Research - (2024) Volume 19, Issue 1
Received: 02-Jan-2024, Manuscript No. gpmp-24-124228; Editor assigned: 04-Jan-2024, Pre QC No. P-124228; Reviewed: 16-Jan-2024, QC No. Q-124228; Revised: 22-Jan-2024, Manuscript No. R-124228; Published: 29-Jan-2024
Objective: The primary objective of this study is to assess and compare the effectiveness of postoperative analgesia in mastectomy procedures at Al-Sadder Teaching Hospital in Iraq, specifically examining the outcomes of General Anesthesia (GA) and Pectoral Nerve Blocks (PECs).
Method: The research was conducted at Al-Sadder Teaching Hospital, a specialized hospital within Missan Health hospitals in Iraq that provides care for over 1,200 patients undergoing general surgeries each month. The hospital has a dedicated area for breast cancer patients, offering analgesic treatments and mastectomy surgeries, in addition to chemotherapy and radiation therapy. Approximately six eligible patients were enrolled in the study each month.
Results: The results of the study revealed that there are statistically significant differences between the study groups in favor of PECs block in terms of decreasing post-operative pain, increasing patient’s satisfaction, decreasing post-operative complications, and decreasing the length of ICU stay and hospital stay.
Conclusion: The research conducted at Al-Sadder Teaching Hospital in Iraq has yielded significant findings about pain management techniques for breast cancer surgery by comparing the efficacy of General Anesthesia (GA) and Pectoral Nerve Block (Pecs Block) in postoperative analgesia for mastectomy procedures. In this study, an investigation was conducted to evaluate the efficacy of two distinct methodologies in mitigating postoperative pain, with the ultimate objective of improving overall patient satisfaction and surgical results.
Mastectomy; Postoperative analgesia; General Anesthesia (GA); Pectoral nerve block (Pecs block); Breast cancer
Breast cancer is a highly widespread kind of malignancy that affects mainly women worldwide, representing a significant proportion of cancer cases and necessitating surgical interventions. In 2020 it resulted in 685000 deaths around the world [1]. Mastectomy continues to be a prevalent surgical intervention utilized in the management of breast cancer. Its primary objective is the complete removal of breast tissue with the intention of eradicating or preventing the dissemination of cancerous cells. However, array serving women 60% of them experience sake postoperative pain and 25% to 60% of them experience chronic postoperative pain alter substantially affects the general well-being and recuperation of individuals [2]. Mastectomy, a necessary procedure for the treatment and survival of breast cancer patients, presents the considerable obstacle of postoperative pain management, which has a substantial effect on the general well-being and recuperation of individuals [3].
Thus, the management of postoperative pain is a critical component of surgical care, since it not only promotes patient comfort but also facilitates the postoperative recovery process. In the context of mastectomy, the optimization of postoperative pain management is of utmost significance because to its potential impact on multiple aspects of patient outcomes, including an as early mobilization, decreased duration of hospitalization, and overall patient satisfaction. Generalizing possessed dots, most used analgesic strategies one based on opioids despite them [4]. The utilization of General Anesthesia (GA) has conventionally been employed in mastectomy surgeries, wherein patients frequently want postoperative analgesia based on opioids for pain management [5].
Nevertheless, the utilization of opioids gives rise to apprehensions pertaining to prospective adverse reactions, such as drowsiness, nausea, vomiting, and the risk of developing a dependence on opioids [6]. In order to effectively mitigate these issues and enhance the management of postoperative pain, there has been a growing focus on the utilization of regional anesthetic procedures, including the Pectoral Nerve Blocks (PECs) [7].
The PECs block is a regional anesthetic technique that utilizes ultrasound guidance to specifically target the pectoral nerves [8]. This approach has been found to be highly effective in providing analgesia for mastectomy procedures. This methodology presents the possibility of enhanced postoperative pain management, decreased utilization of opioids, and a reduction in adverse effects associated with opioid usage. As a result, it has become recognized suggested as a valuable substitute or supplementary method to conventional general anesthesia in the context of mastectomy procedures but result are still confiding [9].
