Original Article - (2021) Volume 16, Issue 3
Effect of Labor Epidural Analgesia on Delivery of Second Twin: A Prospective Observational Study
Mohamed M. Farghali1,2*, Abdelrady S. Ibrahim3 and Waleed S. Farrag3Received: 16-Aug-2021 Published: 28-Sep-2021
Abstract
Background: The delivery of the second twin remains a challenging issue, and the perinatal mortality rate was significantly higher for the retained second twins compared to the unretained second twins. There is no published data regarding the effect of epidural analgesia on delivery of second twin.
Objectives: To evaluate the effect of epidural analgesia on delivery of second twin.
Methods: 343 Women with twin pregnancies planned for trial of vaginal delivery from January 2014 to December 2019 were included in this prospective study. Studied women received lumbar epidural analgesia while parturient in control group received remifentanil intravenous patient-controlled analgesia (IV-PCA) as the insertion of epidural catheter was contraindicated as labor analgesia in this group.
According to the mode of delivery of first twin and second twin, participants were classified into; vaginal delivery/vaginal delivery (V/V) group (both twins delivered vaginally), cesarean section/ cesarean section (C/C) group (both twins delivered by cesarean section (CS)), and vaginal delivery/cesarean section (V/C) group (first twin delivered vaginally and second twin delivered by CS). After delivery, the maternal age, parity, gestational age, chorionicity of the twin pregnancies, mode of delivery, fetal weight, and complications associated with labor analgesia were collected to evaluate effect of epidural analgesia on delivery of second win.
Results: This study found that the risk of requiring delivery by CS for both twins is significantly reduced (P<0.001) if an epidural was used (OR 0.0435; 95%CI:0.022-0.083). Risk of combined V/C for delivery of second twin was significantly reduced if an epidural was used (OR 0.380; 95% CI: 0.163-0.883), (P<0.001).
Conclusion: The use of epidural analgesia in twin pregnancies reduces the CS rate for delivery of both twins and reduces the rate of combined V/C for delivery of second twin. Further future studied are needed to confirm our study findings.
Keywords
Epidural analgesia; Second, Twin; Cesarean section; Vaginal delivery
Introduction
Twin deliveries constitute 2-3% of all deliveries [1]. The route of delivery is the main controversy in intrapartum management of twin pregnancies [2]. It is critically important to decide the delivery route in twin pregnancies to optimize maternal and fetal outcomes [3]. The delivery route in twin pregnancies either vaginally or cesarean delivery varies between institutions [4,5].
There is general agreement favouring vaginal delivery for vertex-vertex twin pregnancies [6]. A randomized trial (RCT) showed that vaginal delivery in uncomplicated twin pregnancies after 32 gestational weeks is possible and safe if the first twin was in cephalic position [7]. Therefore, it is recommended to counsel women with uncomplicated twin pregnancy after 32 weeks for vaginal delivery if the first twin is in cephalic presentation [8].
Nevertheless, the delivery of the second twin remains a challenging issue, and a retrospective study showed increased risk of perinatal mortality for the second twin [9]. Active second stage management for the second twin is associated with better neonatal outcome and low rate of combined vaginal-cesarean delivery [10].
The perinatal mortality rate was significantly higher for the retained second twins (258/1000) compared to the unretained second twins [11]. Apgar scores were lower for retained than unretained second twins [12]. Early recognition of twin pregnancies in which the 2nd twin is more likely to be retained and prompt appropriate measures would reduce the incidence of retained second twin and its consequences [11].
Grobman et al, found strong association between time of epidural administration and cesarean sections (CS) during twin deliveries in nulliparous women [6].
Epidural analgesia is one of the best pain management procedures, commonly used during labor [13]. Despite its effectiveness, the use of epidural analgesia carries some risks [14] including hypotension. fever, prolonged labor, increased need for oxytocin, labor dystocia and instrumental delivery [15,16].
The intrapartum risk factors associated with increased risk of CSs in twin pregnancies were studied previously [17], and there is no published data regarding the effect of epidural analgesia on delivery of second twin. Therefore, this study was designed to evaluate effect of epidural analgesia on delivery of second win.
