18.2.1 (MedCalc© Software bvba, Ostend, Belgium) and IBM© SPSS© Statistics version 23 (IBM© Corp., Armonk, NY) were used for data analysis. The independent t-test was used to compare inter-group differences for continuous numerical variables that were presented as mean and SD. Significant outliers in skew variables were converted to logarithmic form and displayed as the mean and 95% confidence interval. Fisher's exact test was used to compare differences between categorical variables that were presented as numbers and percentages. To check for trends, ordinal data were compared using the chi-squared test. Any continuous variable measured twice or more on the same case was compared using a repeated measure ANOVA with a between factor. P-values with two sides that were ≤ 0.05 were deemed statistically significant.
Results
A total of 77 patients underwent eligibility assessment for the study, out of which 70 patients (35 in each group) were included. Five patients were excluded based on the inclusion criteria and two patients refused to participate in the study (Fig. 1.). The analysis was conducted using data from 68 patients who were diagnosed with ovarian cysts. Out of these, 35 patients were randomly selected to undergo LESS, while the other 35 underwent conventional multiport laparoscopy. However, two patients from the LESS group required additional port insertion and were excluded from the primary outcome analysis. Tab. 1. shows that both groups had similar demographic characteristics.
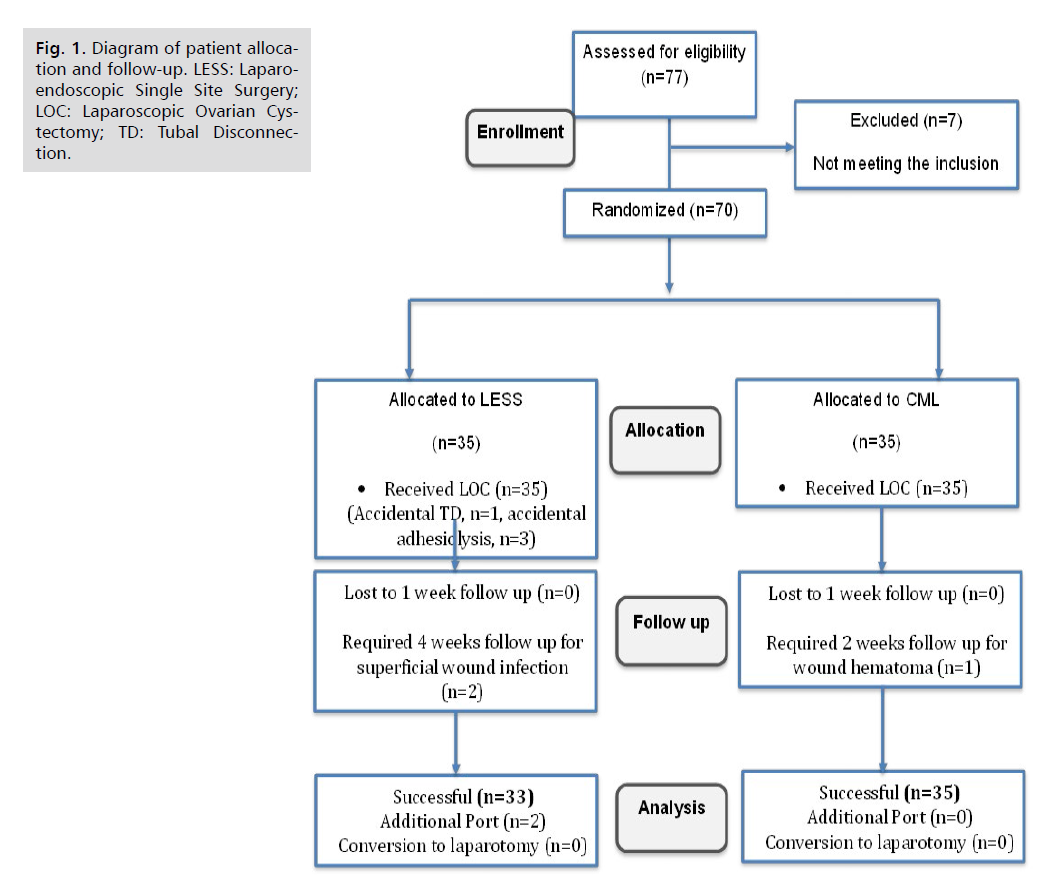
Fig 1. Diagram of patient allocation and follow-up. LESS: Laparoendoscopic Single Site Surgery; LOC: Laparoscopic Ovarian Cystectomy; TD: Tubal Disconnection.
