Research - (2022) Volume 0, Issue 0
Correlation between serum vitamin D3 level and incidence of uterine leiomyoma in Egyptian women: An observational case-control study
Aliaa M. Maaty, Mortada E. Ahmed, Magdy H. Kolaib, Mohamed S. Tolis* and Rania G. El-skaanReceived: 14-Aug-2022, Manuscript No. gpmp-22-71874; Editor assigned: 16-Aug-2022, Pre QC No. P-71874; Reviewed: 30-Aug-2022, QC No. Q-71874; Revised: 14-Sep-2022, Manuscript No. R-71874; Published: 29-Sep-2022
Abstract
Background: Uterine fibroid is thought to be linked to Vitamin D insufficiency.
Objective: To explore the relationship between serum Vitamin D3 levels and uterine fibroids in Egyptian women seeking gynecological services.
Methods: This study was a case-control study conducted at Ain Shams University Maternity Hospital, Gynecology Department during the period from April 2021 to October 2021 on 80 women. Study populations were categorized into 2 groups; the fibroid group included 40 cases having uterine leiomyoma, as well as the control group of 40 cases who were leiomyoma-free women based on transvaginal ultrasound.
Results: While comparing women with uterine fibroids (UFs) to controls, vitamin D levels were significantly lower. (14.80 ± 5.87 vs 23.39 ± 9.11, P <0.001*). The deficiency condition (<20) was more common among the fibroid group than the control (77.5% VS 42.5%, respectively). In the fibroid group (22 %), the proportion of women in the insufficiency range (21–29) was lower than in the control group (25 %). The sufficient condition (30-100) was more common among controls. No case among the fibroid group had a normal vitamin D level. There was no significant relationship between vitamin D level (deficient and insufficient) and age, parity, hemoglobin, body mass index (BMI), size and number of fibroids, complaints, previous intervention, family, and associated gynecological diseases (p >0.05).
Conclusion: Although uterine leiomyomas are more prevalent among Egyptian women with D vitamin deficiency, no association between the vitamin D levels whether it was deficient or insufficient, and UL size and numbers were reported.
Keywords
Uterine leiomyoma; Vitamin D
Introduction
Uterine leiomyoma (UL), often known as uterine fibroids (UFs), has been the most common benign gynecological tumor in the female reproductive system. It is developed mainly from smooth muscle in the uterus [1]. Regarding the general population, the prevalence of UL has been estimated to range from 5 to 69 % [2]. The prevalence of UL rises with age during reproductive years and subsequently falls after menopause [3].
Irrespective of their basically benign neoplastic nature, UFs cause significant comorbidity in female patients, especially in the premenopausal period [4]. Fibroids have been linked to iron deficiency anemia, stomach issues, female pregnancy, or obstetric complications such as abortion and preterm delivery in several studies [5,6].
Even though the cause of fibroids is still unknown, there is a lot of research on the primary factors that cause them, including age, parity, race, obesity, family history, and serum micronutrients [7,8]. It's been debated for the past decade whether Vitamin D insufficiency is linked to the fibroid [9].
Vitamin D (Vit D) is a potent anti-proliferator and immune-modulatory steroid hormone that plays an important function in calcium homeostasis. An active form of Vit D has been shown to influence cellular differentiation, proliferation, malignant invasion, and angiogenesis [10].
It has been proposed that uterine fibroids grow as a result of an improper reaction to tissue healing, which results in altered extracellular matrix production, and that vitamin D can help to reduce this abnormal response by controlling it [11]. Furthermore, Vit D's potential to safely decrease UF lesions in Eker rats, a genuine orthotropic animal model for uterine fibroids, has been proven. These data show that vitamin D could be a potentially helpful therapeutic drug for the nonsurgical treatment of UFs [12].
Regarding a recent review of literature, just a small number of studies looked at Vit D serum levels in patients with ULs. As a result, more studies are needed to create recommendations for vit D screening in women who have UFs or are at greater risk of acquiring UFs.