Materials and Methods
This prospective study was conducted in the Obstetrics and Gynecology department of Sabah Maternity hospital, Kuwait, after approval of the study by the local ethical committee of Obstetrics and Gynecology department and trial registration (ClinialTrials.gov ID: NCT04608006). The Sabah Maternity Hospital is a tertiary care hospital for the country of Kuwait with approximately 12.500 deliveries per year.
Women with twin pregnancies planned for trial of vaginal delivery from January 2014 to December 2019 were included in this prospective study, after informed consent in accordance with the Declaration of Helsinki.
Inclusion criteria include twin pregnancies >34 weeks` gestation calculated from first day of last menstrual period and confirmed by an early ultrasound scan, without previous uterine scars, both twins are viable, and both are vertex presentation (according to hospital protocol vaginal delivery is allowed only when both twins are vertex).
Women with second twin presentation is other than vertex presentation (breech presentation, or transverse lie), require induction of labor, ≥25% difference in fetal weight between first and second twin or one of the twins is stillborn or has major congenital malformations were excluded from this study.
Parturients in the study group received lumbar epidural analgesia while Parturients in control group received remifentanil intravenous patient-controlled analgesia (IV-PCA) when the insertion of epidural catheter was contraindicated as labor analgesia. The criteria of epidural-contraindication include patient refusal, active maternal hemorrhage, septicemia, infection at or near the site of needle insertion and clinical signs of coagulopathy.
Lumbar epidural analgesia was performed by senior anesthetists with more than 5 years’ experience in the field with more than 100 epidural procedures when active phase of labor starts according to the hospital protocol.
Patient was placed in the sitting position, the skin over the lumbar area was cleaned, a sterile drape was applied, and sterile technique was maintained throughout the procedure. Skin and subcutaneous tissue were infiltrated with 3 ml of lidocaine 1% at the intended site of epidural placement.
The lumbar epidural space was located with 18-gauge Tuohy epidural needle using the loss of resistance technique with 2 mL of saline. A 20-gauge epidural catheter (Luer B, Braun, Germany) was placed for all participants following localization of lumbar epidural space.
Lumbar epidural analgesia produces a selective sensory block from T10 to L1, while at the same time sparing the motor supply to the lower limbs (L2-L5).
Initially a 10 ml bupivacaine (0.125%) (ADVANZ Pharma, UK) plus 50 ug fentanyl (Hameln pharma ltd, UK), were injected through the epidural catheter as bolus injection followed by continuous infusion of bupivacaine 0.125% plus 1 ug/ml fentanyl over 6-10 ml/hours.
When the insertion of epidural catheter was contraindicated, remifentanil IV-PCA was given for the studied women as labor analgesia using remifentanil 20 ug/ml (Hospira Ltd, UK) at rate of 20 ug increased gradually up to 50 ug in high dependency unit (HDU) under monitor of vital data (respiratory rate, pulse, blood pressure), urine output, and cardiotocography (CTG).
Labor pains were scored before, and after labor analgesia using VAS (visual analogue score), (0 = no pain and 10 = worst pain). Breakthrough pain was defined as maternal pain or pressure that required one or more doses of unscheduled labor analgesia medications.
According to the mode of delivery of first twin and second twin, participants were classified into 3 delivery groups; vaginal delivery/vaginal delivery (V/V) group (both twins delivered vaginally), cesarean section/ cesarean section (C/C) group (both twins delivered by CS), and vaginal delivery/cesarean section (V/C) group (first twin delivered vaginally and second twin delivered by CS).
After delivery, the maternal age, parity, gestational age, chorionicity of the twin pregnancies (monochorionic or dichorionic twins), mode of delivery, fetal weight, and complications associated with labor analgesia (headache, backache, nausea/vomiting, itching, urinary retention, and neural deficit) were collected to evaluate effect of epidural analgesia on delivery of second win.
Sample size
Three hundred and forty-three (343) twin pregnancies were included in the study. The required sample size was calculated from previous studies [18] and using G Power software 3.1.9.7 for sample size calculation, setting α -error probability at 0.05, power at 0.95%, and effective sample size (w) at 0.5. An effective sample >210 twins’ deliveries (105 in each group) were needed to produce a statistically acceptable figure.