| Variable | LESS (N=35) | Multiport (N=35) | P-value | Significance |
|---|---|---|---|---|
| Age (years) | 31.2 ± 5.1 | 30.2 ± 4.7 | 0.394* | No statistically significant difference |
| BMI (kg/m2) | 33.4 ± 3.4 | 32.6 ± 3.8 | 0.092* | |
| Parity | 3 (1 – 5) | 2 (1 – 4) | 0.184* | |
| History of previous abdominal surgery | 19 (54%) | 17 (48.5%) | 0.209# |
Tab. 1. Demographic characteristics of both study groups.
There was no statistically significant difference in postoperative pain score (VAS score) between the two study groups at 6, 12, and 24 hours (Tab. 2.).
| Post-operative VAS pain score |
LESS (N=33) | Multiport (N=35) | P- value | Significance | |
|---|---|---|---|---|---|
| After 6 hours | Mean ± SD | 5.26 ± 1.31 | 5.06 ± 1.66 | ^0.909 | No statistically significant difference |
| After 12 hours | Mean ± SD | 3.23 ± 1.17 | 3.49 ± 1.5 | ^0.253 | |
| After 24 hours | Mean ± SD | 1.66 ± 0.68 | 1.69 ± 0.72 | ^0.896 | |
Tab. 2. Postoperative pain score (VAS score) in both study groups.
Tab. 3. indicates that in the first week after surgery, the LESS group had a lower demand for extra painkillers (10 mg ketorolac tablets) than the multiport group. However, the difference between the two groups was not statistically significant. Our research discovered that in two instances (5.7%) from the LESS group, extra ports were necessary to carry out the surgery using a single-port for better manipulation.
| Measures | LESS (N=33) | Multiport (N=35) | ^P-value |
|---|---|---|---|
| Consumption of additional analgesics | 16 (48.5%) | 18 (51.4%) | 0.99 |
| No. of tablets | 3 (2-5) | 4 (2-6) | 0.738 |
Tab. 3. The consumption of additional analgesics (ketolac, 10 mg/tablet) among the studied groups.
Based on an intention-to-treat analysis, our research findings indicate that the only intraoperative complications in the multiport group were limited to one case of extraperitoneal insufflation, which was primarily attributed to the patient's obesity. Neither group experienced any bowel damage, vascular injury, or the need for a blood transfusion. The postoperative complications were as follow: 1 case of wound hematoma in the Multiport group that required conservative management for 2 weeks, 2 cases of wound infections in the LESS group that was superficial, while ileus were 1 case in the LESS group, and 2 cases in the Multiport group.
Fig. 2. illustrates the incidence of intraoperative and postoperative complications. However, these differences were not statistically significant Fig. 3. shows The longer hospital stay was related to postoperative ileus (1 patient in LESS group vs. 2 patients in multiport group), wound hematoma (1 patient in multiport group) and delayed bowel movement (5 patients). These differences were not statistically significant (data not tabulated). There was a statistically significant difference between the two procedures with LESS having a lower Psoas score at day 7 with subsequent cosmetic appearance (Tab. 4.).
