Research - (2024) Volume 19, Issue 3
Comparison between two different types of remedies for APHTHOUS ULCER in pregnant women
Sinan Forat Hussein1, Aymen Ahmed Jawad Alkhafaji2, Tahreer Shannan Alwan1, Hussein Aziz Naser3, Ali M. Jaafar Abdulsahib4 and Saif M. Hassan1*Received: 26-Jul-2024, Manuscript No. gpmp-24-143246; Editor assigned: 27-Jul-2024, Pre QC No. P-143246; Reviewed: 12-Aug-2024, QC No. Q-143246; Revised: 19-Aug-2024, Manuscript No. R-143246; Published: 30-Sep-2024
Abstract
Recurrent aphthous ulcers (RAU) are common oral mucosal conditions, with a prevalence of approximately 25% worldwide. They manifest as minor or major aphthous ulcers, often recurring due to factors like genetics, nutritional deficiencies, stress, and immune dysfunction. Pregnant Women are more commonly affected, with orthodontics and stress identified as significant risk factors. Although RAU is a very common condition, no definitive treatment has emerged. At the present time, treatment objectives are pain reduction, decrease in number and size of ulcers and reduction in frequency of attacks. This study aims at assessing whether the remedy (consisting of: tetracycline capsule 5 mg, prednisolone tablet 5 mg, Nystatin drops 2cc, and glycerin solution 20cc) is effective in reducing oral aphthous ulcers in patients in comparison to a standard treatment (triamcinolone oral gel).
Keywords
Aphthous; Canker sores; Antimicrobial agents; Anti-inflammatory agents; Systemic treatment; Remedy
Introduction
Oral aphthous (RAU) is a painful inflammatory condition affecting the oral mucosa. Oral aphthous can be manifested independently or secondary to numerous distinct disease processes. If recurrence occurs frequently, it is called recurrent aphthous stomatitis or ulcer [1,2]. Notably, it is most frequently observed in people who wear orthodontics (braces) [3]. Aphthous ulceration is divided into minor and major. The diagnosis is clinical, and management symptomatic. Types of Aphthous ulcer [1,4,5].
Minor aphthous ulcers: (80% of cases) Ulcers start in childhood or adolescence, are <10mm in diameter, and heal in 7–14 days. Crops of ulcers recur every 1–4 months. Ulcers become less frequent with age.
Major aphthous ulcers: (10% of cases) Ulcers usually start in childhood or adolescence, may be as much as 3cm in diameter, and heal over months, often with scarring. Ulcers recur at shorter intervals than minor aphthae. Major aphthae may be a sign of Behçet disease [1,4,5].
Despite the fact that so many hypotheses have been postulated and the fact that the clinical characteristics of RAU are well-defined, the true precise etiologic remains unclear, or idiopathic. While it may occur in association with systemic disease but the majority of patients are otherwise healthy. Aphthous ulcers may be precipitated by stress, trauma, menstruation, or smoking cessation. Genetic factors may also be important [6,7].
The diagnosis of oral aphthous is crucial as there is no specific diagnostic test currently available. And in this situation, diagnosis is based on the patient’s history and clinical findings. There is a need to exclude other possible causes of recurrent oral ulceration, such as Behcet’s disease, PFAPA (Periodic Fever, Aphthous Stomatitis, Pharyngitis, Adenitis) syndrome, and possible HIV infection [7,8]. Also, special attention should be focused on detailed history. Pharmacists should ask about dental procedures before the ulcer emergence, recent local or chemical injuries, systemic illnesses, and the use of drugs like NSAIDS or bisphosphonates. Following the history, the next important step is the examination of the oral cavity [5,7,8].
Aphthous ulcers or “canker sores” present as well-demarcated, oval, or round recurrent oral ulcers with a white or yellow pseudo membrane and a surrounding erythematous halo. Although they may rarely start as red macules or papules but quickly evolve into the classic ulcer. Especially for longer lasting ulcers, a gray membrane may replace the central yellow pseudo membrane. These ulcers are painful and causing disruptions in eating and speaking, often accompanied by a prodromal burning or tingling sensation.7,8,9 RAU involvement affects various oral regions, including the labial mucosa, buccal mucosa, ventral and lateral tongue, floor of the mouth, soft palate, and the oropharynx. RAU is conventionally classified based on size, duration, and presence or absence of scarring after healing into minor and major [5,7,9].