The primary objective of this study is to assess and compare the effectiveness of postoperative analgesia in mastectomy procedures at Al-Sadder Teaching Hospital in Iraq, specifically examining the outcomes of General Anesthesia (GA) and Pectoral Nerve Blocks (PECs). Through a comprehensive examination of the results and patient perceptions pertaining to these two methodologies, our objective is to provide significant contributions to the realm of breast surgery and the management of postoperative pain. This research aimed to investigate the effectiveness Pectoral Nerve Blocks in managing postoperative pain and enhancing patient satisfaction in individuals undergoing mastectomy aiming to contribute to the existing knowledge on the advantages of regional anesthetic methods, while also providing valuable recommendations for healthcare professionals and surgeons in improving the quality of care and patient comfort during mastectomy procedures for breast cancer patients in the healthcare system of Iraq.
This study followed a prospective, randomized, and double-blind clinical trial design, conducted at Al-Sadder Teaching Hospital after obtaining ethical approval from the Ministry of Health's ethical committee in Iraq.
The study was conducted over an eighteen-month period, from September 2022 to May 2023. And emitting permits schedule for unilateral conservative breast surgery without axillary clearance.
The research was conducted at Al-Sadder Teaching Hospital, a specialized hospital within Missan Health hospitals that provides care for over 1,200 patients undergoing general surgeries each month. The hospital has a dedicated area for breast cancer patients, offering analgesic treatments and mastectomy surgeries, in addition to chemotherapy and radiation therapy. Approximately six eligible patients were enrolled in the study each month.
Inclusion criteria were adult females aged 18 to 60 years old having an American Society of Anesthesiologists (ASA) physical status I or II.
Exclusion criteria patients who had undergone multiple regional anesthesia procedures, individuals with contraindications to regional blocks, severe cardiopulmonary disease, renal and liver dysfunction, known or suspected neurologic deficits, mental illness, skin infections at the puncture site, coagulation disorders, allergies to local anesthetics, prolonged use of opioids or non-steroidal anti-inflammatory drugs, refusal of pectoral nerve blocks, and those not followed up for more than 48 hours.
Participant recruitment
Participants were recruited from the Al-Shefaa center in Al-Sadder Teaching Hospital. Informed consent was obtained from the patients or their legal guardians, ensuring they understood the study's objectives and the use of regional anesthesia. After obtaining ethical approval from the Ministry of Health ethical committee in Iraq were randomly assigned to one of three groups (Group A - General Anesthesia, Group B - PECS Blocks, Group C - Combination of General Anesthesia and PECS Blocks) using sealed opaque envelopes. The blinding process ensured that both patients and medical staff were unaware of the type of anesthesia administered.
Randomization: Computer-generated random numbers were used to allocate patients into the three groups. The random allocation was concealed within sealed envelopes, which were opened after patient enrollment. Data collection occurred postoperatively, with the researcher collecting and recording samples while remaining unaware of the type of anesthesia each patient received.
Data collection: Data collection was executed using private information forms assigned to each study participant, with a unique serial number associated with the type of anesthesia used during surgery. This approach ensured that collected data remained confidential and could be categorized by the anesthesia type without revealing patient identities.
Statistical analysis
The collected data was revised, coded, and tabulated using Statistical package for Social Science (IBM Corp. Released 2017. IBM SPSS Statistics for Windows, Version 25.0. Armonk, NY: IBM Corp.). Data were presented and suitable analysis was done according to the type of data obtained for each parameter.
Descriptive statistics: Mean, Standard deviation (± SD), Standard error (± SE), Median, and range for distributed numerical data. Frequency and percentage of non-numerical data.
Analytical statistics: Chi-Square test was used to examine the relationship between two qualitative variables.
Fisher Exact or Monte Carlo test: was used to examine the relationship between two qualitative variables when the expected count is less than 5 in more than 20% of cells. Paired T Test was used to assess the statistical significance of the difference between two periods.
One Way ANOVA test was used to assess the statistical significance of the difference between more than two study group parametric variables and used “Tukey” for pairwise comparison.
ANOVA with repeated measures test was used to assess the statistical significance of the difference between more than two periods parametric variables and used “Bonferroni” for pairwise comparison.
The Kruskal Wallis test was used to assess the statistical significance of the difference between more than two study group nonparametric variables and used “Dunn's” for pairwise comparison.
Freidman test was used to assess the statistical significance of the difference between more than two period’s non- parametric variables and used “Dunn's” for pairwise comparison.
Probability of results.
A p-value is considered significant if <0.05 at confidence interval 95%.