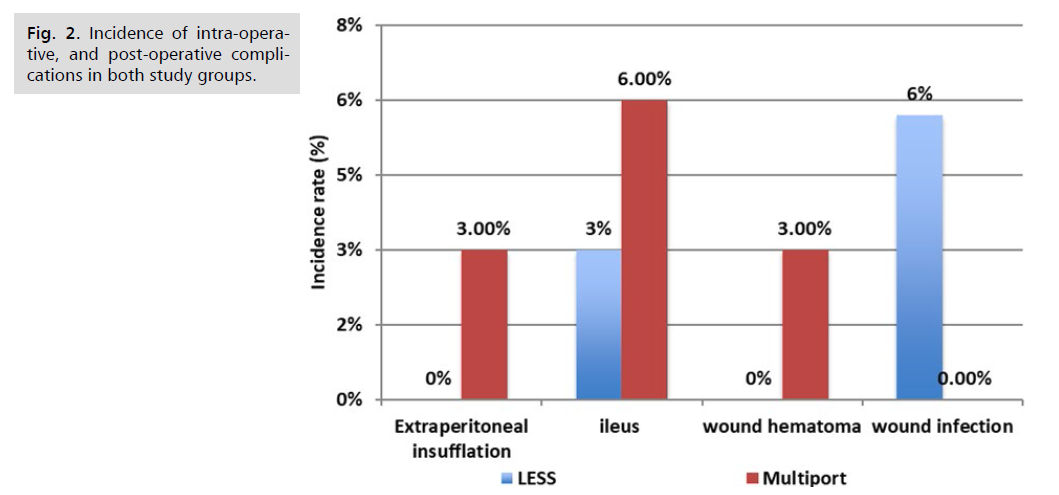
Fig 2. Incidence of intra-operative, and post-operative complications in both study groups.
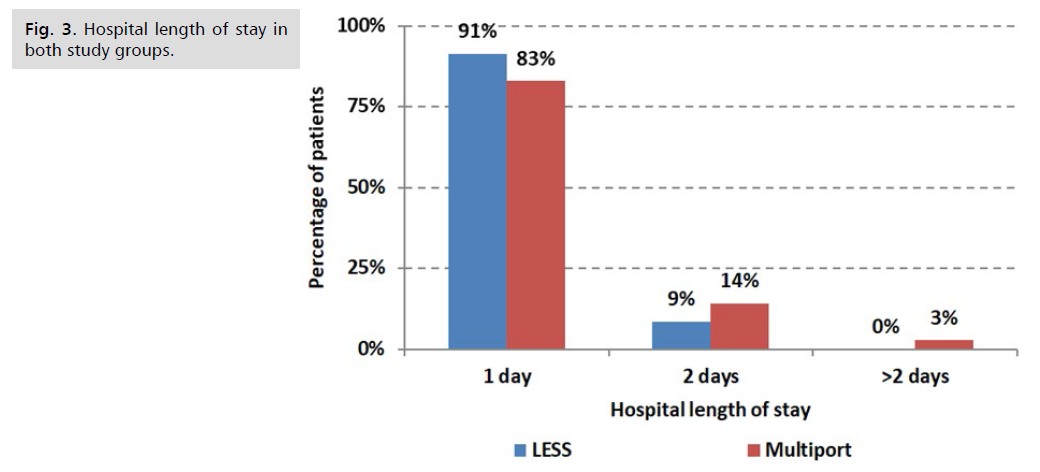
Fig 3. Hospital length of stay in both study groups.
| POSAS | LESS (N=33) | Multiport (N=35) | ^P-value |
|---|---|---|---|
| 1-day post-operative | 14.3 | 14.9 | 0.72 |
| Range | 14.6 – 15 | 15.2 - 15.7 | |
| 7 days post-operative | 10.6 | 12 | 0.02 |
| Range | 10.0 - 12.6 | 11.2 - 14 |
Tab. 4. POSAS score in both study groups at follow up.