It was assessed the impact of the Oral Aphthous ulcer on the oral health-related quality of life, by considering 7 important aspects: functional limitation, physical pain, psychological discomfort, physical disability, psychological disability, social disability and handicap. They are evaluated through five-level questions (never, almost never, occasionally, frequently and very frequently) to comprehensively understand the impact during both the injury and remission phases [1,10,11].
The selection of treatment for RAU is guided by factors such as diagnosis, clinical presentation, severity, and the presence or absence of extra oral lesions. Treatment objectives include pain management, inflammatory response suppression, recurrence frequency reduction, and minimize ulcer borders. Educating patients about the benign and recurrent nature of RAU, as well as the importance of stress reduction and the elimination of trauma (e.g., cheek bite) is advised. While numerous treatments have been proposed, the approach to treating oral aphthous involves a combination of both topical and systemic agents, offering a multitude of therapeutic options [12,13].
Treatments
- Local anesthetic: Topical anesthetics, such as lidocaine 2% viscous solution or spray, polidocanol adhesive dental paste or benzocaine lozenges, are widely used [12,13].
- Antimicrobial agents: Antimicrobial agents use in RAU is intended to control microbial contamination and secondary infection. Such as (Tetracycline, Chlorhexidine gluconate and Triclosan) [12,13].
- Topical glucocorticoids: Topical corticosteroids, including (triamcinolone, hydrocortisone and dexamethasone), demonstrate efficacy despite their brief contact time. Topical corticosteroid use in patients with RAU is intended to limit the inflammatory process associated with the aphthae formation. Corticosteroids exhibit a direct impact on T lymphocytes, altering the response of effector cells to precipitants of immune pathogenesis (e.g., food allergies, trauma, microorganisms) [12,13].
- Anti-inflammatory agents: They inhibit the formation and release of inflammatory mediators from mast cells and neutrophils, exhibiting anti-allergic properties. While contributing to the healing process of aphthous ulcers, they do not reduce the frequency of RAU episodes, as observed with Amlexanox [12,13].
- Systemic treatment: In severe cases of RAU, the use of systemic therapy may be necessary. Prednisolone tablet: is the drug of choice, either independently or in combination with previously mentioned topical agents. Additional treatment options include (Colchicine, Dapsone, Anti-TNF-a agents, Thalidomide, and Infliximab) [12,13].
- Topical triamcinolone acetonide: The drug that needs to be compared is triamcinolone acetonide against the customized remedy. This corticosteroid medication, classified as a glucocorticoid, exhibits potent anti-inflammatory and immunosuppressive properties. When applied topically as a gel, it reduces inflammation, swelling, redness, and pain associated with mouth ulcers. The mechanism of action involves the suppression of the immune response.
Research Method
A total of 38 patients with oral aphthous were selected and assigned to two groups; Group A, consisting of 19 patients who received triamcinolone oral gel (kenalogue), and Group B, consisting of 19 patients treated with the formulated remedy, that consists of (tetracycline 5 mg capsule, prednisolone 5 mg tablet, nystatin drops 2cc and glycerin 20cc). This study spanned from October 2023 to February 2024.
Exclusion criteria: Adult with any disease other that RAU that could be affected by treatment like (diarrhea), Children below age of 12 (tetracycline cause teeth staining), Pregnant women, Lactation women [14].
Inclusion criteria: Apparently healthy adults with no contraindication for treatment [14].
Method of remedy preparation and dosing: Remedy is composed of a 5 mg capsule of tetracycline, to be opened and mixed, serving as an anti-bacterial agent, alongside with a 5 mg tablet of prednisolone to be grinded and mixed, for immunomodulation. Additionally, it includes 2cc of nystatin drops as an anti-fungal component, and a 20cc glycerine solution to mask the unpleasant taste of tetracycline and facilitate the preparation in a solution form.
Results
The demographic data for patients who have completed the study are shown in Tab. 1. where group A are the patients who received kenalogue (Triamcinolone oral gel) and group B are the patients who received the combination remedy Fig. 1.
| Variables | Group A | Group B |
|---|---|---|
| Number | 19 | 19 |
| Age | 20-50 | 20-40 |
| Gender: Male | 6 | 6 |
| Gender: Female | 13 | 13 |
| Duration of therapy | 10-14 days | 3-10 days |
| Size of aphthous prior to the start of therapy | 0.7-3 cm | 1-3.1 cm |
Tab. 1. Demographic data of the patients.
