Research - (2024) Volume 19, Issue 2
Laboratory characteristics in anemic pregnant women to decide treatment with intravenous iron vs. Blood transfusion in Najaf province: A hospital-based study
Maryam K. Alaasam* and Nagham Yahya GhafilReceived: 03-Jun-2024, Manuscript No. gpmp-24-141238; Editor assigned: 04-Jun-2024, Pre QC No. P-141238; Reviewed: 17-Jun-2024, QC No. Q-141238; Revised: 21-Jun-2024, Manuscript No. R-141238; Published: 28-Jun-2024
Abstract
Background: Anemia affects over fifty percent of reproductive-age women globally, with a frequency of 29.9% among individuals aged 15–49 and 36.5% among pregnant women in 2019. Iron Deficiency Anemia (IDA) is common but often inadequately treated, leading to serious maternal and fetal complications, including postpartum depression, maternal mortality, and impaired brain development in children. Anemia can be classified by red blood cell size (microcytic, normocytic, macrocytic) or cause (low production vs. high loss), requiring comprehensive lab tests for accurate diagnosis. “The World Health Organization (WHO)” defines anemia in pregnancy as hemoglobin levels below 11 g/dl, with moderate cases between 10-10.9 g/dl and severe cases below 7 g/dl. Oral iron supplements have low compliance due to side effects, while intravenous iron is underutilized due to perceived risks and costs. Blood transfusions are critical but require careful monitoring and health sector support. Comprehensive diagnostic tests like serum iron and transferrin saturation are essential, especially with systemic inflammation or infection. The CDC also considers hemoglobin below 11 g/dl and hematocrit below 33% as anemic in pregnant women, emphasizing early and effective treatment to prevent severe complications.
Aim: The study aims to evaluate how anemia during pregnancy is managed in Al-Najaf hospitals, focusing on intravenous iron and blood transfusion, and their correlation with lab characteristics.
Method: A descriptive cross-sectional study was conducted in six hospitals in Al-Najaf. Data from pregnant patients treated for severe anemia were collected and compared with national guidelines to assess management practices.
Results: Blood transfusion was predominantly used for microcytic anemia (66 cases) and showed a significant association with moderate anemia (Hb scores 7-9.9 g/dL, P=0.001). Intravenous iron was mainly administered for moderate anemia (32 cases). The dosage of IV iron varied, primarily used for moderate anemia, with doses ranging from 1 to 4 amps.
Conclusion: Misdiagnosis of anemia is common. The majority of cases throghout pregnancy are microcytic anemia (98%) which treated with blood transfusions (67%), although intravenous iron (33%), which is considered safer, is also used. Following ASH guidelines and having a diverse blood supply are essential for effectively managing maternal anemia.
Keywords
Blood transfusion; Anemia; Pregnancy; Intravenous iron (IV iron); Hemoglobin
Introduction
Anemia affected over half of the world's female reproductive-age population in 2019, with a frequency of 29.9% among women aged 15–49 (36.5% among pregnant women and 29.6% among non-pregnant women of reproductive age) [1].
Inadequate iron stores in blood vessels are a significant issue for women all over the world, especially during periods of reproduction. The illness has a significant influence on female's lives and quality of life, however therapy is often inadequate, despite the high prevalence of IDA among reproductive-age women [2,3].
The majority of the world's population suffers from iron deficiency (ID). Irregular hemoglobin levels cause (IDA) when the body fails to produce enough iron to sustain hemoglobin production. Because of the growing size of the mother's red blood cells, the placenta, and the developing baby, the risk of (ID) during pregnancy is increased. Maternal neurological symptoms is linked to serious complications including postpartum depression, placental abruption, maternal death, and a great deal of morbidity or mortality for mothers. Maternal anemia has consequences on long-term neural growth and may worsen fetal intellectual disability, Attention Deficit Hyperactivity Disorder (ADHD), and Autism Spectrum Disorder (ASD) [4].