As a result, the current study's purpose was to investigate the relationship between serum Vit D3 levels and UFs in Egyptian women seeking gynecological care.
Patients and Methods
This was a case-control study undertaken at Ain Shams University Maternity Hospital's Gynecology Department on 80 women with symptomatic UFs who attended the Gynecology outpatient clinic from April to October 2021. Depending on transvaginal ultrasound, the population sample was categorized into two groups:
the fibroid group contained 40 cases with uterine leiomyoma, and the control group included 40 cases who were leiomyoma-free women.
According to our inclusion criteria, which were post-menstrual patients to exclude pregnancy in child bearing period aged from 20 to 45 years to avoid extreme levels of vitamin D , up to para 3, with body mass index ranging from 18 to 30 kg/m2, having one or more subserous, intramural or submucous uterine fibroid with a diameter ranging from 3-10 cm, 125 female patients were enrolled in the study. While we excluded
1) Pregnant or lactating females due to change in fibroids volume during pregnancy in addition to vitamin D levels may be lower than baseline for non pregnant ones and decrease vitamin D levels with lactation.
2) Females with cervical, supracervical or pedunculated fibroids, and small fibroid < 3 cm.
3) Female patients who were suspected of malignant gynecological disease which is usually associated with multiple vitamin deficiency including vitamin D.
4) Females with cardiac, pulmonary, or hematological diseases because of high association between chronic illnesses and multivitamin deficiency.
5) Female patients who received pre-operative hormonal therapy which may increase vitamin D levels and interfere with the study objectives, steroids, vitamin supplement, hormonal therapy during or within 6 months of enrolment.
6) Patients with previous myomectomy or hysterectomy (Fig. 1.).
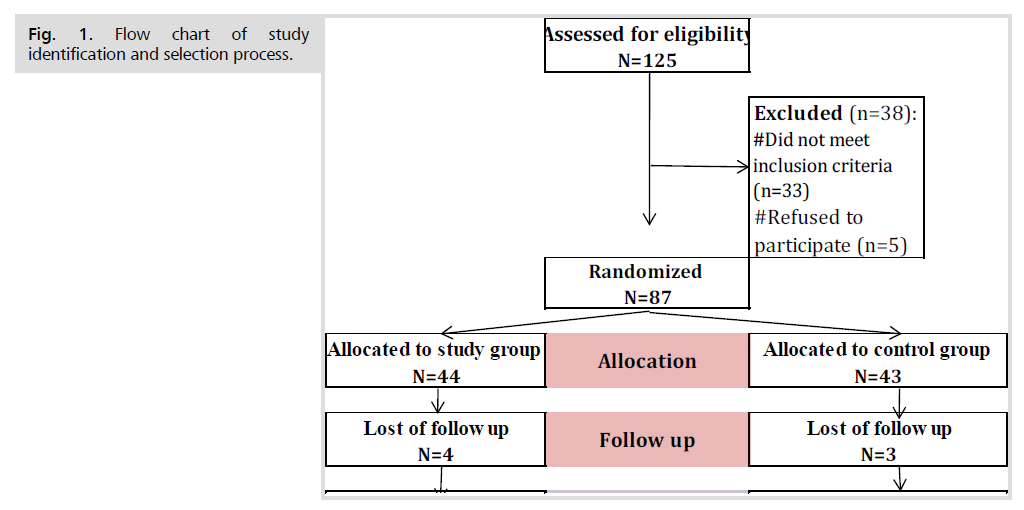
Fig 1. Flow chart of study identification and selection process.
All patients were subjected to detailed history taking, complete clinical examination, and investigations. 2D Ultrasonography was carried out trans-abdominal or trans-vaginal to confirm the exact site, size, and the number of UFs, using MEDISON R5 Ultrasound machine equipped with a 3.5 MHz Convex probe and a vaginal probe.
Laboratory investigation, including complete blood count (CBC), and 25-hydroxy vitamin D3 (25(OH) D3) measurement.