Discussion
Over the last decade, there has been a rise in the use of laparoscopic procedures for treating benign ovarian tumors surgically. Laparoscopy has helped to reduce the costs of treating such tumors, as well as postoperative complications, pain, and hospital stays. Additionally, with the introduction of advanced instrument technology, single-port laparoscopic approaches have recently emerged for abdominal and pelvic surgeries. Initial experience has shown that single-port access laparoscopy is a safe and practical option.
Our results and their interpretation
According to the current study, there was no statistically significant difference in age, BMI, or parity between the LESS and Multiport groups. The two groups' most common reason for previous surgical procedures was cesarean section (57.8% vs. 53%), with appendectomy coming in second (26.4% vs. 35.3%) with no statistically significant difference in past surgical history between the two groups.
According to our findings, there was no significant difference in postoperative pain scores between the two groups at 6, 12, and 24 hours. As a result, during the first week after the operation, the LESS group's use of additional analgesics (ketorolac, 10 mg/tablet) did not significantly decrease compared to the Multiport group. This was most probably attributed to the avoidance of agonizing lateral ports incisions through the rectus musculature.
The comparison of our results in relation to similar studies
In line with our findings, Song, et al. assessed postoperative pain using VAS scores at 6, 24, and 48 hours. They concluded that there was no statistically significant difference between the two techniques [7,8].
Fagotti, et al. found that using LESS (Laparoendoscopic single-site surgery) to treat benign adnexal disease resulted in lower postoperative pain levels compared to other methods. They measured this using VAS (Visual Analog Scale) score, and they also observed a decrease in the need for additional pain medication after the procedure [9]. Angioni, et al. found that postoperative pain was significantly less in the LESS group than in the multiport group. The mean VAS scores were 5.2 and 8.2, respectively [10].
Laparoscopic ovarian cystectomy with a single port in the LESS group was successful in 35 patients, despite being a new technique. In only 2 cases (5.7%), an additional port was needed due to extensive pelvic adhesions. In contrast, the conventional multiport group did not require any additional ports. In concordance with our results, Sandberg, et al. 7 evaluates the rate of additional ports needed during more sophisticated LESS surgery for hysterectomy, reported that out of the 1344 patients, 48 (3.5%) had at least one additional port, compared to one (0.06%) in the conventional group. This is consistent with Dursun, et al. who reported the use of standard straight laparoscopic instruments in LESS surgery in the treatment of adnexal mass as ovarian cystectomy, and all 14 cases were successful [11]. According to Garcia-Henriquez, et al. Single-Incision Laparoscopic Surgery (SILS) can be performed with standard straight surgical instruments [12].
The same results were reported by Tam, et al. moving this is in line with Dursun, et al.'s report of successful treatment of adnexal mass and ovarian cystectomy using standard straight laparoscopic instruments in LESS surgery. The instruments between hands during surgery may be necessary. However, crossing two straight instruments did not differ substantially from standard laparoscopic skills [13].
Regarding the operative data, our analysis showed that the LESS group and Multiport group had operative times of 49.3 ± 15 min and 41.8 ± 18 min, respectively, and operative blood losses of 78 ± 20 ml and 69 ± 18.5 ml, respectively. There was no statistically significant difference between the two groups for either the duration of the procedure in minutes or the volume of blood lost in milliliters. As a result, the group did not differ statistically significantly in the pre-operative, post-operative, or drop in Hb values.
In agreement with our findings, Dursun et al., reported no differences in median operative time in laparoscopic adnexal surgery between LESS and conventional groups (64 minutes vs. 57.5 minutes) [11]. A surgical procedure requires sufficient education and experience. As surgeons gain more experience, procedure duration is expected to decrease [14].
Lee, et al. found a statistically significant difference (P=0.0007) in median operative time for treating adnexal mass between the LESS group (44 minutes) and the multiport group (49 minutes) [15]. The study did not identify any specific factors that contribute to a shorter operating time for LESS surgery. However, it is interesting to note that in our study, the operating time was reduced dramatically over the course of three months (less than ten cases) without the use of specialized tools or training. The time was reduced from sixty minutes to thirty minutes. Based on our operative results, it is evident that the learning curve for LESS laparoscopy is shorter.