Anemia can be categorized according to the size of the red blood cells; manifestations of this system include "microcytic," "normocytic," and "macrocytic" anemia. A different approach to categorizing anemia highlights the underlying mechanism by distinguishing between an increase in red blood cell loss and a decrease in their synthesis. The existence of the primary hemolytic or loss of blood cause is indicated by a boost in number of reticulocyte [5]. There is a broad variety of medical issues that can lead to anemia, and determining the precise reason requires extensive laboratory testing, which presents difficulties in ordinary management [5].
The specific causes of anemia should be investigated, which often requires a variety of laboratory tests, and these categories assist in limiting it. You may use these tests to check for myeloma, inflammation, malnutrition, sickle cell disease, thalassemia, as well as the function of the kidney [6,7].
The likelihood for significant consequences, such as serious maternal morbidity, exceeds that in women who have antepartum anemia. A better understanding of which women are at increased risk for maternal morbidity and death may be achieved by early identification and management of anemia in the prepartum period. Hemoglobin concentrations less than 11 g/dl are considered anemia, according to the (WHO). Hemoglobin levels are used to classify the degree of gestational anemia: mild is defined as falling between 10 and 10.9 g/dl, moderate as falling between 7 and 9.9 g/dl, and severe as falling below 7 g/dl [8].
Over fifty percent of child-bearing women who take iron supplements orally report side effects such as constipation, vomiting, nausea, and epigastric pain. These negative outcomes can result in failure to comply and a long time to recover from anemia [9].
Uncertainty regarding expense and hazard lead to its improper usage or underutilization over gestation, despite the fact that intravenous (IV) iron treatment may rapidly boost the stores of iron and compensate for the poor intestinal absorption of oral formulations. The preceding iron injection preparations were linked to a substantially reduced chance of reactions due to hypersensitivity [10].
However, additional blood tests such as serum iron and transferrin saturation may be helpful in cases where a false-normal ferritin grade has been observed, such as in cases of systemic inflammation or infection, even though serum ferritin is the best diagnostic for IDA. For the purpose of ruling out other potential disorders, assessment for IDA is typically organized. Transfusion of blood is a critical medical procedure that plays a vital part in providing necessary treatment to patients. Hence, it is crucial for the competent health authorities to implement suitable and sufficient measures to guarantee that the healthcare facilities in the nation possess the fundamental prerequisites, such as the necessary human and financial resources, infrastructure, and other types of support, to deliver services in accordance with the established standards [11].
According to the Centers for Disease Control and Prevention (CDC), anemia observed during both the initial and final quarters is characterized by (Hb) grades below 11 g/dL and a quantity of packed cells below 33% [12]. Every quarter requires an evaluation of the related parameters. The negative impact of anemia on the mother or the unborn child is devastating [11].
The average healthy individual stores around 4 to 5 grams of iron in their body. The average daily intake of elemental iron for humans is 5–15 mg, with haem iron ranging from (1–5 mg). A significant amount of iron is absorbed in the duodenum and proximal jejunum, although only (1-2 mg) really makes it into the gut. To compensate for the daily losses caused by cell desquamation and blood loss, macrophages mostly recycling the (20-25mg/day) of iron that the body needs by swallowing erythrocytes [13].
Pseudo-anemia is a condition in which the count of red blood cells appears to be reduced due to the rise in blood levels throughout gestation [14,15]. The Mean Cell Volume (MCV) is a measure of the median size of a red blood cell. The formula for calculating hct/RBC yields femtoliters (fL), the standard unit of measurement. Microcytic means less than 80 fL, normocytic means 80–100 fL, and macrocytic means more than 100 fL [16].
Childbearing female (Hb) grades and Maternal Chorionic Villus sampling (MCV) have a weakly association. For this reason, keeping them inside the predetermined parameters is of the crucial significance [17]. (RBCs) carry oxygen and carbon dioxide in a complex protein called hemoglobin (Hgb) [18]. This component accounts for more than (95%) of the total dry weight of (RBCs). Hb comprises a quaternary arrangement with four globular proteins (2α and 2β globulins) and a heme group (fe2+, which binds oxygen) [16].
Aim
This study aims to assess anemia management methods during pregnancy in Al-Najaf hospitals/Iraq by intravenous iron (iron sucrose) and blood transfusion and this correlation with some laboratory characteristics that use to investigate anemia.