Serum vitamin D level: 25-(OH) D3 was measured to monitor serum vitamin D level. Radioimmunoassay was applied to measure serum Vitamin D3 [25(OH) D3] levels. 25(OH) D3 was evaluated via a direct, competitive chemiluminescence immunoassay. Unit used for laboratory assessment of vitamin D3 level was ng/ml.
Competition principle: The assay took 18 minutes in total.
1st incubation: 25-OH vitamin D3 in the sample (35 μL) competes with vitamin D (the biotin-labelled) in the complex contained in R2 (Ruthenium-labelled specific antibody of biotin-vitamin D and monoclonal 25-OH vitamin D3-). The remaining amount of the complex (Ruthenium-labelled specific antibody of biotin-vitamin D and monoclonal 25-OH vitamin D3-) is determined by the concentration of analyte in the sample.
2nd incubation: The combination of biotin with streptavidin causes the complex to bind to the solid phase.
The reaction mixture is sucked into the measuring cell, where the microparticles are magnetically trapped on the electrode's surface. ProCell is next used to remove any compounds that have not been bound. Chemiluminescent emission is generated when a voltage is supplied to the electrode, which is detected by a photomultiplier. The findings are calculated using a calibration curve.
In this study, we considered low-level serum Vit D is considered lower than 30 ng/ml. Normal Vit D levels are considered when the 25-OH D3 serum level range of 30 - 100 ng/ml, Vitamin D insufficiency (mild decrease) is demarcated when the serum level of 25-OH D3 ranged 21 to 29 ng/ml, Vitamin D deficiency (greater decrease) is known when serum level of 25-OH D3 reach 20 ng/mL or lower.
Ethical Considerations: The ethics committee of the department of obstetrics and gynecology at Ain Shams University's faculty of medicine gave its approval to the study. Before being enrolled in the study, all participants gave their informed written consent after being informed about the study's purpose and procedures.
Number of clinical trial registration: 05151393
Sample Size Justification and Calculation: PASS software (PASS 11). For sample size calculations, (Hintze. J (2011, NCSS, LLC, Kasville, Utah, USA) was employed, as well as a statistical calculator based on a 95 percent confidence interval and study power of 80 percent with a 5 percent error. According to a previous study [13], cases were defined as those who had at least one uterine fibroid larger than 10 mm discovered on ultrasonography, whereas controls were defined as those who did not have any uterine pathology. The sample size was estimated based on these values, and a sample size of 77 cases was sufficient to detect such a difference. The sample size will be 80 cases divided into 40 fibroid cases and 40 healthy controls without fibroid, assuming a drop-out rate of roughly 5% (Fig. 1.).
Statistical analysis of the data: The IBM SPSS software programme version 20.0 was used to examine the data that was supplied into the computer. (IBM Corporation, Armonk, NY). Numbers and percentages were used to describe qualitative data. The Shapiro-Wilk test was done to ensure that the distribution was normal. Range (minimum and maximum), mean, standard deviation, median, and interquartile range were used to characterize quantitative data (IQR). The significance of the acquired results was assessed at a 5% level.
Results
Tab. 1. summarizes the baseline characteristics (1). When compared to the control group, the fibroid group's age and BMI were significantly greater. (p= 0.016, and 0.001, respectively).
| Fibroid (n = 40) | Control (n = 40) | t | p | |
|---|---|---|---|---|
| Age (years) | ||||
| Min. – Max. | 23.0 – 45.0 | 19.0 – 45.0 | t= 2.470* | 0.016* |
| Mean ± SD. | 37.32 ± 5.68 | 33.75 ± 7.18 | ||
| Median (IQR) | 38.0 (34.0 – 41.50) | 33.50 (29.0 – 39.50) | ||
| Parity | ||||
| P0 | 3(7.5%) | 2(5.0%) | χ2= 3.539 | MCp= 0.309 |
| P1 | 6(15.0%) | 7(17.5%) | ||
| P2 | 10(25.0%) | 17(42.5%) | ||
| P>3 | 21(52.5%) | 14(35.0%) | ||
| Min. – Max. | 0.0 – 3.0 | 0.0 – 3.0 | U= 696.0 | 0.284 |
| Mean ± SD. | 2.23 ± 0.97 | 2.08 ± 0.86 | ||
| Median (IQR) | 89.0 | 83.0 | ||
| BMI(kg/m2) | ||||
| Min. – Max. | 27.0 – 33.0 | 20.50 – 31.0 | t= 3.363* | 0.001* |
| Mean ± SD. | 29.23 ± 1.76 | 27.48 ± 2.78 | ||
| Median (IQR) | 29.10 (27.60 – 30.05) | 27.85 (27.35 – 29.10) | ||
Tab.1. Comparison between the two studied groups according to demographic data.