The results obtained were comparable to Takahiro and Satoru's study in 2011, which showed that LESS surgery had a shorter learning curve. This is because the skills required for performing and completing the LESS procedure are the same as those needed for traditional laparoscopy. Moreover, any issues that might arise during LESS are more likely to occur in the early stages of the learning process. According to Escobar, et al. LESS surgery has a shorter learning curve, especially for surgeons who are already skilled in conventional multiport laparoscopy. This makes the transition to LESS surgery easier and results in a significant decrease in operative time and the time required closing the single port used in LESS surgery. The study suggests that a surgeon needs to perform 10 to 15 LESS surgeries to become proficient in this technique [2].
In terms of hospital stay, almost all patients from both groups were discharged from the hospital one day after the surgery. The percentage of patients who were released from the hospital was 91.4% in the LEES group and 82.9% in the multiport group. There was no significant difference in the duration of the hospital stay between the two groups. However, the patients who experienced postoperative ileus had a longer hospital stay. Only one patient (2.9%) in the LESS group and two patients (5.7%) in the multiport group had postoperative ileus.
Similar findings were found by Lee, et al. in which the median postoperative stay was equal in both groups which was approximately 2 days [15].
Regarding the surgical complications, the findings of our study showed that neither group experienced intestinal injury, vascular injury, or the need for a blood transfusion. Instead, the only intraoperative complication was a case of extraperitoneal insufflation as a result of the procedure in the multiport group. The postoperative complications occurred in form of one case of wound hematoma in the Multiport group that required frequent dressing, wound compression, and hemostatics until complete healing after 2 weeks and two cases of wound infections in the LESS group, one of which required 4 weeks follow up along with frequent dressing and topical antibiotic cream and the other in addition to frequent dressing required 7 days course of oral antibiotics without needing any further intervention, while ileus occurred in one case in the LESS group, and two cases in the Multiport group. However, the differences in intra-operative and post-operative complications were statistically non-significant in the studied groups. Extraperitoneal gas insufflation occurs due to failure to introduce the Veress needle into the peritoneal cavity in obese patients and this occurred in about 2% of cases [16].
In agreement with our findings, Karim, et al. reported no incidence of wound infection in the multiport group with only one patient in LESS group had superficial wound infection (2.22%) [17]. This is consistent with Omori et al., who reported 2 cases of surgical site infection out of 7 of SILS gastrectomy and all recovered with conservative treatment [18]. Also, Wakasugi, et al. (2015) reported that seroma was the only postoperative wound complications and its incidence was 11%. The cosmetic outcome after surgery was assessed using Patient and Observer Scar Assessment Scale (POSAS) that is valid and reliable. The scar was assessed on day 1 and after 7 days [19]. The study findings showed that, on day one, there was no statistically significant difference in the cosmetic outcome between the LESS group and the multiport group's median scores (14.3 vs. 14.9, P=0.72). The LESS group showed improved objective and subjective cosmetic outcomes, as evidenced by the significantly lower median score (10.6 vs. 12, P=0.02) at 7 days after discharge when compared to the Multiport group. These findings were also supported by another study of Angioni, et al. [10] who reported significantly higher cosmetic satisfaction at at one week, four weeks, and twenty-four weeks following surgery for the LESS group. Similar results were reported by Fagotti, et al. [9] and Angioni, et al. [10] who revealed that LESS surgery outperforms traditional laparoscopic surgery in terms of patient satisfaction and cosmetic outcome. All, however, stated that in order to draw firm conclusions regarding the cosmetic result, more comparative research with larger sample sizes are required. In addition, according to three studies reported on cosmetic results, patients in the LESS group were significantly more satisfied with their scars and had higher satisfaction with their own body at three measured moments (1, 4, and 24 weeks) [7]. According to a previous survey, visibility is the most important factor in reflecting patients' satisfaction [20].