Method
Records of pregnant patients admitted for the treatment of anemia were examined at six hospitals that were chosen in Al-Najaf has conducted a descriptive cross-sectional study. A specific study form created for this purpose was used to collect the data. Participating in the data-gathering process were pregnant patients who had been hospitalized to hospitals in order to treat anemia. A comparison of the management practices and national guidelines was then used to examine the data that had been gathered.
Data Analysis
Descriptive statistics, which included computations of percentages and frequencies, were used to describe the study population. In order to examine the correlations, we used the 2016 version of Excel and SPSS 26,which is a statistical package for social science. A significant criteria of p_value < 0.05 was applied to evaluate the association between the categorical variables using the Chi-square test.
Results
Out of (113) pregnant women were specific diagnosis; (75) received blood and (38) received IV iron (Tab. 1. and Fig. 1.).
| Type of Anemia Management vs. Diagnosis | Diagnosis | |||||
|---|---|---|---|---|---|---|
| Macrocytic | Microcytic | Normocytic | Total | P-value | ||
| Type of anemia management | Blood Transfusion | 1 | 66 | 8 | 75 | 0.582 |
| IV IRON | 0 | 32 | 6 | 38 | ||
| Total | 1 | 98 | 14 | 113 | ||
Tab. 1. Type of anemia management vs. diagnosis.
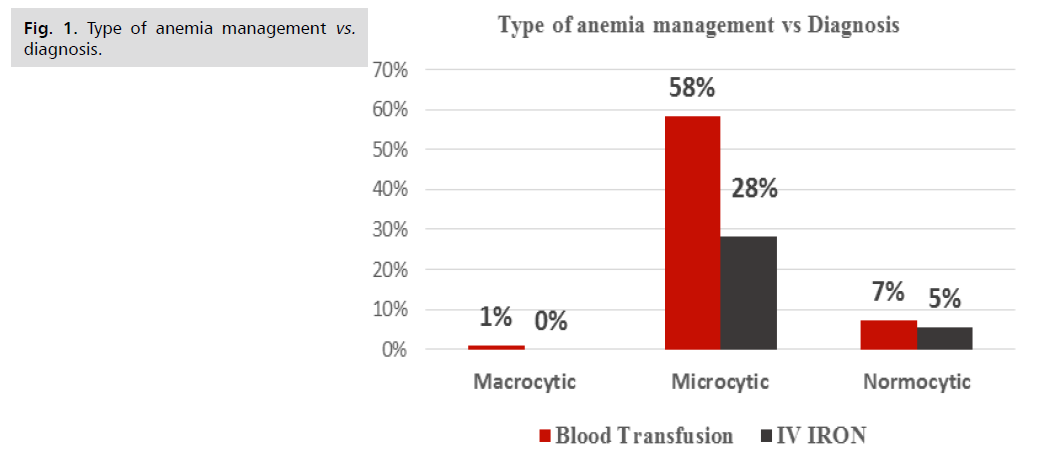
Fig 1. Type of anemia management vs. diagnosis.
The American Society of Hematology (ASH) provides a classification of anemia severity during pregnancy based on Hemoglobin (Hb) levels. This classification helps in identifying and managing the condition effectively. Tab. 2. and Fig. 2. summarizes the severity of anemia, corresponding scores, and Hb levels.
| Severity of anaemia | Score | Hb level |
|---|---|---|
| Severe anaemia | 1 | <7 g/dL |
| Moderate anaemia | 2 | 7-9.9 g/dL |
| Mild anaemia | 3 | 10-10.9 g/dL |
Tab. 2. Score of Hb in pregnancy according to ASH.