A comparative analysis was conducted among three distinct groups, each receiving various treatment modalities: General Anesthesia (GA), pectoralis muscle plane block (PECS block), and a combined approach involving both GA and PECS block. The sample size for each group consisted of 25 female participants. The average age was comparable among the three groups: general anesthesia (GA) group (47.40 ± 8.11 years), pectoralis nerve block (PECS block) group (46.44 ± 9.42 years), and GA with PECS block group (48.28 ± 8.70 years). The obtained p- value exceeded the threshold of 0.05, indicating a lack of statistically significant variation in age across the different groups. The average weight was comparable among the three groups: general anesthesia (GA) group (80.52 ± 7.93 kg), pectoral nerves (PECS) block group (82.04 ± 5.33 kg), and GA with PECS block group (77.92 ± 7.29 kg). The obtained p-value of 0.112 indicates that there is no statistically significant difference in weight between the groups. The average height exhibited minimal variation among the three groups: general anesthesia (GA) group had a mean height of 158.0 ± 4.68 cm, the PECS block group had a mean height of 160.8 ± 3.38 cm, and the GA with PECS block group had a mean height of 159.5 ± 4.24 cm. The obtained p-value indicated that there was no statistically significant variation in height between the different groups (Tab. 1.).
| Variables | GA (n=25) | PECS block (n=25) | GA with PECS block (n=25) | Test | p |
|---|---|---|---|---|---|
| Age (years) | |||||
| Mean ± SD. | 47.40 ± 8.11 | 46.44 ± 9.42 | 48.28 ± 8.70 | F= 0.276 | 0.760 |
| Min. – Max. | 25.0 – 58.0 | 26.0 – 59.0 | 32.0 – 60.0 | ||
| Weight (kg) | |||||
| Mean ± SD. | 80.52 ± 7.93 | 82.04 ± 5.33 | 77.92 ± 7.29 | F= 2.255 | 0.112 |
| Min. – Max. | 67.0 – 100.0 | 70.0 – 91.0 | 68.0 – 90.0 | ||
| Height (cm) | |||||
| Mean ± SD. | 158.0 ± 4.68 | 160.8 ± 3.38 | 159.5 ± 4.24 | F= 2.706 | 0.074 |
| Min. – Max. | 150.0 – 168.0 | 154.0 – 167.0 | 154.0 – 170.0 | ||
Tab. 1. Comparison between the three studied groups regarding to personal data.
According to the data presented in the table, it can be observed that the entirety of the patient population, consisting of 25 individuals in each group, underwent a mastectomy procedure. This implies that there was an absence of variation in the nature of the procedure among the three cohorts. The ASA (American Society of Anesthesiologists) classification was employed for the evaluation of patients' physical condition prior to surgical procedures. The findings indicated that there was no statistically significant variation observed among the three groups under investigation in terms of ASA (Tab. 2. & Fig. 1.).
| Variables | GA (n=25) | PECS block (n=25) | GA with PECS block (n=25) | Test | p | |||
|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |||
| Type of operative | ||||||||
| Mastectomy | 25 | 100.0 | 25 | 100.0 | 25 | 100.0 | – | – |
| ASA classification | ||||||||
| I | 8 | 32.0 | 11 | 44.0 | 6 | 24.0 | Χ2= 2.280 | 0.320 |
| II | 17 | 68.0 | 14 | 56.0 | 19 | 76.0 | ||
Tab. 2. Comparison between the three studied groups regarding to ASA classification.
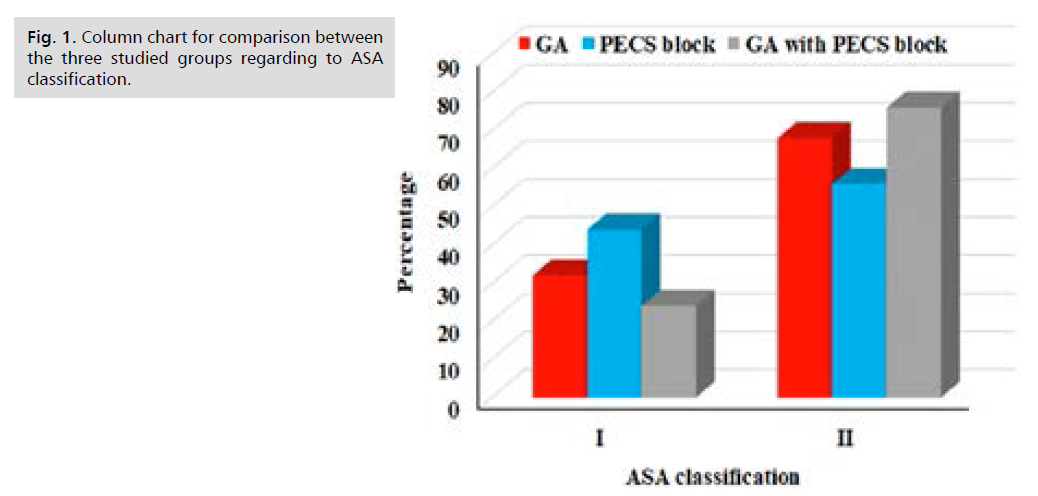
Fig 1. Column chart for comparison between the three studied groups regarding to ASA classification.