In contrast to our findings, Kim, et al. [21] studied the scar satisfaction using POSAS 1 week and 2 months after surgery and showed no difference between the single site group and the multiport one. The advantage of the umbilical scar over the abdominal scar is that it is well hidden. In addition, the umbilical skin is composed of relatively thin epidermis and dermis compared to other skin thus associated with less pigmentation and thinner scar thickness [22]. Moreover, the umbilicus lacks significant intrinsic blood vessels and nerves, and there are no muscle layers. In contrast to the lower quadrant of the abdomen, that includes epigastric vessels and muscle layers. This will be more prominent if used a larger incision in the lower quadrant of the abdomen for larger trocar size in operative gynecological laparoscopies as using morcellators in myomectomies or specimen extraction [23].
Advantage and disadvantage of the LESS surgery only become apparent over time and following the implantation stage. Furthermore, it is difficult to determine whether single-port surgery should be an additional option for minimally invasive surgery [7].
This study has several strengths. Firstly, it has a randomized controlled study design. Secondly, the study assessed two different surgical routes, included a large number of women, and did not lose any patients during follow-up. It is one of the few studies in the world that compares using SILS port and straight laparoscopic instruments to conventional multiport laparoscopy in gynecological literature. Additionally, the study was conducted at a single facility with the same anesthetic protocol and surgical team, which likely improved the validity of the findings.
Limitations of the study
The findings of this research should be considered in light of its limitations, which include the fact, that ovarian reserve after single-port and multiport laparoscopic ovarian cystectomies were not assessed. Also, the study was conducted in a single center with a small target population, which limits its external validity as it may not be representative of the larger patient population. In addition, the short duration of patient follow-up prevented the demonstration of the long-term effects on factors such as reproductive outcome, menopausal age, or cyst recurrence. Therefore, further research is still needed to be conducted on this topic.
Conclusion
As evident from the current study that with a short learning curve, the LESS technique for ovarian cystectomy is practical, safe, and just as effective as the traditional method. Reducing port-related morbidity and improving patient satisfaction with regard to pain and cosmetic results are potential benefits that are pursued. It should be noted, though, that superficial wound infections can occur and that an extra port may be required in as many as 5.7% of LESS procedures.
References
- Aarts JW, Nieboer TE, Johnson N, et al. Surgical approach to hysterectomy for benign gynaecological disease. Cochrane Database Syst Rev. 2015(8).
- Escobar PF, Bedaiwy MA, Fader AN, et al. Laparoendoscopic Single-Site (LESS) Surgery in patients with benign adnexal disease. Fertil Steril. 2010;93(6):2074-2074e7.
- Bradford LS, Boruta DM. Laparoendoscopic single-site surgery in gynecology: A review of the literature, tools, and techniques. Obstet Gynecol Surv. 2013;68(4):295-304.
- Pelosi MA, Pelosi 3rd MA. Laparoscopic hysterectomy with bilateral salpingo-oophorectomy using a single umbilical puncture. N J Med. 1991;88(10):721-726.
- Piskun G, Rajpal S. Transumbilical laparoscopic cholecystectomy utilizes no incisions outside the umbilicus. J Laparoendosc Adv Surg Tech. 1999;9(4):361-364.
- Chae JK, Kim JH, Kim EJ, et al. Values of a patient and observer scar assessment scale to evaluate the facial skin graft scar. Ann Dermatol. 2016;28(5):615-623.
- Sandberg EM, La Chapelle CF, van den Tweel MM, et al. Laparoendoscopic single-site surgery versus conventional laparoscopy for hysterectomy: A systematic review and meta-analysis. Arch Gynecol Obstet. 2017;295:1089-1103.