Statistical analysis
Collected data were statistically analyzed using Statistical Package for Social Sciences (SPSS): computer software version 20 (Chicago, IL, USA). Numerical variables were presented as mean and standard deviation (±SD), while categorical variables were presented as number (n) and percentage (%). Chi-square test (x2) or Fisher exact was used for analysis of qualitative variables, while Student (t) test were used for analysis of quantitative variables. Yates’ correction was applied to tables with one or more cells with expected frequency less than five. Multivariate logistic regression test was used to calculate the odds ratio for different clinical data collected before delivery as independent factors and mode of delivery as a dependent factor. P< 0.05 was considered significant.
Results
Three hundred and forty-three (343) twin pregnancies at ≥34 weeks` eligible for vaginal delivery were included in this study, 67.3% (231/343) of them received epidural analgesia, and 32.7% (112/343) received remifentanil IV-PCA.
Regarding the delivery mode, 68.8% (236/343) of the participants’ delivered both twins vaginally, while the total incidence of CS was 31.2% (107/343), 9.3% (32/343) of the CSs were performed for delivery of the second twin after vaginal delivery (VD) of the first twin (Fig. 1.).
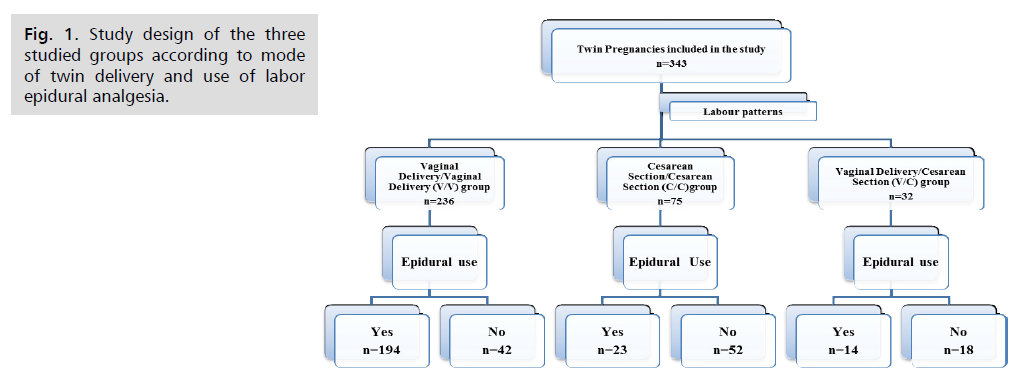
Figure 1: Study design of the three studied groups according to mode of twin delivery and use of labor epidural analgesia.
There was no significant difference between the three delivery groups regarding, the mean maternal age, gestational age, parity, and chronicity (Tab. 1.).
| Variables | V/V group (n = 236) |
C/C group (n = 75) |
V/C group (n= 32) |
VV/CC | CC/VC | VV/VC |
|---|---|---|---|---|---|---|
| P1 | P2 | P3 | ||||
| Parturient Age (years) | 31.6 ± 5.7 | 29.8 ± 5.4 | 31.3 ± 4.7 | 0.99 | 0.98 | 0.5 |
| Gestational age (weeks) | 35.3 ± 1.5 | 35.8 ± 1.7 | 36.0 ± 1.5 | 0.5 | 0.99 | 0.99 |
| Parity | 1.7 ± 0.8 | 2.1 ± 0.9 | 1.8 ± 0.9 | 0.5 | 0.5 | 0.5 |
| Chorionicity M/D | 55/181 | 16/59 | 7/25 | 0.95 | 0.72 | 0.85 |
Chorionicity M/D: Monochorionic twins/ Dichorionic twins
Comparison between groups by using student t test
Data were expressed as mean ± standard deviation (SD)
V/C group: Vaginal Delivery/Cesarean Section group
V/V group: Vaginal Delivery/Vaginal Delivery group
Tab. 1. Demographic and clinical data of the three delivery groups.
As shown in table 1, there was no significant difference between the gestational age ranges of the three delivery groups. In C/C 34/75 (45.3%) of the women delivered between 34- and 35-weeks’ gestation compared with 17/32 (53.1%) in the V/C group. The main indication for CS in the C/C group was fetal distress [35 (46.6%) of either first twin or second twin], cervical dystocia or failure to progress in 25 (33.33%), prolonged latent phase in 7 (9.3%), cord prolapse in 5 (6.6%), and 3 CSs were done for non-medical reasons.