According to the data presented in Tab. 3. and Fig. 2. The findings indicate that there was no statistically significant disparity observed in the average Hemoglobin (Hb) levels among the three groups prior to the surgical procedure. Nevertheless, a notable disparity in the average levels of Hb was seen among the three groups following the surgical procedure. The results of the post hoc tests indicated a substantial decrease in the mean Hemoglobin (Hb) level in the General Anesthesia (GA) group compared to the GA with pectoralis muscle plane (PECS) block group. However, there was no statistically significant difference observed between the PECS block group and the other two groups. Nevertheless, the levels of Hemoglobin (Hb) exhibited a decline subsequent to the surgical procedure across all three cohorts. The study's findings revealed a statistically significant disparity in the average hemoglobin levels between the preoperative and postoperative measurements within each group (p<0.05).
| Postoperative Pain Score | ||||||
|---|---|---|---|---|---|---|
| Baseline | 1 hr. | 6 hr. | 12 hr. | 18 hr. | 24 hr. | |
| Mean | 8.20 | 2.24 | 4.88 | 2.76 | 1.48 | 0.76 |
| SE. | 0.26 | 0.14 | 0.22 | 0.23 | 0.13 | 0.09 |
| P1 | <0.001* | 0.076 | <0.001* | <0.001* | <0.001* | |
Tab. 3. Change in postoperative pain score (VAS) in GA group.
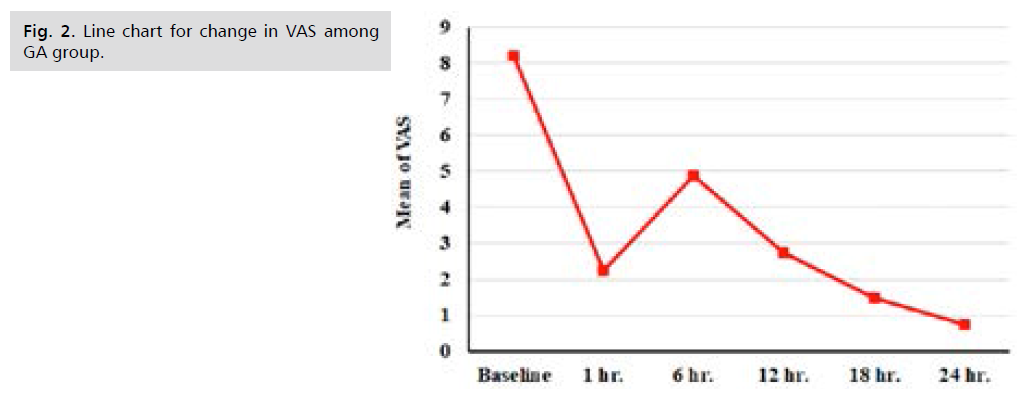
Fig 2. Line chart for change in VAS among GA group.
According to the findings presented in Tab. 4. and Fig. 3. it was observed that the pain score in the group receiving General Anesthesia (GA) exhibited a significant decrease following surgery. Furthermore, this decrease in pain score persisted over time when compared to the baseline period, with statistical significance (p <0.05). Specifically, the mean pain score at baseline was recorded as 8.20, which subsequently decreased to 2.24 at 1 hour, 4.88 at 6 hours, 2.76 at 12 hours, 1.48 at 18 hours, and 0.76 at 24 hours.