Vitamin D levels were compared in the two studied groups and highly statistically significant differences were found as shown in Tab. 2. Vitamin D level was more deficient in patients with fibroid than controls. Out of 40 cases, 31 women (77.5%) were found to have deficient vitamin D levels while in controls they were 17 women (42.5%). Nine women in the case group (22.5%) were vitamin D insufficient, while 10 women (25%) in the control group were insufficient (Tab. 2.)
| Vitamin D level | Fibroid (n = 40) | Control (n = 40) | Test of Sig. | p | ||
|---|---|---|---|---|---|---|
| No. | % | No. | % | |||
| Deficiency (<20) | 31 | 77.5 | 17 | 42.5 | ||
| Insufficiency (21 – 29) | 9 | 22.5 | 10 | 25.0 | χ2= 17.136* | <0.001* |
| Normal (30 – 100) | 0 | 0.0 | 13 | 32.5 | ||
| Min. – Max. | 5.50 – 27.90 | 8.0 – 51.40 | U= 345.50* | <0.001* | ||
| Mean ± SD. | 14.80 ± 5.87 | 23.39 ± 9.11 | ||||
| Median (IQR) | 13.75 (10.0 – 17.80) | 22.35 (16.15 – 30.75) | ||||
Tab. 2. Comparison between the two studied groups according to vitamin D level.
Hemoglobin level was significantly different among study and control groups, 10.41 ± 0.86 Vs 10.84 ± 0.57 respectively. Using the Ultra-Sound, the mean size of fibroid was 53.55 ± 16.05 mm while the mean number of fibroids was 2.03 ± 1.39 and ranged from 1 to 5.
Complain was significantly different among study and control groups (p<0.001*). The most frequent complaint was AUB in 55% in fibroid group and 40% in control group. 10% in fibroid group and 15% in control group complained from infertility, 12.5% in fibroid group and 15% in control group complained from pelvic heaviness, 22.5% in fibroid group and none in control group complained from pressure symptoms and only control group complained from Urinary incontinence and Vaginal discharge (Fig. 2.).
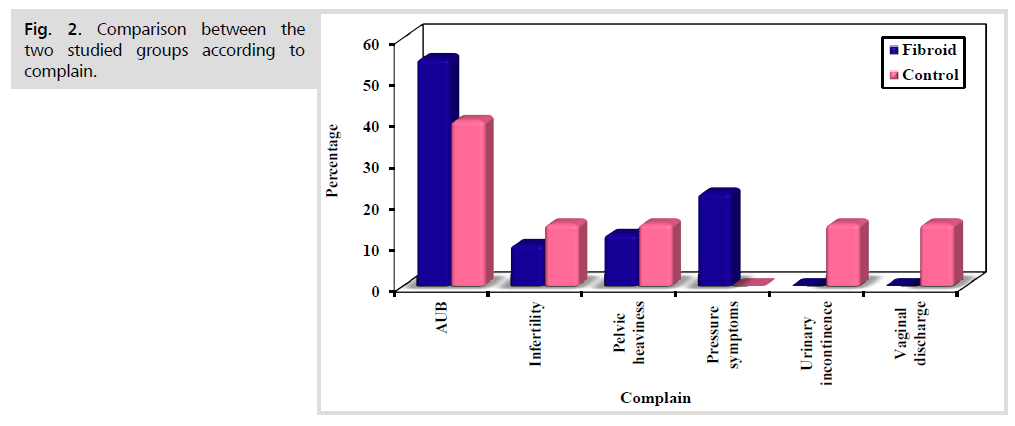
Fig 2. Comparison between the two studied groups according to complain.