In this study, we tried to exclude factors affecting mode of twins’ delivery, however, the relationship between some intrapartum factors in both the C/C group and V/C group was presented (Tab. 2. and Fig. 2.).
| Variables | Parity | Epidural use | Birth weight difference | |||
|---|---|---|---|---|---|---|
| Nulliparous | Multiparous | Yes | No | <10% | ≥10% | |
| n=178 (51.9%) | n=165 (48.1%) |
n=267 (77.8%) | n=76 (22.2%) | n=301 (78.7%) | n=42 (12.3%) |
|
| Incidence of C/C group | 48 (13.9%) | 27 (7.8%) | 23 (6.7%) | 52 (15.1%) | 58 (16.9%) | 17 (5.0%) |
| P-value | <0.0001* | <0.0001* | <0.0001* | |||
| Incidence of V/C group | 19 (5.5%) | 13 (3.8%) | 14 (4.1%) | 18 (5.2%) | 11 (3.2%) | 21 (6.1%) |
| P-value | <0.0001* | <0.0001* | <0.0001* | |||
C/C group: Cesarean Section/Cesarean Section group
Data presented as number and percentage (%)
V/C group: Vaginal Delivery/Cesarean Section group
Tab. 2. Intrapartum factors and the incidence of caesarean section in twin pregnancies.
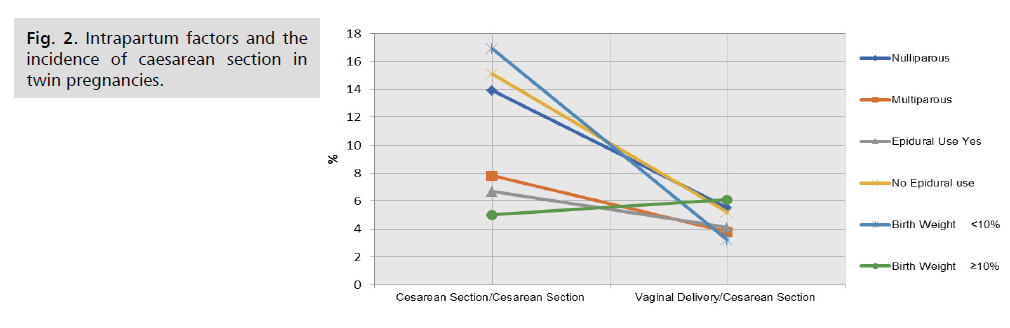
Figure 2: Intrapartum factors and the incidence of caesarean section in twin pregnancies.
This study found that the risk of requiring delivery by CS for both twins is significantly reduced (P<0.001) if an epidural was used (OR 0.0435; 95%CI:0.022-0.083). The second twin was less likely to be delivered by CS after VD of the first twin if an epidural labor analgesia used (OR 0.380; 95%CI: 0.163-0.883), (P< 0.001) (Tab. 3.).
| Variables | Parity | Epidural use | Birth weight difference | |||
|---|---|---|---|---|---|---|
| Nulliparous | Multiparous | Yes | No | <10% | ≥10% | |
| n=178 (51.9%) | n=165 (48.1%) |
n=267 (77.8%) | n=76 (22.2%) | n=301 (78.7%) | n=42 (12.3%) |
|
| Incidence of C/C group | 48 (13.9%) | 27 (7.8%) | 23 (6.7%) | 52 (15.1%) | 58 (16.9%) | 17 (5.0%) |
| P-value | <0.0001* | <0.0001* | <0.0001* | |||
| Incidence of V/C group | 19 (5.5%) | 13 (3.8%) | 14 (4.1%) | 18 (5.2%) | 11 (3.2%) | 21 (6.1%) |
| P-value | <0.0001* | <0.0001* | <0.0001* | |||
C/C group: Cesarean Section/Cesarean Section group
Data presented as number and percentage (%)
V/C group: Vaginal Delivery/Cesarean Section group
Tab. 3. Association between different clinical data and route of delivery.
This study showed that the CS after VD was associated with good outcome for the second twin. The incidence of 1st min. Apgar score <4 was reported in 19 (25.3%) of first twin and in 20 of the second twin (26.6%) in C/C group, while it was reported in 0 (0%) for the first twin and in 4 (12.5%) of the second twin in the V/C group (P=0.04). No fetal death or neonatal injuries were recorded in this study.