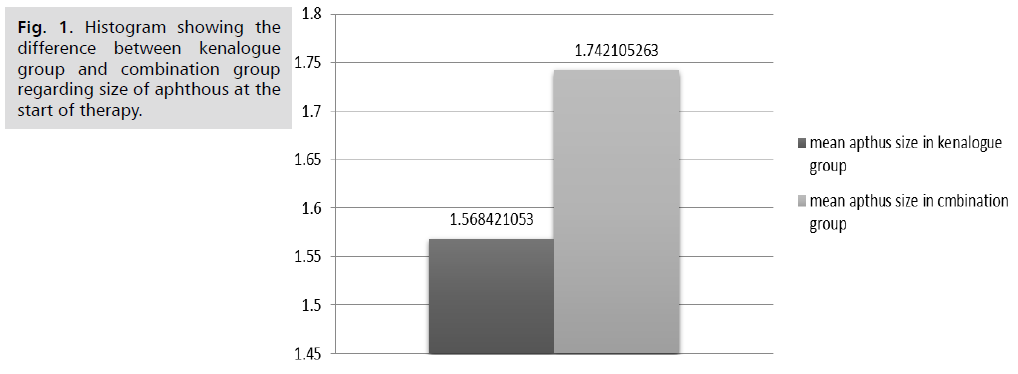
Fig. 1. Histogram showing the difference between kenalogue group and combination group regarding size of aphthous at the start of therapy.
Correlation between age of patient, duration of therapy and size of aphthous in combination group. Tab. 2. shows that there is a significant correlation (P=0.012) between age of patients and size of aphthous. Also shows that there is a significant correlation (P=0.0000001) between size of aphthous and duration of therapy.
| Variables | Age of pt in combination group | Duration of therapy in combination group | Size of aphthous in combination group | |
|---|---|---|---|---|
| Age of pt in combination group | Pearson Correlation | 1 | 0.417 | 0.564* |
| Sig. (2-tailed) | 0.075 | .012 | ||
| N | 19 | 19 | 19 | |
| Duration of therapy in combination group | Pearson Correlation | 0.417 | 1 | 0.848** |
| Sig. (2-tailed) | 0.075 | 0.000 | ||
| N | 19 | 19 | 19 | |
| Size of aphthus in combination group | Pearson Correlation | 0.564* | .848** | 1 |
| Sig. (2-tailed) | 0.012 | 0.000 | - | |
| N | 19 | 19 | 19 | |
**: Correlation is significant at the 0.01 level (2-tailed).
Tab. 2. Correlation between age of patient, duration of therapy and size of aphthous in combination group.
The diagram as in Fig. 2. shows that there is a significant direct correlation (y= 0.3333 * x -3) between age of patient and duration of therapy in combination group. The diagram as in Fig. 3. shows that there is a significant direct correlation (y= 0.1 * x -1) between age of patient and size of aphthous in combination group. The diagram as in Fig. 4. shows that there is a significant direct correlation (y= 0.3 * x -1) between duration of therapy and size of aphthous in combination group. Tab. 3. shows that there is a significant correlation (P=0.004) between age of patients and size of aphthous. Also shows that there is a significant correlation (P=.0000001) between size of aphthous and duration of therapy. The diagram as in Fig. 5. shows that there is a significant direct correlation (y= 0.75 * x -11.25) between age of patient and duration of therapy in kenalogue group. The diagram as in Fig. 6. shows that there is a significant direct correlation (y= 0.075 * x -0.625) between age of patient and size of aphthous in kenalogue group 3.3.2.
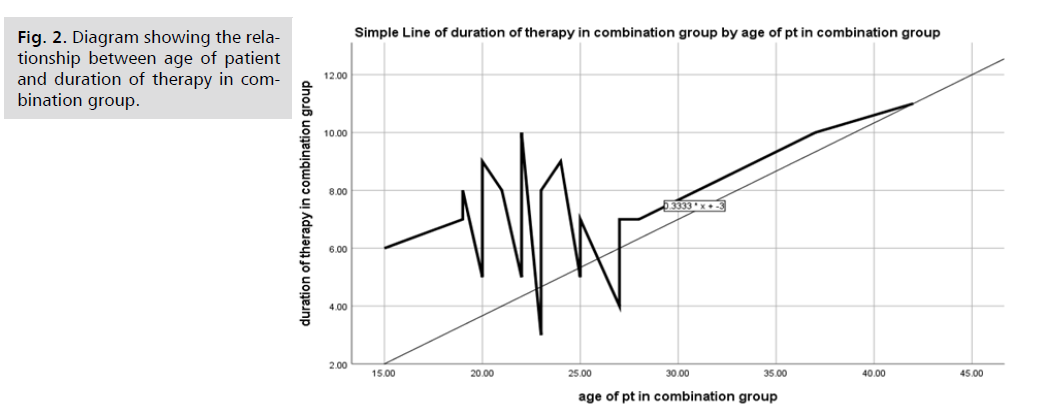
Fig. 2. Diagram showing the relationship between age of patient and duration of therapy in combination group.