| Postoperative Pain Score | GA (n=25) | PECS block (n=25) | GA with PECS block (n=25) | H | P1 | P2 | P3 | P4 |
|---|---|---|---|---|---|---|---|---|
| Baseline | ||||||||
| Mean ± SE. | 8.20 ± 0.26 | 2.16 ± 0.24 | 1.64 ± 0.15 | - | - | - | - | - |
| Min. – Max. | 4.0 – 10.0 | 0.0 – 4.0 | 1.0 – 3.0 | - | - | - | - | - |
| 1 hr. | ||||||||
| Mean ± SE. | 2.24 ± 0.14 | 0.64 ± 0.10 | 1.0 ± 0.0 | 52.266 | <0.001* | <0.001* | <0.001* | 0.185 |
| Min. – Max. | 1.0 – 4.0 | 0.0 – 1.0 | 1.0 – 1.0 | |||||
| 6 hr. | ||||||||
| Mean ± SE. | 4.88 ± 0.22 | 0.60 ± 0.33 | 0.0 ± 0.0 | 53.859 | <0.001* | <0.001* | <0.001* | 0.081 |
| Min. – Max. | 3.0 – 7.0 | 0.0 – 5.0 | 0.0 – 0.0 | |||||
| 12 hr. | ||||||||
| Mean ± SE. | 2.76 ± 0.23 | 0.0 ± 0.0 | 0.0 ± 0.0 | 58.523 | <0.001* | <0.001* | <0.001* | 0.386* |
| Min. – Max. | 1.0 – 5.0 | 0.0 – 0.0 | 0.0 – 0.0 | |||||
| 18 hr. | ||||||||
| Mean ± SE. | 1.48 ± 0.13 | 0.0 ± 0.0 | 0.0 ± 0.0 | 70.696 | <0.001* | <0.001* | <0.001* | 1 |
| Min. – Max. | 0.0 – 3.0 | 0.0 – 0.0 | 0.0 – 0.0 | |||||
| 24 hr. | ||||||||
| Mean ± SE. | 0.76 ± 0.09 | 0.0 ± 0.0 | 0.0 ± 0.0 | 67.027 | <0.001* | <0.001* | <0.001* | 1 |
| Min. – Max. | 0.0 – 1.0 | 0.0 – 0.0 | 0.0 – 0.0 | |||||
Tab. 4. Comparison between the three studied groups regarding to postoperative pain score (VAS).
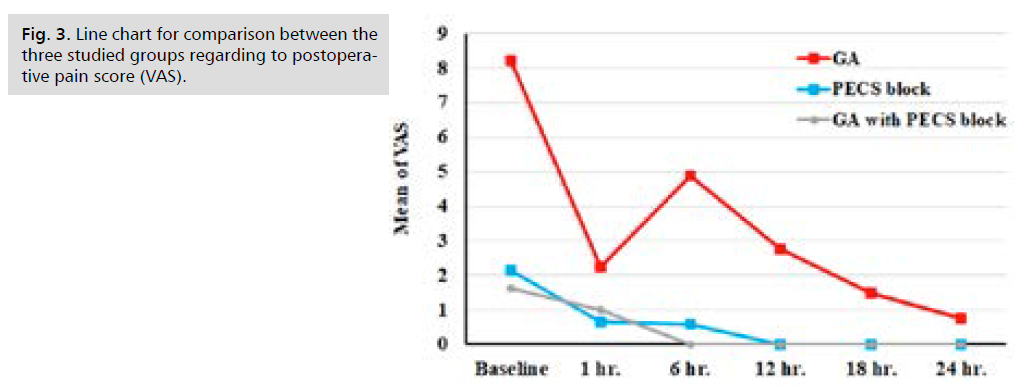
Fig 3. Line chart for comparison between the three studied groups regarding to postoperative pain score (VAS).
With respect to the assessment of postoperative pain scores at various time intervals, the findings indicated a statistically significant elevation in the median pain score within the General Anesthesia (GA) group compared to both the pectoral nerves (PECS) block group and the GA with PECS block group. The findings indicated that female patients who underwent pectoral nerves (PECS) block during the first 12 hours after surgery experienced a complete resolution of pain. In the case of female individuals who underwent General Anesthesia (GA) with pectoralis muscle plane (PECS) block, it was observed that the sensation of discomfort subsided within a duration of 6 hours. This implies that employing either a pectoral nerve block (PECS block) or a combination of General Anesthesia (GA) and PECS block yielded the highest efficacy in mitigating postoperative pain following mastectomy (Tab. 5. & Fig. 4.).