Out of 40 fibroid cases, 5 women (12.5%) used Mirena, and no cases in the control group. 6 women (15%) in the fibroid group and 8 women (20%) in controls used Tranexamic Acid. 6 women (15%) in the fibroid group and 8 women (20%) in controls used COCs.
In the fibroid group, 9 women (22.5%) had a positive family history, 6 women (15%) had PID, 4 (10%) had vaginitis and 2 (5%) had Cystorectocele.
In the fibroid group, there were 31 (77.5%) cases with vitamin D deficiency and 9 (22.5%) cases with vitamin D insufficiency. There was no significant relationship between vitamin D level (deficient and insufficient) and age, parity, hemoglobin, BMI, size and number of fibroids, complaints, previous intervention, family history, and associated gynecological diseases (p >0.05) (Tab. 3.)
| Variables | Vitamin D level | Test of sig. | p | |||
|---|---|---|---|---|---|---|
| Deficiency (<20) (n= 31) | Insufficiency (21 – 29) (n= 9) | |||||
| No. | % | No. | % | |||
| Age (years) | ||||||
| Min. – Max. | 23.0 – 45.0 | 29.0 – 44.0 | t= 1.108 | 0.275 | ||
| Mean ± SD. | 37.23 ± 5.94 | 37.67 ± 5.0 | ||||
| Median | 38.0 | 39.0 | ||||
| Parity | ||||||
| P0 | 2 | 6.5 | 1 | 11.1 | c2= 1.971 | MCp= 0.616 |
| P1 | 4 | 12.9 | 2 | 22.2 | ||
| P2 | 9 | 29.0 | 1 | 11.1 | ||
| P≥3 | 16 | 51.6 | 5 | 55.6 | ||
| Min. – Max. | 0.0 – 3.0 | 0.0 – 3.0 | U= 134.50 | 0.874 | ||
| Mean ± SD. | 2.26 ± 0.93 | 2.11 ± 1.17 | ||||
| Median | 3.0 | 3.0 | ||||
| HB | ||||||
| Min. – Max. | 8.50 – 11.40 | 8.50 – 11.0 | t= 1.108 | 0.275 | ||
| Mean ± SD. | 10.49 ± 0.84 | 10.13 ± 0.92 | ||||
| Median | 10.60 | 10.40 | ||||
| BMI(kg/m2) | ||||||
| Min. – Max. | 27.0 – 33.0 | 27.10 – 33.0 | t= 0.843 | 0.405 | ||
| Mean ± SD. | 29.10 ± 1.67 | 29.67 ± 2.07 | ||||
| Median | 29.0 | 29.20 | ||||
| Size (mm) | ||||||
| Min. – Max. | 12.0 – 85.0 | 32.0 – 74.0 | t= 0.069 | 0.946 | ||
| Mean ± SD. | 53.65 ± 16.91 | 53.22 ± 13.53 | ||||
| Median | 51.0 | 53.0 | ||||
| Number of fibroid | ||||||
| Min. – Max. | 1.0 – 5.0 | 1.0 – 5.0 | U= 111.50 | 0.371 | ||
| Mean ± SD. | 2.13 ± 1.41 | 1.67 ± 1.32 | ||||
| Median | 2.0 | 1.0 | ||||
| Complain | ||||||
| AUB | 15 | 48.4 | 7 | 77.8 | 2.724 | MCp= 0.414 |
| Infertility | 4 | 12.9 | 0 | 0.0 | ||
| Pelvic heaviness | 5 | 16.1 | 0 | 0.0 | ||
| Pressure symptoms | 7 | 22.6 | 2 | 22.2 | ||
| Previous intervention | ||||||
| No | 17 | 54.8 | 4 | 44.4 | 7.731 | MCp= 0.097 |
| Cocs | 1 | 3.2 | 1 | 11.1 | ||
| Mirena | 2 | 6.5 | 0 | 0.0 | ||
| Previous myomectomy | 5 | 16.1 | 1 | 11.1 | ||
| Progestogens | 1 | 3.2 | 3 | 33.3 | ||
| Tranexamic Acid | 5 | 16.1 | 0 | 0.0 | ||
| Family history | ||||||
| Positive | 7 | 22.6 | 2 | 22.2 | 0.001 | FEp= 1.000 |
| Irrelevant | 24 | 77.4 | 7 | 77.8 | ||
| Associated gyn. disease | ||||||
| No | 20 | 64.5 | ||||
| Cystorectocele | 1 | 3.2 | ||||
| PID | 6 | 19.4 | ||||
| Vaginitis | 4 | 12.9 | ||||
Tab. 3. Relation between Vitamin D level and different parameters in fibroid group (n = 40).