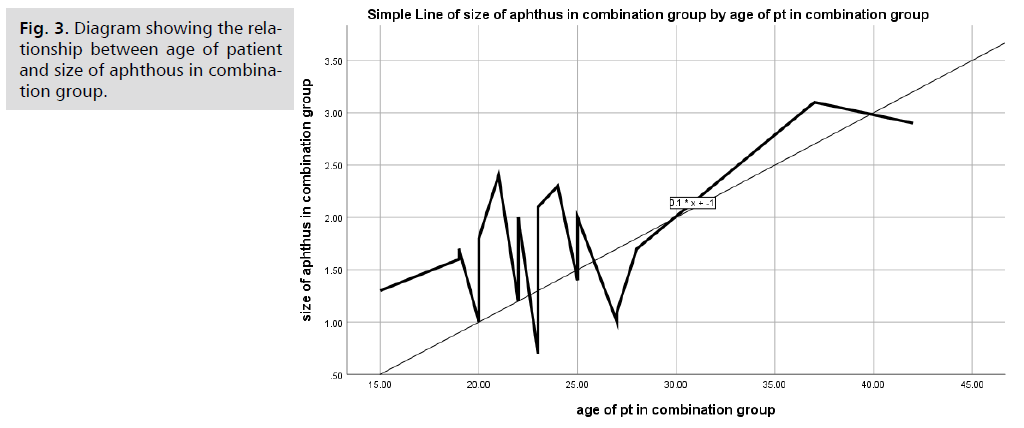
Fig. 3. Diagram showing the relationship between age of patient and size of aphthous in combination group.
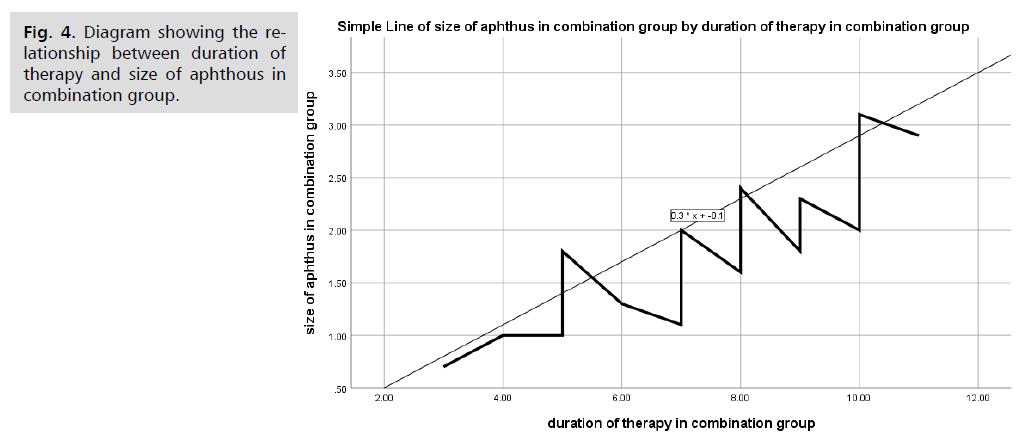
Fig. 4. Diagram showing the relationship between duration of therapy and size of aphthous in combination group.
| Variables | Age of pt in kenalogue group | Size of aphthus in kenalogue group | Duration of therapy in kenalogue group | |
|---|---|---|---|---|
| Age of pt in kenalogue group | Pearson Correlation | 1 | 0.631** | 0.599** |
| Sig. (2-tailed) | 0.004 | 0.007 | ||
| N | 19 | 19 | 19 | |
| Size of aphthus in kenalogue group | Pearson Correlation | 0.631** | 1 | 0.864** |
| Sig. (2-tailed) | .004 | 0.000 | ||
| N | 19 | 19 | 19 | |
| Duration of therapy in kenalogue group | Pearson Correlation | 0.599** | 0.864** | 1 |
| Sig. (2-tailed) | 0.007 | 0.000 | - | |
| N | 19 | 19 | 19 | |
Tab. 3. Correlation between age of patient and duration of therapy and size of aphthous in kenalogue (triamcinolone oral gel) group.