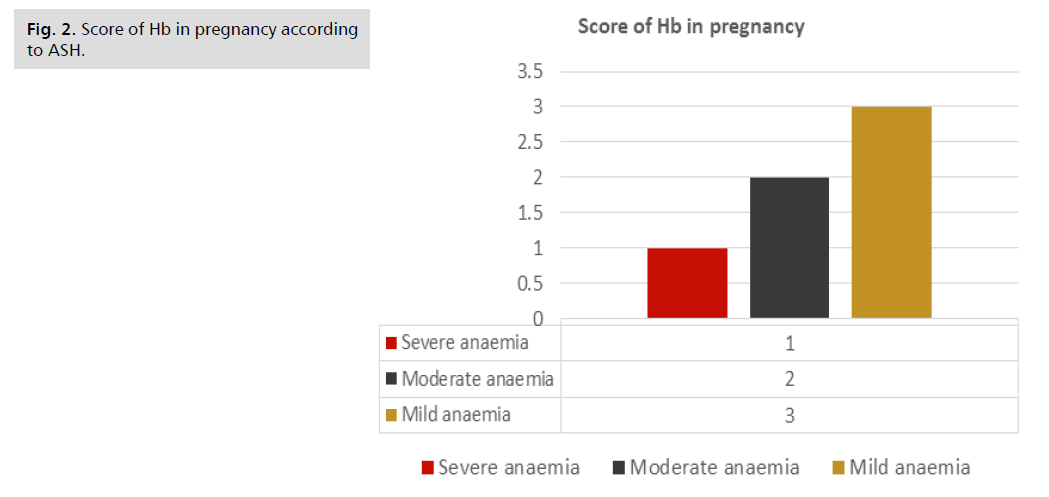
Fig 2. Score of Hb in pregnancy according to ASH.
Tab. 3. and Fig. 3. data presented here compare two methods for treating anemia: blood transfusions and intravenous iron, across a range of hemoglobin scores that correspond to the severity of the condition.
| Type of Anemia Management vs. Score of Hb | Score of Hb | P-value | ||
|---|---|---|---|---|
| 1 | 2 | 3 | ||
| Blood Transfusion | 10 | 104 | 1 | 0.001 |
| IV IRON | 0 | 40 | 9 | |
| Total | 10 | 144 | 10 | |
Tab. 3. Type of anemia management vs. score of Hb.
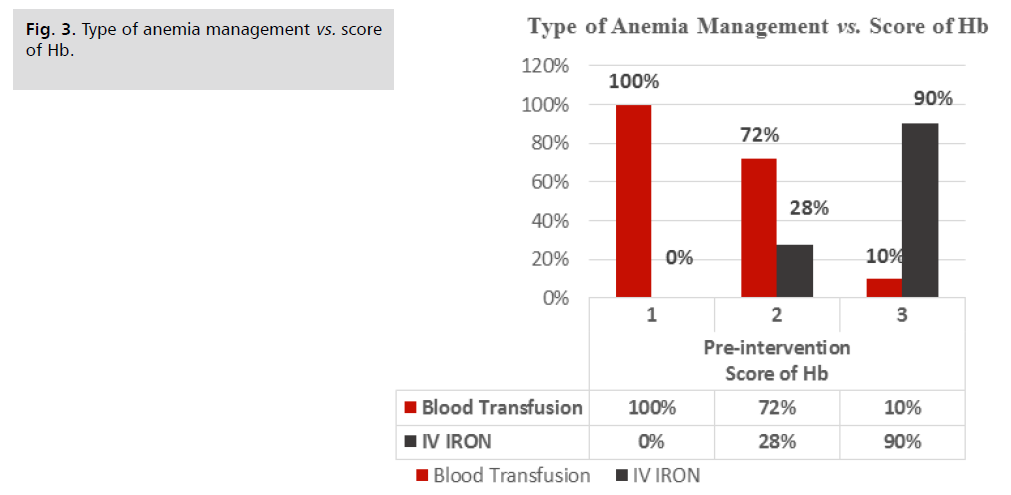
Fig 3. Type of anemia management vs. score of Hb.
