Case Report - (2024) Volume 19, Issue 4
Conservative management of dehiscent scar discovered in the second trimester: A case report
Salwa Neyazi1, Haytham Hagsaad Abdelrahman Mohamed1, Mohammed Ahmed Mohammed Abdel Razeq1, Mohamed Mahmoud Abdel Aziz2, Raghad Mohamed Albarrak3, Shaden Fahad BinSaeedan3, Reem Hassan Alamri3, Asma Mohammed Almutairi3 and Ahmed Sherif Abdel Hamid Abdel Wahab4*Received: 01-Nov-2024, Manuscript No. gpmp-24-152919; Editor assigned: 04-Nov-2024, Pre QC No. P-152919; Reviewed: 14-Nov-2024, QC No. Q-152919; Revised: 21-Nov-2024, Manuscript No. R-152919; Published: 30-Dec-2024
Abstract
Dehiscent scars and hematomas occurring on previous cesarean scars during pregnancy are uncommon. This situation poses a significant risk to both maternal and fetal health. This case report involves a 32-year-old woman, Gravida 3 Para 2, with two previous cesarean sections, who arrived at the emergency department at 25 weeks and 2 days of gestation, reporting lower abdominal pain. Upon examination, mild tenderness was noted in the right lower quadrant. An ultrasound revealed a hematoma measuring 8.4cm x 3.3cm, indicative of a dehiscent scar, which MRI confirmed. The patient was admitted for careful observation, and routine ultrasounds showed a reduction in the hematoma size, leading to the decision to extend the pregnancy. The initial dose of Dexamethasone was given and subsequently completed. An emergency cesarean section was conducted at 34 weeks and 2 days of gestation, resulting in the successful delivery of a healthy baby girl. The takeaway from this case is that not all cases of dehiscent scars require immediate termination and that conservative management plays a role.
Keywords
Previous scar hematoma; Emergency cesarean section; Dehiscent scar; Incomplete rupture uterus
Introduction
Asymptomatic dehiscences of the lower uterine segment are occasionally discovered during repeat cesarean sections but are rarely identified early in pregnancy. Uterine dehiscence refers to the partial separation of a uterine scar while the serosa layer remains intact. This condition increases the likelihood of uterine rupture; thus, thoroughly assessing the tissue around the outpouching is essential. Uterine rupture involves the complete tearing of all layers of the uterus, including the serosa [1]. It is linked to a significant risk of morbidity and mortality for both mothers and newborns. Surgeries involving the uterus, such as cesarean deliveries, elevate the risk of both dehiscence and rupture. We present a case involving uterine dehiscence associated with a hematoma and highlight the role of sonography in evaluation and treatment planning [2].
Case Presentation
A 32-year-old woman, who is pregnant for the third time and has had two previous deliveries, came to the emergency department of King Khalid Hospital (King Saud University) at 25 weeks and 2 days of gestation, reporting lower abdominal pain that was not radiating, rated at 7 out of 10 in intensity, without any vaginal bleeding or fluid leaking. There were no signs of any medical conditions. The patient has a history of two cesarean sections, with the last one occurring four years ago. She presented with persistent and moderate pain in the right lower abdomen without any bleeding or urinary issues. On examination, there was mild tenderness in the right lower quadrant upon deep palpation but no palpable contractions or tenderness at the surgical scar, and the cervical os was closed.
The Abdominal ultrasound revealed a subacute hematoma situated in front of the uterus, closely associated with the previous cesarean section scar. It was decided to admit her for careful observation, which involved ongoing ultrasounds and an MRI (Fig. 1.). The patient was informed about various management approaches, including the option of pregnancy termination, possible in-utero repair of the defect, or monitoring the situation with preterm delivery. The patient chose not to proceed with termination. The patient rejected the option of repairing the defect due to concerns about the risk of early preterm delivery, as well as being stable and symptom-free. So, conservative management decided to keep the patient in the hospital under observation and serial ultrasound examinations. The patient was given dexamethasone for promoting fetal lung development, and enoxaparin for preventing venous thromboembolism was provided.