Discussion
The current guidelines suggest the VD as an appropriate mode of delivery for twin pregnancy when both twins have appropriate estimated weight, the first twin in vertex presentation and no contraindications for VD [19-21]. A group of twin pregnancies at >34 weeks` gestation were included in this study because of the hospital policy which allows vaginal delivery for twin pregnancies only after 34 weeks` gestation.
Chervenak et al. found the multiple gestations have a 25-30% incidence of CS [5], and Grobman et al, reported 18.7% CS rate while reviewing 134 sets of twins undergoing trial of labour (TOL) at 36 weeks` gestation [6].
In this study, the total incidence of CS was 107/343 (31.2%), 9.3% (32/343) of them were performed for the delivery of the second twin by cesarean section after vaginal delivery of first twin.
Grobman et al, reported that women who delivered by CS were more likely to be nulliparous, have less cervical dilation on admission, epidural placement, and higher mean oxytocin infusion. In addition, Grobman et al, found the time of epidural analgesia, and nulliparity were most strongly associated with CS [6].
Similarly, in this study the CS rate was higher for nulliparous compared to multiparous women (13.9% versus 7.8%, respectively).
The association between nulliparity and failed trial of vaginal delivery in twin gestation was previously established but, was not assessed separately for combined delivery and cesarean delivery of both twins [22-24].
Goyert et al, previously concluded that the variation in cesarean section rates among physicians was not attributable to the practice setting, the patient population, or the degree of obstetric risk, but to individual practice style [25]. In this study, the physician experience was not a critical factor for determining the incidence of the cesarean section rate in twins.
Previous studies suggested that if the second twin was significantly larger than the first, cesarean delivery should be considered [5,26]. Sullivan et al, investigated the birth weight discordance of > 20%, and reached the same conclusion [27]. Th this study, women with birth weight discrepancy > 25% between the first and second twins were excluded.
Cesarean delivery of the second twin after vaginal delivery of the first twin was extremely uncommon, but now occurs much more frequently. The reported incidence of combined twin delivery ranges between 5% and 10% [28]. These estimates are based mostly on small studies or retrospective data. Sullivan et al, reported a 17% rate of cesarean delivery of the second twin after vaginal delivery of the first twin [27], while the reported incidence of cesarean delivery of second twin after vaganial delivery of the first twin in this study was 9.3%.
Previous studies described cord prolapse as the most significant factor for combined V/C deliveries (35-50%), while arrest disorders accounted for the majority of unplanned cesarean delivery in other studies [28,29].
In contrast with previous studies, most of the unplanned cesarean deliveries in this study were due to non-reassuring fetal heart rate (48% in the C/C group and 37.5% in the V/C group). Other common indications were arrest of dilatation (33.3%) in the C/C group and arrest of descent (28.1%) in the combined V/C group.
Mei et al, studied 725 women of planned vaginal deliveries for twin pregnancies, and reported 32.7% successful vaginal deliveries for both twins, and conversion to 10 of planned vaginal deliveries (4.2%) [30]. Mei et al, found that the conversion from vaginal deliveries to cesarean sections were higher with spontaneous labor (OR: 2.1; 95%CI: 1.6-2.7; P=0.003), and with an inter-twin delivery interval >60 min. (OR:5.1; 95%CI: 2.5-10.8; P< 0.001), while, the delivery provider and years in practice were not significantly affect the conversion rate [30].
About 2786 women were included in the Twin Birth Study to evaluate the incidence and risk factors for combined V/C delivery in twin pregnancies, 842 women delivered first twin by vaginal delivery, of them 59 (7%) had a combined V/C delivery. Women in the combined V/C delivery group had a lower rate of nulliparity (22.0% versus 34.7%, P=0.047) and higher rates of non-cephalic presentation for the second twin (61.0% versus 27.3%, P<0.001). In a multivariable model, the only risk factor significantly associated with combined V/C delivery was transverse/oblique lie of second twin following delivery of first twin (AOR, 47.7; 95% CI: 15.4-124.5) [31].