Tab. 4. and Fig. 4. information about the correlation between blood transfusions and ABO blood group, and Rh factor (positive or negative) as well as the distribution of blood transfusions by type of blood and Rh factor.
| Blood Transfusion association with ABO & Rh | Rh | ||||
|---|---|---|---|---|---|
| Rh-ve | Rh+ve | Total | P-value | ||
| ABO | A | 4 | 49 | 53 | 0.270 |
| AB | 3 | 10 | 13 | ||
| B | 3 | 35 | 38 | ||
| O | 2 | 33 | 35 | ||
| Total | 12 | 127 | 139 | ||
Tab. 4. The distribution of blood transfusion with ABO & Rh.
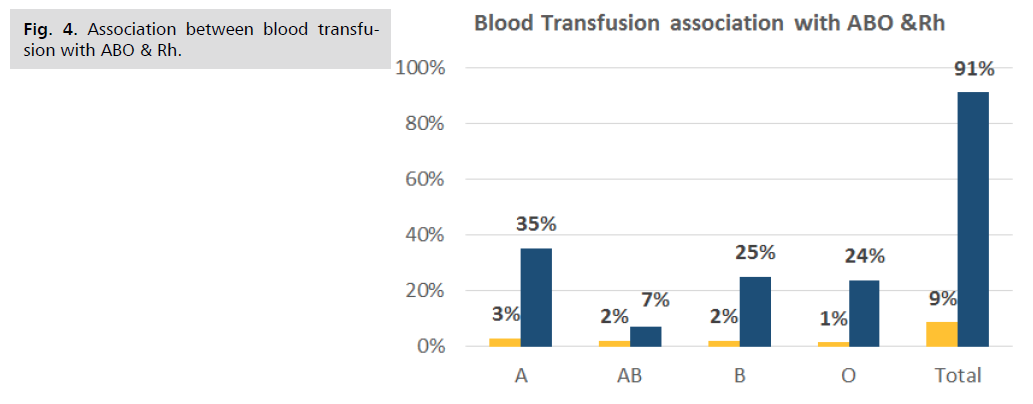
Fig 4. Association between blood transfusion with ABO & Rh.
Tab. 5. and Fig. 5. shows the distribution of intravenous iron doses given to pregnant women with varying Hb scores, which indicate the severity of anemia; the doses were 1 amp, 2 amps, and 3 amps.
| Dose of IV IRON & Score of Hb | Dose of IV IRON | |||||
|---|---|---|---|---|---|---|
| 1 amp | 2 amp | 3 amp | Total | P-value | ||
| Score of Hb | 1 | 0 | 2 | 6 | 8 | 0.339 |
| 2 | 1 | 17 | 16 | 34 | ||
| 3 | 1 | 2 | 4 | 7 | ||
| Total | 2 | 21 | 26 | 49 | ||
Tab. 5. Dose of IV IRON & Score of Hb.
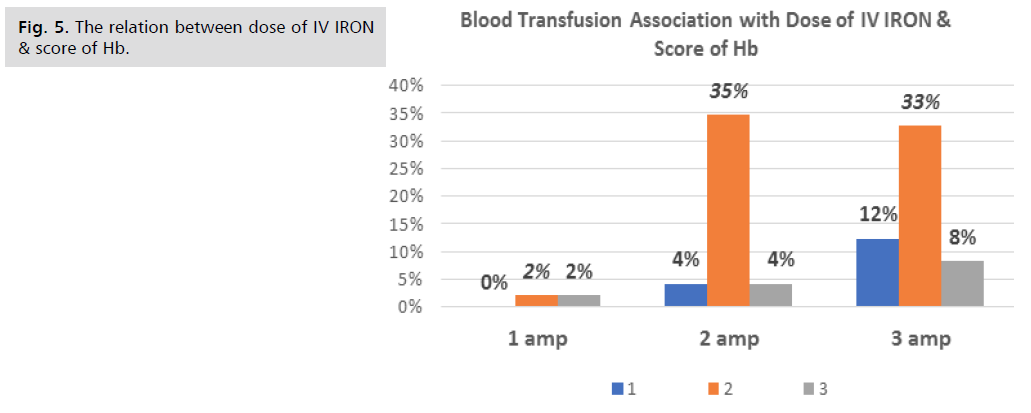
Fig 5. The relation between dose of IV IRON & score of Hb.