| Type of analgesic requirements postoperative | GA (n=25) | PECS block (n=25) | GA with PECS block (n=25) | Χ2 | P1 | P2 | P3 | P4 | ||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|
| No. | % | No. | % | No. | % | |||||||
| Baseline | ||||||||||||
| Non | 1 | 4 | 21 | 84 | 20 | 80 | 75.62 | MC <0.001* |
MC <0.001* |
MC <0.001* |
FE 1.000 | |
| Tramadol | 24 | 96 | 0 | 0 | 0 | 0 | ||||||
| Paracetamol | 0 | 0 | 4 | 16 | 5 | 20 | ||||||
| 1 hr. | ||||||||||||
| Non | 1 | 4 | 25 | 100 | 25 | 100 | 70.588 | <0.001* | <0.001* | <0.001* | – | |
| Paracetamol | 24 | 96 | 0 | 0 | 0 | 0 | ||||||
| 6 hr. | ||||||||||||
| Non | 8 | 32 | 21 | 84 | 25 | 100 | 46.55 | MC <0.001* |
MC <0.001* |
<0.001* | FE 0.110 | |
| Tramadol | 0 | 0 | 4 | 16 | 0 | 0 | ||||||
| Ketrolac | 17 | 68 | 0 | 0 | 0 | 0 | ||||||
| 12 hr. | ||||||||||||
| Non | 21 | 84 | 25 | 100 | 25 | 100 | 6.088 | MC 0.031* | 0.037* | 0.037* | – | |
| Tramadol | 4 | 16 | 0 | 0 | 0 | 0 | ||||||
| 18 hr. | ||||||||||||
| Non | 1 | 4 | 25 | 100 | 25 | 100 | 70.588 | <0.001* | <0.001* | <0.001* | – | |
| Paracetamol | 24 | 96 | 0 | 0 | 0 | 0 | ||||||
| 24 hr. | ||||||||||||
| Non | 25 | 100 | 25 | 100 | 25 | 100 | – | – | – | – | – | |
Tab. 5. Comparison between the three studied groups regarding to analgesic requirements.
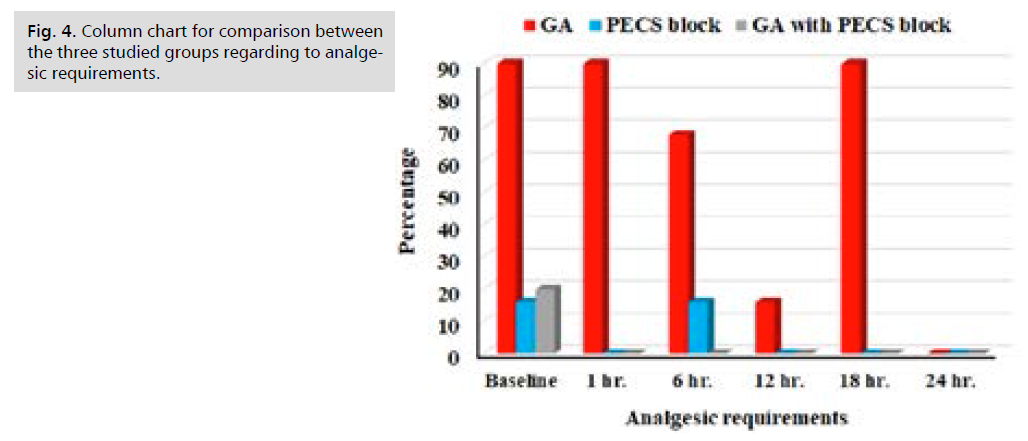
Fig 4. Column chart for comparison between the three studied groups regarding to analgesic requirements.
The surgical intervention known as mastectomy entails the extraction of breast tissue, and the effective management of pain following the procedure is of utmost importance in ensuring patient well-being and recuperation [10]. Regional anesthetic approaches, such as the pectoral nerve block (PECS block), have garnered significant interest as a potential approach to enhance postoperative pain management in individuals undergoing mastectomy, as highlighted by Karvandian, et al. [11]. The PECS block is a form of localized anesthetic that effectively inhibits the neural pathways responsible for innervating the pectoralis major and pectoralis minor muscles. This technique can be employed to administer analgesia during surgical interventions or other operations that involve the aforementioned musculature. The experimental group in this study was administered general anesthesia, a form of anesthesia that induces a state of unconsciousness [12,13]. The administration of general anesthesia normally entails the utilization of a pharmacological amalgamation of sedative agents, analgesic substances, and neuromuscular blocking agents. The PECS block has the potential to mitigate Systolic Blood Pressure (SBP) by the inhibition of stress hormone release and the induction of vasodilation, resulting in the widening of blood vessels. In the study conducted by Naghibi, et al. [14], the group that had general anesthesia was also administered a PECS block.