In our hospital, the rate of epidural analgesia during labour is greater than 70% since we have a full-time anaesthesiologist available for the Obstetrics department. In this study, 267 from 343 parturient (77.8%) received epidural analgesia, while the remaining received remifentanil IV-PCA, and 236/343 (68.8%) delivered both twins vaginally.
The most relevant outcomes in this study were the epidural analgesia which not an independent risk factor for CS for both twins, but it was independent risk factor for combined V/C twin delivery. In this study, we found that epidural placement at a cervical dilation of ≥4cm was associated with significant improvement in the vaginal delivery rate. Grobman's et al, found that the timing of the epidural placement at less than 3 cm increased the CS rate to 44% [6].
Although, this study concluded that CS after vaginal delivery was associated with a good outcome for the second twin. The Twin Birth Study concluded that combined V/C delivery was associated with higher risk of adverse neonatal outcomes for the second twin. The second twin in the combined V/C delivery had a higher rate of fetal/neonatal death or serious neonatal morbidity (13.6% versus 2.3%; P<0.001) including 5th min. Apgar score <7, neonatal intensive care unit (ICU) admission, abnormal level of consciousness, and assisted ventilation [31]. The data of the Twin Birth Study should be used for counselling of women with twin gestation who consider a trial of labour [31].
To our knowledge, this study is first prospective study conducted in Kuwait including (343) to evaluate the effect of epidural analgesia on delivery of second twin (most of previous studies were retrospective studies). Women refused to participate and/or give consent was the only limitation faced during this study.
This study found that the risk of requiring delivery by CS for both twins is significantly reduced (P<0.001) if an epidural was used (OR: 1.85; 95%CI: 0.788-4.35). Risk of combined V/C for delivery of second twin was significantly reduced if an epidural was used (OR: 0.380; 95% CI: 0.163-0.883), (P<0.001).
This study concluded that in twin pregnancies; the use of epidural analgesia reduces the CS rate for delivery of both twins and reduces the rate of combined V/C for delivery of second twin. Further future studied are needed to confirm our study findings.
Conclusion
The use of epidural analgesia in twin pregnancies reduces the CS rate for delivery of both twins and reduces the rate of combined V/C for delivery of second twin. Further future studied are needed to confirm our study findings.
Ethical Consideration
The study was approval by the ethical committee of Obstetrics and Gynecology department of Maternity hospital, Kuwait, informed consents were obtained from participants in accordance with the Declaration of Helsinki. The study was registered as clinical trial ClinialTrials.gov ID: NCT04608006).
Conflicts of Interest
Authors declare no conflicts of interest related to this article.
Financial Disclosure
Nil.
References
- Martin JA, Park MM. Trends in twin and triplet births: 1980-97. Natl Vital Stat Rep. 1999;47(24):1-16.
- Warenski JC, Kochenour NK. Intrapartum management of twin gestation. Clin Perinatol. 1989;16(4):889-97.
- Bowes WA Jr, Taylor ES, O'Brien M, et al. Breech delivery: evaluation of the method of delivery on perinatal results and maternal morbidity. Am J Obstet Gynecol. 1979;135(7):965-73.
- Benachi A, Pons JC. Is the route of delivery a meaningful issue in twins? Clin Obstet Gynecol. 1998;41(1):30-5.
- Chervenak FA, Johnson RE, Berkowitz RL, et al. Is routine cesarean section necessary for vertex-breech and vertex-transverse twin gestations? Am J Obstet Gynecol. 1984;148(1):1-5.
- Grobman WA, Dooley SL, Peaceman AM. Risk factors for cesarean delivery in twin gestations near term. Obstet Gynecol. 1998;92(6):940-4.
- Asztalos EV, Hannah ME, Hutton EK, et al. Twin Birth Study: 2-year neurodevelopmental follow-up of the randomized trial of planned cesarean or planned vaginal delivery for twin pregnancy. Am J Obstet Gynecol. 2016;214(3):371.e1-371.e19.
- Macones GA, Peipert J, Nelson DB, et al. Maternal complications with vaginal birth after cesarean delivery: a multicenter study. Am J Obstet Gynecol. 2005;193(5):1656-62.
- Sheay W, Ananth CV, Kinzler WL. Perinatal mortality in first- and second-born twins in the United States. Obstet Gynecol. 2004;103(1):63-70.