Discussion
It has been suggested for the past decade that Vit D deficiency is linked to fibroid. According to several studies, the majority of UL patients have hypovitaminosis D [14-16]. Furthermore, some researchers believe that adequate vitamin D serum levels are linked to a lower risk of Uls.(15) Vit D has been shown in studies to be a possible single [17] or combined treatment [18].
Vit D levels were statistically substantially lower in women with UFs compared to controls (14.80 5.87 vs 23.39 9.11, P0.001*) in the current study. The fibroid group had a higher rate of deficit (<20 ng/mL) than the control group (77.5 percent VS 42.5 percent, respectively). In the fibroid group (22 percent), the proportion of women in the insufficiency range (21–29 ng/mL) was lower than in the control group (25 percent). Finally, among controls, the sufficient condition (30-100) was more common. A normal vitamin D level was not found in any of the fibroid cases.
Our findings matched those of Sabry et al., who found that cases with ULs had considerably lower levels of 25-hydroxyvitamin D3 than controls. (19.7 ± 11.8 vs 22.3 ± 6.5 ng/mL, P = .01) [19].
Using data from the National Institute of Environmental Health Sciences Uterine Fibroid study, Baird et al. retrospectively tested stored plasma samples of 1036 women (674 with leiomyomas and 362 unaffected controls) and discovered that those with vitamin D sufficiency (>20 ng/mL) had a 32 percent lower risk of leiomyoma development [15].
Moreover, several studies have linked low levels of serum vitamin D to the development of UF. The majority of the research looked at Afro-American women, who had a higher risk of developing UF.(20, 21) Furthermore, A number of epidemiological studies have also shown the importance of vitamin D deficiency in the development of UFs [15,16].
Brakta et al. examined human and animal data and discovered new avenues for better understanding the Vit D-based therapy approach for the long-term treatment of UFs. Vitamin D3 inhibits leiomyoma cell proliferation and tumor formation in vitro, according to the researchers. These findings suggested that vitamin D3 could be used as a non-surgical, effective, and safe therapeutic option for UFs. They suggested that a clinical trial using vitamin D3 or an analogue for hypocalcemia, paricalcitol, for non-surgical medical therapy of UFs would be needed based on these findings [22].
Mitro et al., on the other hand, found no link between Vit D and uterine leiomyomas. In 3590 premenopausal women, there was no link between blood levels of 25 (OH) D and self-reported UL diagnosis in their large cross-sectional investigation done between 2001 and 2006. The authors noted that the case-finding would lead to differential misclassification, which would result in an "underestimation" of the predicted link between 25 (OH) D3 insufficiencies and the prevalence of uterine leiomyomas [23].
Age, gender, weight, clothes, cultural habits, , Vit D, skin pigmentation calcium supplements, polymorphism of Vit D receptors and sun exposure all have a role in the prevalence of Vit D insufficiency and deficiency among Arabs [24,25].
We found in the fibroid group, there were 31 (77.5%) cases with vitamin D deficiency and 9 (22.5%) cases with vitamin D insufficiency. Age, parity, hemoglobin BMI, size, and number of fibroids, complaints, previous intervention, family, and associated gynecological disorders had no significant link (p >0.05).