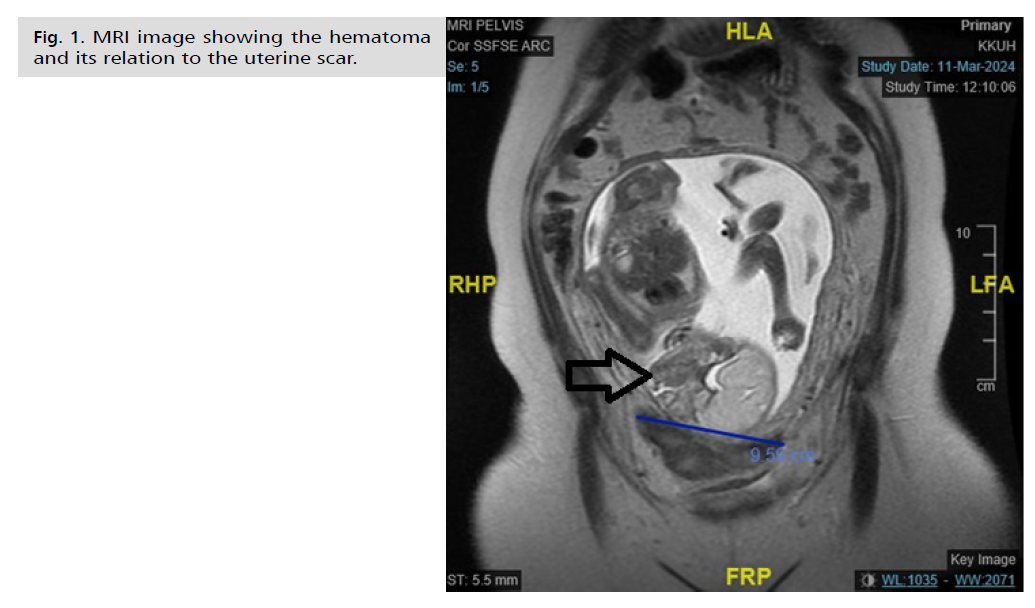
Fig. 1. MRI image showing the hematoma and its relation to the uterine scar.
The initial ultrasound at 25 weeks and 2 days revealed a hypoechoic region measuring 8.4 × 3.3 cm in front of the scar, indicating a dehiscent scar and the presence of a hematoma. Follow-up ultrasounds indicated a gradual decrease in the size of the hematoma at 27 weeks and 4 days: 6.3 × 2.6 cm (Fig. 2.).

Fig. 2. Transabdominal US at 27weeks+2 days showing a decrease in the size of hematoma to 6.3 × 2.6 cm.
The serial ultrasound examinations indicate a positive response with ongoing reduction (shrinkage) of the subacute hematoma located near the cesarean section scar. At 28 weeks and 2 days, the size measured 5.5 × 2.2 cm. At 29 weeks and 2 days, it was 5.5 × 1.6 cm. At 30 weeks and 2 days, the size changed to 5.8 × 1.5 cm. At 31 weeks and 2 days, it measured 2.8 × 1.5 cm. At 32 weeks and 2 days, the dimensions were 3.0 × 1.0 cm. Finally, at 33 weeks and 2 days, it was recorded as 2.3 × 1.2 cm.
Following a consultation with the neonatal intensive care unit (NICU) at 34 weeks and 2 days of gestation, an emergency cesarean section was conducted due to ongoing risks related to the hematoma. While operating, a 3 × 4 cm necrotic and infected hematoma was identified (Fig. 3.) and addressed by repairing the dehiscent scar without any complications. This led to the birth of a healthy baby girl who weighed 2.1 kg and had favorable Apgar scores. The post-operative recovery was straightforward, with minimal blood loss recorded at 700 ml.