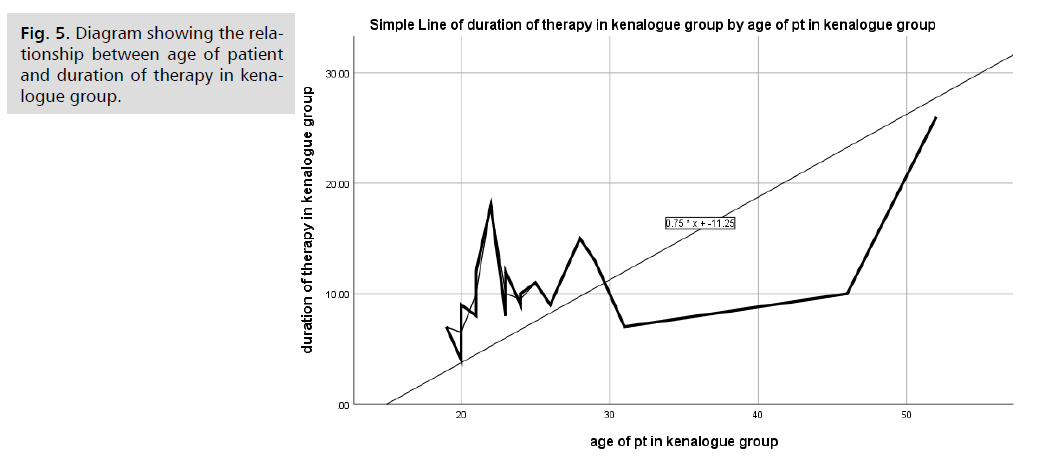
Fig. 5. Diagram showing the relationship between age of patient and duration of therapy in kenalogue group.
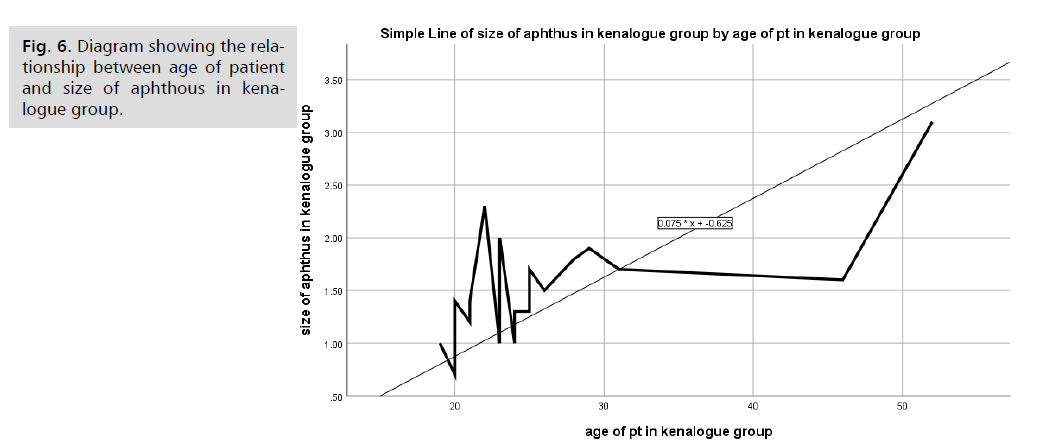
Fig. 6. Diagram showing the relationship between age of patient and size of aphthous in kenalogue group.
Discussion
The description of the demographic features of patients who participated in the study and finished it. The fact that there are two groups, group A and group B, is mentioned in the text. Group A is comprised of patients who were given kenalogue, which is oral gel containing triamcinolone, whereas group B is made up of patients who were given a combined treatment. Based on this information, it appears that the research comprised allocating patients to a variety of therapies in order to establish a comparison of the impact of these treatments on demographic factors.
According to Tab. 2., there are substantial correlations between three variables: the age of patients, the size of the aphthous, and the length of time that therapy is being administered. The correlation between the age of patients and the size of their aphthous spaces has a p-value of 0.012, which indicates that there is a relationship that is statistically significant. In addition, there is a significant correlation between the size of the aphthous and the length of time that therapy is administered. The p-value for this correlation is quite low, which indicates that there is a strong association between these two factors. Taking into consideration these findings, it appears that age, aphthous size, and the length of therapy are all interconnected aspects.