Sabry et al's findings, on the other hand, revealed a statistically significant negative connection between serum Vit D levels and UF volume in women with ULs. They found that women with the lowest serum Vit D levels had the most fibroid tumor burden [19].
A number of prior studies have found that Vit D insufficiency is more common among obese people [26,27]. Kumaratne et al. looked at Vit D insufficiency and BMI in a group of Hispanic American teenagers in a retrospective study. In which participants who were overweight or obese were twice as likely to be vitamin D deficient as those who were either underweight or healthy weight. Vitamin D levels were shown to be lower in people with a higher BMI [26].
In contrast to current results, Al-Horani et al. reported that Vit D levels are regulated by a variety of factors, including , gender, sex, nationality, physical activity BMI, and lifestyle,(28) as previously observed in the Middle East [29,30].
In summary, we found that ULs are more prevalent among Egyptian women with deficient D vitamin levels, however, there was no association between the vitamin D levels whether it was deficient or insufficient, and UL size and numbers.
Conclusion
Although uterine leiomyomas are more prevalent among Egyptian women with D vitamin deficiency, no association between the vitamin D levels whether it was deficient or insufficient, and UL size and numbers were reported.
Acknowledgments
The authors of this study possess no acknowledgments to make with regards to this study and this manuscript’s content.
Competing Interests
No competing interests exist.
Authors Contribution
(A) Study Design · (B) Data Collection. (C) Statistical Analysis · (D) Data Interpretation · (E) Manuscript Preparation · (F) Literature Search · (G) No Fund Collection
References
- Mohammadi R, Tabrizi R, Hessami K, et al. Correlation of low serum vitamin-D with uterine leiomyoma: a systematic review and meta-analysis. Reprod Biol Endocrinol. 2020;18(1):85-9.
- Stewart EA, Cookson CL, Gandolfo RA, et al. Epidemiology of uterine fibroids: a systematic review. BJOG: Int J Obstet Gynaecol. 2017;124(10):1501-12.
- Drayer SM, Catherino WH. Prevalence, morbidity, and current medical management of uterine leiomyomas. Int J Gynaecol Obstet. 2015;131(2):117-22.
- Laughlin SK, Schroeder JC, Baird DD. New directions in the epidemiology of uterine fibroids. Semin Reprod Med. 2010;28(3):204-17.
- Pavone D, Clemenza S, Sorbi F, et al. Epidemiology and Risk Factors of Uterine Fibroids. Best Pract Res Clin Obstet Gynaecol. 2018;46:3-11.
- Zepiridis LI, Grimbizis GF, Tarlatzis BC. Infertility and uterine fibroids. Best Pract Res Clin Obstet Gynaecol. 2016;34:66-73.
- Sparic R, Mirkovic L, Malvasi A, et al. Epidemiology of Uterine Myomas: A Review. Int J Fertil Steril. 2016;9(4):424-35.
- Tolvanen J, Uimari O, Ryynänen M, et al. Strong family history of uterine leiomyomatosis warrants fumarate hydratase mutation screening. Hum Reprod. 2012;27(6):1865-9.
- Farzaneh F, Sadeghi K, Chehrazi M. Vitamin D Status in Women with Uterine Fibroids: A Cross-sectional Study. Open Access Maced J Med Sci. 2020;8(B):109-13.
- Rahmanian M, Saghafi M, Darban M, et al. Is Vitamin D Effective in the Treatment of Uterine Leiomyoma? A Randomized Controlled Double-Blind Clinical Trial. Middle East J Rehab Health Stud. 2018;5(4).
- Singh V, Barik A, Imam N. Vitamin D(3) Level in Women with Uterine Fibroid: An Observational Study in Eastern Indian Population. J Obstet Gynaecol India. 2019;69(2):161-5.
- Sersam LW, Najeeb SF. Serum Vitamin D3 Levels in Women with and without Uterine Fibroids. Postgrad Med J. 2018;17(3).