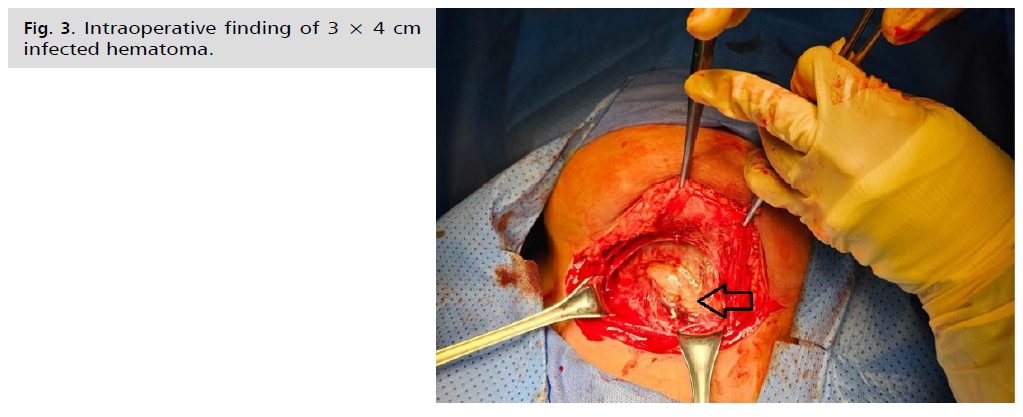
Fig. 3. Intraoperative finding of 3 × 4 cm infected hematoma.
The patient was given postoperative treatment that included antibiotics, specifically cefuroxime 1.5g IV every 8 hours and metronidazole 500mg IV every 8 hours for 48 hours, after which there was a transition to oral antibiotics consisting of cefuroxime 500 mg twice daily and metronidazole 500 mg three times daily at the time of discharge. Prophylactic enoxaparin should be continued for 6 weeks due to an extended hospitalization period, with pain management involving paracetamol 1000 mg and diclofenac 50 mg as needed, alongside wound care instructions. A follow-up strategy was implemented to monitor vital signs, detect possible complications, and ensure the resolution of any hematomas.
Discussion
The strength of the uterus after a cesarean delivery is important for predicting outcomes in future pregnancies, especially for women with multiple cesarean sections. Scars from these surgeries can lead to issues like menstrual problems, ectopic pregnancies, uterine dehiscence, rupture, and complications during labor. The technique used to close the uterine incision can greatly affect uterine strength later. Women who have a "modified two-layer closure" typically experience less bleeding, thicker scars six weeks post-surgery, and lower rates of scar dehiscence [1].
A uterine scar dehiscence occurs when a weakened uterus, often from a previous cesarean section, expands during pregnancy, compromising the integrity of the scar. This separation begins with the internal layers, while the outer serosa layer remains intact. Complications depend on factors such as the fetus's position, defect location, and placenta placement. If the placenta invades the uterine wall, it can lead to placenta percreta, posing risks of severe bleeding, hysterectomy, and even death. If the serosa layer separates, it is classified as a uterine rupture, which is rising in frequency alongside cesarean deliveries. Uterine rupture occurs in about 5 out of 1000 women with a cesarean history [3].
A study revealed that nearly 50% of mothers who experienced a uterine rupture following a trial of labor suffered from moderate postpartum hemorrhage. In comparison, 15% encountered severe postpartum hemorrhage, and 3.8% required a peripartum hysterectomy. Additionally, in the same study, 57.7% of newborns were reported to have perinatal complications, with 9.3% classified as serious. These serious complications included perinatal death, severe asphyxia, and post-hypoxic encephalopathy [4,5].
MRI is the gold standard for diagnosing uterine dehiscence, while sonography effectively monitors changes during pregnancy. Both transabdominal and endovaginal sonography are recommended for evaluating cesarean scar dehiscence in pregnant women. A transabdominal approach can provide a broader view of the defect in the fetus and bladder. In contrast, an endovaginal approach offers more detail on the serosa layer's defect size and integrity. It's important to measure both the neck of the defect and the size of the sac protruding through it [2].
There are various treatment options for uterine dehiscence, which include terminating the pregnancy, followed by fixing the defect or attempting to repair the defect. In contrast, the pregnancy is ongoing, or the situation is expected with preterm delivery. Repairing the defect while the pregnancy is continuing involves a high risk of uterine rupture. This approach should only be pursued if the dehiscence presents symptoms. The prevailing practice is to monitor the pregnancy through weekly endovaginal ultrasounds closely and to plan for an early cesarean delivery. Prompt delivery is crucial because the onset of contractions and rupture of membranes heightens the risk of uterine rupture, necessitating an urgent cesarean section. During delivery, the defect can be repaired; however, a hysterectomy may be required if the uterus is extensively damaged. One study described the successful repair of symptomatic cesarean scar dehiscence in a non-pregnant individual using a da Vinci-assisted laparoscopic technique. This procedure effectively addressed the defect and alleviated the patient's symptoms.