The research encompassed a comparative analysis of three distinct cohorts that underwent varying treatment approaches: General Anesthesia (GA) in isolation, the Pecs block as a standalone intervention, and the combined strategy using both GA and the Pecs block. Each group was comprised of 25 female participants. The study revealed that the mean age was comparable across the three groups, and no statistically significant disparity was detected. This finding indicates that age did not exert a substantial influence on the comparison of outcomes between the groups. Likewise, the average weight and average height exhibited identical values among the groups, with no statistically significant disparities seen.
According to the study cited in the provided information, it was seen that all 25 patients in each of the three groups underwent mastectomy, implying that there was uniformity in the surgical procedure across the groups. The ASA classification, a widely utilized tool for assessing patients' physical status before surgical procedures, was also utilized by the researchers [11]. The findings indicated that there was no statistically significant difference in ASA classification among the three groups. Previous research has investigated the influence of anesthetic strategies on the categorization and evaluation of risk in surgical procedures for breast cancer [11].
The present study investigated the impact of various anesthetic procedures on the provision of postoperative analgesia in individuals undergoing mastectomy. The findings revealed that a total of 25 patients in each group were administered midazolam as a premedication. Furthermore, there was no statistically significant disparity observed in the allocation of midazolam dosages among the three groups. This implies that the distribution of patients administered with 2 mg, 2.5 mg, and 3 mg of midazolam was comparable among the three groups. Zhou, et al. [13] conducted a study to examine the impact of the combination of Pecs block and general anesthesia on patients undergoing mastectomy. The findings of the study are consistent with our own data, suggesting that there was no statistically significant variation in the administration of midazolam doses among the different groups.
The findings indicate a notable reduction in pain scores within the General Anesthesia (GA) group following the surgical procedure. Moreover, this drop persisted throughout the subsequent time intervals, in contrast to the baseline period (p<0.05). The initial pain score averaged 8.20, then subsequently declined to 2.24 after 1 hour, 4.88 after 6 hours, 2.76 after 12 hours, 1.48 after 18 hours, and 0.76 after 24 hours. The aforementioned findings are consistent with prior research endeavors that have examined the influence of various anesthetic methods on the experience of pain following surgery. In their study, Naghibi, et al. [14] examined the postoperative pain scores and morphine requirements of patients following elective lower abdomen surgery, comparing the effects of spinal anesthesia with general anesthesia. The researchers noted that the utilization of spinal anesthesia was correlated with decreased pain scores and diminished morphine needs in comparison to the use of general anesthesia. In a similar vein, the study conducted by De Cassai, et al. [15] investigated the impact of a pectoral nerve block on the experience of postoperative pain subsequent to breast surgery. The findings of their investigation demonstrated that the group receiving a pectoral nerve block had significantly reduced levels of pain in comparison to the group receiving general anesthesia. Moreover, there was a substantial and statistically significant disparity in the number of analgesic requests made by the two groups.
Gerbershagen, et al. [16] conducted a comprehensive prospective cohort research to assess postoperative pain in a substantial sample of over 50,000 patients belonging to 179 distinct surgery groups. The research underscored significant disparities in pain intensity among various surgical procedures. Although the precise numerical ranking of pain levels may not have held therapeutic importance, its purpose was to enable comparisons among different surgery groups. The study conducted by Chu, et al. [12] aimed to examine the effects of a paravertebral block on the level of postoperative pain experienced by patients who underwent breast surgery. The findings of their research indicate that individuals who had a paravertebral block exhibited notably lower pain scores and decreased usage of opioids in comparison to those who solely underwent general anesthesia. Furthermore, the study conducted by Widmeyer, et al. [17] investigated an innovative methodology for enhancing postoperative pain control and mitigating narcotic usage subsequent to hip arthroscopy. The study revealed that individuals who had a combined approach of general anesthesia and peripheral nerve block exhibited notably reduced pain scores in comparison to those who alone got general anesthesia. Zhang, et al. [10] did a comprehensive review and meta-analysis that specifically examined the analgesic effectiveness and safety of the erector spine plane block in the context of breast cancer surgery. The results of this study shown that the erector spinae plane block had a significant correlation with reduced pain levels in comparison to the utilization of general anesthesia in isolation.