- Srivastava P, Gupta HP, Singhi S, et al. Evaluation of 25-hydroxy vitamin D3 levels in patients with a fibroid uterus. J Obstet Gynaecol. 2020;40(5):710-4.
- Ciebiera M, Włodarczyk M, Ciebiera M, et al. Vitamin D and Uterine Fibroids-Review of the Literature and Novel Concepts. Int J Mol Sci. 2018;19(7).
- Baird DD, Hill MC, Schectman JM, et al. Vitamin D and the risk of uterine fibroids. Epidemiol. 2013;24(3):447-53.
- Paffoni A, Somigliana E, Vigano P, et al. Vitamin D status in women with uterine leiomyomas. J Clin Endocrinol Metab. 2013;98(8):E1374-8.
- Ciavattini A, Delli Carpini G, Serri M, et al. Hypovitaminosis D and "small burden" uterine fibroids: Opportunity for a vitamin D supplementation. Medicine. 2016;95(52):e5698.
- Ali M, Shahin SM, Sabri NA, et al. 1,25 Dihydroxyvitamin D3 Enhances the Antifibroid Effects of Ulipristal Acetate in Human Uterine Fibroids. Reprod Sci. 2019;26(6):812-28.
- Sabry M, Halder SK, Allah AS, et al. Serum vitamin D3 level inversely correlates with uterine fibroid volume in different ethnic groups: a cross-sectional observational study. Int J Womens Health. 2013;5:93-100.
- Baird DD, Patchel SA, Saldana TM, et al. Uterine fibroid incidence and growth in an ultrasound-based, prospective study of young African Americans. Am J Obstet Gynecol. 2020;223(3):402.e1-.e18.
- Wise LA. Study of Environment Lifestyle and Fibroids (SELF): Advancing the Field of Fibroid Epidemiology. J Womens Health. 2015;24(11):862-4.
- Brakta S, Diamond JS, Al-Hendy A, et al. Role of vitamin D in uterine fibroid biology. Fertil Steril. 2015;104(3):698-706.
- Mitro SD, Zota AR. Vitamin D and uterine leiomyoma among a sample of US women: Findings from NHANES, 2001-2006. Reprod Toxicol. 2015;57:81-6.
- Holick MF, Binkley NC, Bischoff-Ferrari HA, et al. Evaluation, treatment, and prevention of vitamin D deficiency: an Endocrine Society clinical practice guideline. J Clin Endocrinol Metab. 2011;96(7):1911-30.
- Al-Musharaf S, Al-Othman A, Al-Daghri NM, et al. Vitamin D deficiency and calcium intake in reference to increased body mass index in children and adolescents. Eur J Pediatr. 2012;171(7):1081-6.
- Kumaratne M, Early G, Cisneros J. Vitamin D Deficiency and Association With Body Mass Index and Lipid Levels in Hispanic American Adolescents. Glob Pediatr Health. 2017;4:2333794x17744141.
- Liu X, Xian Y, Min M, et al. Association of 25-hydroxyvitamin D status with obesity as well as blood glucose and lipid concentrations in children and adolescents in China. Clin Chim Acta. 2016;455:64-7.
- Al-Horani H, Abu Dayyih W, Mallah E, et al. Nationality, Gender, Age, and Body Mass Index Influences on Vitamin D Concentration among Elderly Patients and Young Iraqi and Jordanian in Jordan. Biochem Res Int. 2016;2016:8920503.
- Racinais S, Hamilton B, Li CK, et al. Vitamin D and physical fitness in Qatari girls. Arch Dis Child Educ Pract Ed. 2010;95(10):854-5.
- Al-Daghri NM, Alkharfy KM, Al-Othman A, et al. Effect of gender, season, and vitamin D status on bone biochemical markers in Saudi diabetes patients. Molecules. 2012;17(7):8408-18.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Author Info
Aliaa M. Maaty, Mortada E. Ahmed, Magdy H. Kolaib, Mohamed S. Tolis* and Rania G. El-skaanCopyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.