In a case series by Hatstat, et al. [1], a 27-year-old pregnant woman with a history of two cesarean sections experienced right lower abdominal pain at 17 weeks gestation. An MRI revealed a 1.26 mm myometrial defect in the anterior lower uterine segment, with part of the amniotic sac herniating through it. She opted to continue her pregnancy, monitored with weekly ultrasounds and had an early cesarean at 34 weeks, where the defect was repaired. Another case involved a 33-year-old woman with a similar delivery history. Before becoming pregnant, she underwent imaging that indicated fluid outside the uterus and a thin lower uterine segment showing an absent myometrium. During her pregnancy, she was monitored for potential complications and, at 29 weeks, was found to have a 3.5 cm myometrial defect. Given her high risk for placenta percreta, a planned early cesarean was performed at 36 weeks, with successful repair of the defect and no complications for the mother or newborn.
The study by Zhu, et al. [2] in 2021 was a retrospective analysis at the Third Affiliated Hospital of Zhengzhou University, analyzing deliveries from January 2016 to December 2020. It focused on 23 women with uterine scar dehiscence identified during cesarean sections. Most participants (22) were carrying singletons; the average age was 34 years. Fourteen had one prior cesarean, and nine had two. Most (20) underwent elective cesareans. Preoperative detection of dehiscence via ultrasonography was 26.1%, while intraoperative detection was 69.6%. Six cases were detected preoperatively, while 17 were missed. Findings included anechoic regions and thinner lower uterine segments. There were no fatalities among mothers or new-borns, although one woman chose to terminate her pregnancy. Among gestational ages between 37 to 40 weeks, scar thickness varied from 1.0 to 1.8 mm, with one case of dehiscence in a woman with a 1 mm thick scar at 38 weeks.
Conclusion
This case report's message is that early detection of uterine scar dehiscence in women with prior cesarean delivery can reduce maternal and neonatal risks. Regular scans during pregnancy and accurate identification of ultrasound features are crucial. Even if dehiscence is found in the second trimester, conservative management through strict observation is a viable option.
Authors Contributions
All authors jointly contributed to the conception and design of the study.
Funding
This research received no external funding.
Disclosure of Interest
The authors declare no conflict of interest.
Ethics Approval and Informed Consent to Participate
No IRB is required as it is a case report.
Data Sharing
The datasets used and analyzed during the current study are available from the corresponding author upon reasonable request.
Acknowledgment
Not applicable.
Authors' Contribution
(A) Study Design · (B) Data Collection . (C) Statistical Analysis · (D) Data Interpretation · (E) Manuscript Preparation · (F) Literature Search · (G) No Fund Collection
References
- Hatstat LM. Sonographic assessment of uterine dehiscence during pregnancy in women with a history of cesarean section: A case series. J Diagn Med Sonogr. 2016;32(5):283-286.
- Zhu Z, Li H, Zhang J. Uterine dehiscence in pregnant with previous caesarean delivery. Ann Med. 2021;53(1):1266-1270.
- Fogelberg M, Baranov A, Herbst A, et al. Underreporting of complete uterine rupture and uterine dehiscence in women with previous cesarean section. J Matern Fetal Neonatal Med. 2017;30(17):2058-2061.
- Al‐Zirqi I, Stray‐Pedersen B, Forsén L, et al. Uterine rupture after previous caesarean section. BJOG. 2010;117(7):809-820.
- La Rosa MF, McCarthy S, Richter C, et al. Robotic repair of uterine dehiscence. JSLS. 2013;17(1):156.
Author Info
Salwa Neyazi1, Haytham Hagsaad Abdelrahman Mohamed1, Mohammed Ahmed Mohammed Abdel Razeq1, Mohamed Mahmoud Abdel Aziz2, Raghad Mohamed Albarrak3, Shaden Fahad BinSaeedan3, Reem Hassan Alamri3, Asma Mohammed Almutairi3 and Ahmed Sherif Abdel Hamid Abdel Wahab4*2Department of Anesthesia, Faculty of Medicine, King Saud University, Riyadh, Saudi Arabia
3Medical Intern, King Saud University, Riyadh, Saudi Arabia
4Department of Obstetrics and Gynecology, Faculty of Medicine, Ain Shams University, Cairo, Egypt
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.