- Song T, Kim ML, Jung YW, et al. Laparoendoscopic single site vs. conventional laparoscopic gynecologic surgery: A metaanalysis of randomized controlled trials. Am J Obstet Gynecol. 2013; 209(4):e1-e9.
- Fagotti A, Rossitto C, Marocco F, et al. Perioperative outcomes of Laparoendoscopic Single Site Surgery (LESS) vs. conventional laparoscopy for adnexal disease: A case control study. Surg Innov. 2011;18:29-33.
- Angioni S, Pontis A, Sedda F, et al. Single port vs. conventional multiport access prophylactic laparoscopic bilateral salpingo-oophorectomy in high risk patients for ovarian cancer: A comparison of surgical outcomes. Open Access Sci Med Res. 2015;8:1575-1580.
- Dursun P, Tezcaner T, Zeyneloglu HB, et al. Adnexal masses treated using a combination of the SILS port and non curved straight laparoscopic instruments: Turkish experience and review of the literature “Hindawi Publishing Corporation”. Minim Invasive Surg. 2013;836380:1-8.
- Garcia-Henriquez N, Shah SR, Kane TD. Single incision laparoscopic cholecystectomy in children using standard straight instruments: A surgeon‟s early experience. J Laparoendosc Adv Surg Tech. 2011;22(6):555-559.
- Tam YH, Lee KH, Sihoe JDY, et al. Initial experience in children using conventional laparoscopic instruments in single incision laparoscopic surgery. J Pediatr Surg. 2010;45(12): 2381-2385.
- Seow KM, Tsou CT, Lin YH, et al. Outcomes and complications of laparoscopically assisted vaginal hysterectomy. Int J Gynecol Obsttet. 2006;95:29-34.
- Lee IO, Yoon JW, Chung D, et al. A comparison of clinical and surgical outcomes between laparo-endoscopic single-site surgery and traditional multiport laparoscopic surgery for adnexal tumors. Obsttet Gynecol Sci. 2014;57(5):386-392.
- Gordon AG. Complications of laparoscopy. Pract Training Res Gynecol Endosc. 2017;136-142.
- Karim MA, Ahmed J, Mansour M, et al. Single incision vs. conventional multiport laparoscopic cholecystectomy: A comparison of two approaches. Int J Surg. 2012;10(7):368-372.
- Omori T, Oyama T, Akamatsu H, et al. Transumbilical single-incision laparoscopic distal gastrectomy for early gastric cancer. Surg Endosc Other Interv Tech. 2011;25(7):2400-2404.
- Wakasugi MM, Masuzawa T, Tei M, et al. Single-incision totally extraperitoneal inguinal hernia repair: Our initial 100 cases and comparison with conventional three-port laparoscopic totally extraperitoneal inguinal hernia repair. Surg Today. 2015;45:606-610.
- Yeung PP, Bolden CR, Westreich D, et al. Patient preferences of cosmosis for abdominal incisions in gynecologic surgery. J Minim Invasive Gynecol. 2013;20:79-84.
- Kim TJ, Shin SJ, Kim TH et al. Multi-institution, prospective, randomized trial to compare the success rates of single-port vs. multiport laparoscopic hysterectomy for the treatment of uterine myoma or adenomyosis. J Minim Invasive Gynecol. 2015;22:785-791.
- El-Oteify M, Saad El-Dien HM, Mubarak W. Sensory nerve endings in the human female umbilical skin: Light and electron microscopic study. Egypt J Histol. 2011;34:57-68.
- Lee D, Kim SK, Kim K, et al. Advantages of single-port laparoscopic myomectomy compared with conventional laparoscopic myomectomy: A randomized controlled study. J Minim Invasive Gynecol. 2017;25(1): 124-132.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Author Info
Alaa M. Atef, Alaa El Feky, Ahmed Tharwat, Mahmoud Nabil Abd-Allah* and Amr Helmy YehiaCopyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.