Due to the fact that patients who are older usually have multiple chronic diseases for example (DM, chronic hypertension and hyperthyroidism) and usually infectious diseases go alongside with those chronic diseases. Therefor it is rational and logical to find that aphthous ulcer’s duration of treatment is longer and the possibility of catching the disease is higher in those groups of patient. There is a significant direct correlation was observed between age of patient and duration of therapy and age of patient and size of aphthous in kenalogue (triamcinolone oral gel) group. And this result was inconsistent with the result obtained by Sharquie KE et al. Lactic acid 5 percent mouthwash is an effective mode of therapy in treatment of recurrent aphthous ulcerations.
Conclusion
There are strong relationships between patient age, aphthous size, and therapy duration. The association between age and aphthous size is statistically significant (p=.012), and there is a strong correlation between aphthous size and therapy duration (p=.0000001). These findings suggest that age, aphthous size, and therapy duration are linked factors.
Acknowledgement
The authors would like to thank all the supervisors and all the research participants who willingly attended on the data collection, enabling the successful implementation of this study.
Conflict of Interest
The authors declared there is no conflict of interest
Authors' Contribution
(A) Study Design · (B) Data Collection . (C) Statistical Analysis · (D) Data Interpretation · (E) Manuscript Preparation · (F) Literature Search · (G) No Fund Collection
References
- Preeti L, Magesh KT, Rajkumar K, et al. Recurrent aphthous stomatitis. J Oral Maxillofac Pathol. 2011;15(3):252-256.
- Ship II. Epidemiologic aspects of recurrent aphthous ulcerations. Oral Surg Oral Med Oral Pathol. 1972;33(3):400-6.
- Shulman JD. An exploration of point, annual, and lifetime prevalence in characterizing recurrent aphthous stomatitis in USA children and youths. J Oral Pathol Med. 2004;33(9):558-66.
- Jurge S, Kuffer R, Scully C, et al. Number VI recurrent aphthous stomatitis. Oral Diseases. 2006;12(1):1-21.
- Scully C. Aphthous ulceration. N Engl J Med. 2006;355(2):165-72.
- Porter SR, Hegarty A, Kaliakatsou F, et al. Recurrent aphthous stomatitis. Clin Dermatol. 2000;18(5):569-78.
- Femiano F, Lanza A, Buonaiuto C, et al. Guidelines for diagnosis and management of aphthous stomatitis. Pediatr Infect Dis J. 2007;26(8):728-32.
- Scully C, Porter S. Recurrent aphthous stomatitis: current concepts of etiology, pathogenesis and management. J Oral Pathol Med. 1989;18(1):21-7.
- Paleri V, Staines K, Sloan P, et al. Evaluation of oral ulceration in primary care. Brit Med J. 2010;340.
- Cheng S, Kirtschig G, Cooper S, et al. Interventions for erosive lichen planus affecting mucosal sites. Cochrane Database Syst Rev. 2012(2).
- Brocklehurst P, Tickle M, Glenny AM, et al. Systemic interventions for recurrent aphthous stomatitis (mouth ulcers). Cochrane Database Syst Rev. 2012(9).
- Altenburg A, Abdel‐Naser MB, Seeber H, et al. Practical aspects of management of recurrent aphthous stomatitis. J Eur Acad Dermatol Venereol. 2007;21(8):1019-26.
- Altenburg A, Zouboulis CC. Current concepts in the treatment of recurrent aphthous stomatitis. Skin Therapy Lett. 2008;13(7):1-4.
- Fani MM, Ebrahimi H, Pourshahidi S, et al. Comparing the effect of phenytoin syrup and triamcinolone acetonide ointment on aphthous ulcers in patients with Behcet’s syndrome. Iran Red Crescent Med J. 2012;14(2):75.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Author Info
Sinan Forat Hussein1, Aymen Ahmed Jawad Alkhafaji2, Tahreer Shannan Alwan1, Hussein Aziz Naser3, Ali M. Jaafar Abdulsahib4 and Saif M. Hassan1*2College of Dentistry, AL Ameed University, Iraq
3Al-Zahraa University for Women, Karbala, Iraq
4College of Pharmacy, The Islamic University, Najaf, Iraq
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.