Discussion
Many persons with anemia go undiagnosed because the symptoms are subtle or hard to pin down. Anemia or its underlying cause may be the source of the symptoms [19].
For each of the three anemia types “macrocytic, microcytic, and normocytic”, Tab. 1. and Fig. 1. compares the two main methods of treatment: blood transfusion and intravenous iron. A blood transfusion was necessary in the only (1) instance of macrocytic anemia. Intravenous iron did not handle any instances. Microcytic anemia accounts for (98) of the total cases, making it the most common kind of anemia. Blood transfusions were used to address (66) instances, whereas intravenous iron was used to handle (32) cases. The number of instances with normocytic anemia is (14). Iron was administered intravenously in (6) instances and blood transfusions in (8). P-value obtained from the chi-squared test is approximately 0.582. Given their high occurrence, blood transfusion and intravenous iron are acceptable treatments for managing microcytic anemia patients. The use of blood transfusions, nevertheless, seems to be increasingly prevalent which is not acceptable due to it is resulting from (IDA) which may easily managed by iron supplement or iv iron with no need for risk of transfusion of blood.
Anemia during pregnancy may be categorized according to its the level of severity and the degree of hemoglobin (Hb) as shown in Tab. 2. and Fig. 2. according to “American society of Hematology ASH”.
Depending on the severity of the problem, the findings clearly show that anemia care options varies. as seen in Tab. 3 and Fig. 3. the rapid correction of hemoglobin levels is likely the driving factor behind the high prevalence of blood transfusions in cases of severe and moderate anemia. Whereas intravenous iron is more often used for moderate anemia, it provides a safer and more effective option for less severe instances. Setting techniques for managing anemia based on the severity of the ailment is crucial for optimizing patient outcomes, as shown by the statistically significant variation in treatment distribution that the p-value was (0.001). Managing Hemoglobin (Hb) levels may help reduce the likelihood of unfavorable pregnancy outcomes. Researchers have found mixed results when looking at the link between maternal hemoglobin levels and complications during pregnancy, such as Low Birth Weight (LBW), Premature Labor (PTB), and perinatal fatality [20].
In Tab. 4. and Fig. 4. the information set offers insight into the occurrence of blood transfusions according to various ABO and Rh factors. Corresponding with the distribution of the general population, Rh-positive transfusions are rather frequent, with Blood Group A being a particularly prevalent recipient group. This information highlights the need of having a diversified and sufficient blood supply to fulfill the transfusion requirements of patients with different Rh factors and blood types.
Despite the link between a mother's anemia and unfavorable obstetrical consequences, there is still no consensus on what hemoglobin count is ideal for minimizing the need for blood transfusions during childbirth. A mother's risk of packed red blood cell transfusion and postpartum readmission was five times greater if she had anemia before giving birth, but this risk did not extend to other perinatal complications. Peripartum transfusion rates may be decreased by enhancing predelivery hemoglobin, especially if it is at least 10.6 g/dL [21]. As in Tab. 5. and Fig. 5. they showed how various kinds of anemia are managed with the judicious use of intravenous iron. Given the prevalence of mild anemia, it is obvious that patients need extensive iron replacement, with dosages adjusted according to their specific requirements. Cases of mild anemia are treated with lesser dosages to prevent iron overload and promote a progressive repair, that is against the approach of ASH guidelines which are recommend the dose does not below or exceed (200 mg) in one session.
Conclusion
Because of its subtle symptoms, anemia during pregnancy is often misdiagnosed. Iron Deficiency Anemia (IDA) is treated more safely with intravenous iron (33%), but blood transfusions (67% of cases) are commonly used for microcytic anemia (98% of cases). Treatment options for maternal anemia vary according to its severity; moderate cases are best treated with intravenous iron, while severe cases often require blood transfusions. Reducing the need for perinatal transfusions by as much as 80% is possible with improved maternal Hemoglobin (Hb) levels. Different ABO and Rh factors necessitate a diverse blood supply. To effectively manage anemia, it is essential to adhere to ASH guidelines, particularly those pertaining to iron dosage.