- Fox NS, Silverstein M, Bender S, et al. Active second-stage management in twin pregnancies undergoing planned vaginal delivery in a U.S. population. Obstet Gynecol. 2010;115(2 Pt 1):229-233.
- Adinma JI, Agbai AO. The second twin: retained and unretained. Trop Doct. 1995;25(3):132-3.
- Aniebue UU, Ezegwui HU, Ozumba BC. Retained second twins in Enugu, Nigeria. Int J Gynaecol Obstet. 2003;81(3):281-5.
- Rawal N. Epidural technique for postoperative pain: gold standard no more? Reg Anesth Pain Med. 2012;37(3):310-7.
- Zhang J, Klebanoff MA, DerSimonian R. Epidural analgesia in association with duration of labor and mode of delivery: a quantitative review. Am J Obstet Gynecol. 1999;180(4):970-7.
- Leighton BL, Halpern SH. The effects of epidural analgesia on labor, maternal, and neonatal outcomes: a systematic review. Am J Obstet Gynecol. 2002;186(5 Suppl Nature):S69-77.
- Alexander JM, Sharma SK, McIntire DD, et al. Epidural analgesia lengthens the Friedman active phase of labor. Obstet Gynecol. 2002;100(1):46-50.
- Hofmeyr GJ, Barrett JF, Crowther CA. Planned caesarean section for women with a twin pregnancy. Cochrane Database Syst Rev. 2011;7(12):CD006553.
- Agrawal D, Makhija B, Arora M, et al. The effect of epidural analgesia on labour, mode of delivery and neonatal outcome in nullipara of India, 2011-2014. J Clin Diagn Res. 2014;8(10):OC03-6.
- Hofmeyr GJ, Drakeley AJ. Delivery of twins. Baillieres Clin Obstet Gynaecol. 1998;12(1):91-108.
- de Veciana M, Major C, Morgan MA. Labor and delivery management of the multiple gestation. Obstet Gynecol Clin North Am. 1995;22(2):235-46.
- Houlihan C, Knuppel RA. Intrapartum management of multiple gestations. Clin Perinatol. 1996;23(1):91-116.
- Breathnach FM, McAuliffe FM, Geary M, et al. Perinatal Ireland Research Consortium. Prediction of safe and successful vaginal twin birth. Am J Obstet Gynecol. 2011;205(3):237.e1-7.
- Fox NS, Gupta S, Melka S, et al. Risk factors for cesarean delivery in twin pregnancies attempting vaginal delivery. Am J Obstet Gynecol. 2015;212(1):106.e1-5.
- de Castro H, Haas J, Schiff E, et al. Trial of labour in twin pregnancies: a retrospective cohort study. BJOG. 2016;123(6):940-5.
- Goyert GL, Bottoms SF, Treadwell MC, et al. The physician factor in cesarean birth rates. N Engl J Med. 1989;320(11):706-9.
- Blickstein I, Schwartz-Shoham Z, Lancet M, et al. Vaginal delivery of the second twin in breech presentation. Obstet Gynecol. 1987;69(5):774-6.
- Sullivan CA, Harkins D, Seago DP, et al. Cesarean delivery for the second twin in the vertex-vertex presentation: operative indications and predictability. South Med J. 1998;91(2):155-8.
- Olofsson P, Rydhström H. Twin delivery: how should the second twin be delivered? Am J Obstet Gynecol. 1985;153(5):479-81.
- Kurzel RB, Claridad L, Lampley EC. Cesarean section for the second twin. J Reprod Med. 1997;42(12):767-70.
- Mei JY, Muñoz HE, Kim JS, et al. Rates of Cesarean Conversion and Associated Predictors and Outcomes in Planned Vaginal Twin Deliveries. Am J Perinatol. 2020.
- Aviram A, Lipworth H, Asztalos EV, et al. The worst of both worlds-combined deliveries in twin gestations: a subanalysis of the Twin Birth Study, a randomized, controlled, prospective study. Am J Obstet Gynecol. 2019;221(4):353.e1-353.e7.
Author Info
Mohamed M. Farghali1,2*, Abdelrady S. Ibrahim3 and Waleed S. Farrag32Department of Obstetrics and Gynecology, Sabah Maternity hospital, Kuwait
3Department of Anesthesia and Intensive Care Unit, Assiut University, Assiut, Egypt
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.