There was no statistically significant difference observed between the mean pain score at 1 hour after surgery and the mean pain score at baseline in the group that had general anesthesia with pectoral nerve block. Nevertheless, the sensation of discomfort ceased throughout the alternate time intervals, and this alteration was deemed to possess statistical significance (p<0.05). These findings indicate that the PECS block shown efficacy in the initial postoperative period for pain reduction; however, its analgesic impact was not sustained beyond a duration of one hour. The findings indicate that the PECS block has the potential to be an effective method for immediate postoperative pain management. Sun, et al. [18] did a meta-analysis that shares similarities with the present study, as it encompassed the identical set of 13 Randomized Controlled Trials (RCTs) involving a total of 940 patients. It also led to a reduction in opioid consumption during the surgical procedure itself, as well as a delay in the time at which the first request for analgesic medication was made. These findings provide more evidence to support the effectiveness of Pecs block in managing pain during breast cancer surgery. In their study, Yu, et al. [19] examined the impact of Pecs II block on the recurrence of breast cancer following surgical intervention. A total of 526 patients diagnosed with breast cancer were randomly assigned to two distinct groups: one receiving general anesthesia alone, and the other receiving general anesthesia in combination with a Pecs II block. The findings of their study demonstrated a considerable reduction in remifentanil use during surgery as a result of the implementation of the Pecs II block. Nevertheless, the Pecs II block did not demonstrate any statistically significant impact on the Overall Survival (OS), Recurrence-Free Survival (RFS), and Distant Recurrence-Free Survival (DRFS) of breast cancer patients following surgical resection. This finding indicates that the administration of Pecs II block did not have a significant effect on the long-term prognosis of individuals with breast cancer. However, it does provide potential benefits in terms of lowering opioid usage during surgical procedures.
The findings of the study indicated that the group receiving general anesthesia with pectoralis nerve blocks (PECS) demonstrated superior results in relation to Postoperative Nausea and Vomiting (PONV), patient satisfaction, and time of discharge. The occurrence of postoperative nausea and vomiting (PONV) was shown to be notably reduced in the group that received General Anesthesia (GA) with pectoral nerves (PECS) block, in comparison to the group that just received general anesthesia. In addition, it was seen that the group receiving general anesthesia with patient-controlled epidural analgesia (GA with PECS) exhibited a greater level of patient satisfaction. This was evidenced by a higher proportion of patients within this group expressing a state of being highly content with their pain management. Furthermore, it was shown that patients who received the GA with PECS block intervention experienced a reduced duration of stay in the Postanesthesia Care Unit (PACU). In order to provide additional substantiation for these findings, an examination of the research conducted by Clairoux, et al. [20] is warranted.
The present study aimed to examine the effects of regional anesthetic, specifically paravertebral blocks, on postoperative outcomes in patients undergoing breast cancer surgery. The findings indicated that individuals who got paravertebral blocks exhibited a reduced duration of hospital stay prior to being deemed ready for discharge, a lower occurrence of Postoperative Nausea and Vomiting (PONV), and shorter stays in the post-anesthesia care unit (PACU) in comparison to those who received General Anesthesia (GA). The results of this study are consistent with previous research indicating that the utilization of regional anesthetic methods, such as the pectoral nerves (PECS) block, may present certain benefits in comparison to general anesthesia alone.
The results of this study indicate that the choice of anesthetic procedure may not significantly influence patient satisfaction. Nevertheless, it is crucial to acknowledge that the aforementioned investigation is a solitary study encompassing a comparatively limited number of participants. Additional investigation is required to validate these findings and gain a more comprehensive understanding of the variables that influence patient contentment with anesthesia.
H. A, N.A and S.J designed the study and performed the experiments. In addition, both authors analyzed the data and write the manuscript.
The authors acknowledge/Sousee University/ Faculty of Medicine Ibn El Jazzar/Tunis/College of Health and Medical Technology, Al-Manara University, Iraq.
These authors declare that above-submitted work was not funded by any governmental or private funding source nor supported by any financial projects.
Not applicable since the study not involving humans or animals.
The authors declare that they have no conflict of interest.
(A) Study Design · (B) Data Collection · (C) Statistical Analysis · (D) Data Interpretation · (E) Manuscript Preparation · (F) Literature Search · (G) No Fund Collection
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.