Authors’ Contribution
(A) Study Design · (B) Data Collection · (C) Statistical Analysis · (D) Data Interpretation · (E) Manuscript Preparation · (F) Literature Search · (G) No Fund Collection
References
- Turawa E, Awotiwon O, Dhansay MA, et al. Prevalence of anaemia, iron deficiency, and iron deficiency anaemia in women of reproductive age and children under 5 years of age in south africa (1997–2021): A systematic review. Int J Environ Res Public Health. 2021;18(23):12799.
- Petraglia F, Dolmans MM. Iron deficiency anemia: Impact on women’s reproductive health. Fertil Steril. 2022;118(4):605-606.
- Cappellini MD, Santini V, Braxs C, et al. Iron metabolism and iron deficiency anemia in women. Fertil Steril. 2022;118(4):607-614.
- Tang GH, Sholzberg M. Iron deficiency anemia among women: An issue of health equity. Blood Rev. 2023:101159.
- Halfon P, Penaranda G, Ringwald D, et al. Laboratory tests for investigating anemia: From an expert system to artificial intelligence. Pract Lab Med. 2024;39:e00357.
- Milovanovic T, Dragasevic S, Nikolic AN, et al. Anemia as a problem: GP approach. Dig Dis. 2022;40(3):370-375.
- Cacoub P, Choukroun G, Cohen-Solal A, et al. Towards a common definition for the diagnosis of iron deficiency in chronic inflammatory diseases. Nutrients. 2022;14(5):1039.
- Harrison RK, Lauhon SR, Colvin ZA, et al. Maternal anemia and severe maternal morbidity in a US cohort. Am J Obstet Gynecol. 2021;3(5):100395.
- JP AK, Somannavar MS, George N. Efficacy of iron treatments on hemoglobin and ferritin levels in iron deficient pregnant women: Systematic review and meta-analysis. Clin Epidemiol Glob Health. 2023:101375.
- Avni T, Bieber A, Grossman A, et al. The safety of intravenous iron preparations: systematic review and meta-analysis. InMayo clinic proceedings 2015; 90:12-23.
- Surbek D, Vial Y, Girard T, et al. Patient Blood Management (PBM) in pregnancy and childbirth: literature review and expert opinion. Arch Gynecol Obstet. 2020;301:627-641.
- Kanu FA. Anemia among pregnant women participating in the special supplemental nutrition program for women, infants, and children—United States, 2008–2018. Morb Mortal Wkly Rep. 2022;71.
- Marley A, Brookes MJ. Iron deficiency anaemia–modern investigation and management. Medicine. 2023.
- Inam-ul-Haq MA, Anwar B, Saleem MA. Hematological Profile of healthy pregnant females in association with parity. J Rawal Med Coll. 2013;17(1).
- Singh P, Singh S. Topesh. Hematological parameters in anaemic pregnant women attending the antenatal clinic of tertiary care hospital. Int J Res Health Sci. 2014;2(4):981-986.
- Arika WM, Nyamai DW. Hematological markers of in vivo toxicity. J Hematol Thrombo Dis. 2016;4(02):1.
- Chaudhari SJ, Bodat RK. Tracking of Haematological Parameters In First And Second Trimester Of Pregnancy. Natl J Med Res. 2015;5(03):259-261.
- Okebe J, Mwesigwa J, Agbla SC, et al. Seasonal variation in haematological and biochemical reference values for healthy young children in The Gambia. BMC Pediatrics. 2016;16:1-8.
- Ghafel N. Association of the blood groups with mostly public Diseases. Kufa J Nurs Sci. 2021;11(1):263-275.
- Burden CA, Smith GC, Sovio U, et al. Maternal hemoglobin levels and adverse pregnancy outcomes: individual patient data analysis from 2 prospective UK pregnancy cohorts. Am J Clin Nutr. 2023;117(3):616-624.
- Cozzi GD, Blanchard CT, Szychowski JM, et al. Optimal predelivery hemoglobin to reduce transfusion and adverse perinatal outcomes. Am J Obstet Gynecol. 2023;5(2):100810.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Author Info
Maryam K. Alaasam* and Nagham Yahya GhafilCopyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.