Research - (2023) Volume 18, Issue 1
Comparative study between auadratus lumborum block vs. transversus abdominis plane block for postoperative analgesia in patients undergoing cesarean section
Omar Mohammed Taha Elsafty, Karim Youssef Kamal Hakim and Mohamed Mourad AliReceived: 14-Dec-2022, Manuscript No. gpmp-22-83461; Editor assigned: 15-Dec-2022, Pre QC No. P-83461; Reviewed: 20-Jan-2023, QC No. Q-83461; Revised: 20-Mar-2023, Manuscript No. R-83461; Published: 29-Mar-2023
Abstract
Background: Ultrasound (US)-guided quadratus lumborum block (QLB) and transversus abdominis plane block (TAP) are used as a part of multimodal analgesia for postoperative pain after cesarean delivery.
Methods: Prospective randomized control study.
Results: QLB group showed significantly better visual analog score (VAS) scores from 6 h till 24 h Postoperative. Time for the first request for morphine was significantly longer in the QLB group (10.47 ± 4.6 hrs) than in the TAP group (7.40± 1.5 hrs.), (p < 0.001 and its total consumption was lesser (p=0.01) in the QLB group (4.30 ± 3.4 mg) than in TAP group (6.60 ± 3.4 mg). Moreover, only 3 patients (10%) in the QLB group experienced nausea and/or vomiting vs. 10 (33.3%) in TAP group with significant value.
Conclusion: QLB was more effective in providing visceral and somatic pain analgesia after cesarean section in comparison to TAP block with less incidence of postoperative nausea and/or vomiting
Keywords
Quadratus lumborum block; Transversus abdominis plane block; Postoperative pain management
Abbreviations
US: Ultrasound; QLB: Quadratus lumborum block; TAP: Transversus abdominis plane; CS:caesarean section ASA: American Society of anesthesiologists; ECG: Electrocardiography; SBP: Systolic blood pressure; DBP: Diastolic blood pressure; MABP: Mean arterial blood pressure; Spo2: Arterial oxygen saturation; Etco2: End-tidal co2; VAS: Score visual analog score; PACU: Postanesthesia care unit; SPSS: Statistical Package for Social Science
Introduction
Enhanced recovery after surgery is a multimodal perioperative care pathway that promotes preoperative organ function and reduces the stress response generated by surgical trauma to achieve speed recovery [1]. Opioids have several side effects such as sedation, dizziness, nausea, vomiting, constipation, physical dependence, tolerance, pruritis, and respiratory depression [2]. As a result, various approaches are required to control postoperative pain and reduce opioid usage and adverse effects [3]. The sensory nerves of the anterolateral abdominal wall, T6-L1, that travel to innervate the abdomen are blocked during the transversus abdominis plane block (TAP) [4]. After lower abdominal surgery, a TAP block can provide effective analgesia [5].
Quadratus lumborum block (QLB) block is classified anatomically into 3 groups: QLB 1 (Lateral approach) provides analgesia from T7 to L1 [6]. QLB 2 is conducted by injection medication at the site posterior to the quadratus lumborum muscle from the posterior abdominal wall [7]. QLB 3, also referred to as transmuscular quadratus lumborum block, aimed at the anterior border of quadratus lumborum and posterior to psoas major, so that the anesthetic can spread to the thoracic paravertebral space [8]. In comparison to the TAP block, Blanco R, et al. QLB has an advantage in extending the local anesthetic agent beyond the transversus abdominis plane to the thoracic paravertebral area this increased distribution of local anesthetic agents causes significant analgesia and prolongs the effect of the injected local anesthetic solution [9]. This study aims to compare the effect of ultrasound guided bilateral QLB vs. bilateral ultrasound guided TAP block on postoperative analgesia in patients undergoing cesarean delivery under general anesthesia, and compare the incidence of postoperative nausea and vomiting.
Aim of the Work
This study to compare effect between bilateral quadratus lumborum block vs. bilateral transversus abdominis plane block as postoperative analgesia in pateints undergoing caesarean delivery under general anaestheia to avoid side effect of narcotics as mode of analgesia postoperative.
Methods
A clinically, randomized, controlled and interventional study was conducted from January 2021 to December 2021 at Ain Shams University Gynecology and Obstetrics Hospital. It was approved by the research ethics committee at the faculty of medicine, Ain Shams University, Cairo, Egypt (FMASU M D 08/2020) FWA 000017585 and registered with Pan African Clinical Trial Registry identifier: PACTR202111789904479. Written informed consent was obtained from all patients.
Sixty adult female patients aged between 18 and 45 years old,American Society of anesthesiologists (ASA) II, scheduled for caesarean delivery under general anesthesia. Patients were randomized into two equal groups (TAP group and QLB group). Randomization was performed using a computer generated random number table in opaque sealed envelopes with a 1:1 allocation ratio.
Group TAP (n=30): where each patient received general anesthesia plus bilateral TAP block.
Group QLB (n=30): where each patient received general anesthesia plus bilateral QL block.
Inclusion criteria
1. Female, aged 18- 45years.
2. ASA physical status II.
3. Scheduled for caesarean delivery.
Exclusion criteria
1. Included patients who refused to participate in this study.
2. Had a body mass index (BMI) of more than 30 kg/m.
3. ASA physical status more than II, or had major disease, e.g., cardiac, renal, respiratory, neurologic, or hepatic.
4. Patients using anticoagulants or with coagulopathy.
5. Infection at the site of injection.
6. Allergy or contraindications to local anesthetics.
Study tools
Preoperative settings: A history, clinical examination, and investigations tailored to the patient’s condition were performed for each patient.
Monitoring: All patients were continuously monitored with standard ASA monitors: non-invasive automated blood pressure measurement (NIBP), electrocardiogram (ECG), pulse oximetry (Spao2), and capnography.
Anesthesia and surgical procedure: On arrival of the patients to the operating room, electrocardiography (ECG), noninvasive blood pressure, and pulse oximetry were applied. Baseline parameters such as systolic blood pressure (SBP), diastolic blood pressure (DBP), mean blood pressure (MABP), heart rate (HR), and arterial oxygen saturation (SpO2) were recorded. An intravenous (IV) line was inserted, and IV fluid started. For both groups, general anesthesia was induced with IV injection of fentanyl (1 μg/kg) and propofol (2 mg/kg) then; rocuronium dose for rapid sequence induction (1-1.2 mg/kg) was injected for endotracheal intubation then capnography was connected, and mechanical ventilation was used to maintain the end-expiratory CO2 (ETCO2) values between 34 and 36 mmHg. Anesthesia was maintained with isoflurane 1–2% in a 40% oxygen-air mixture. An incremental dose of rocuronium (0.1-0.2 mg/kg) was given every 30 min or when needed.
After endotracheal intubation, stabilization of the patient’s vital data, and before the start of the surgery, the anesthesiologist (who was blinded to the collected data until the end of the study) performed the block techniques and administered the medication. Both blocks were performed under complete aseptic precautions using an ultrasound machine with a high-frequency linear probe covered with a sterile sheath (Sonoscape® SSI 6000, Chinawith12 6 MHz high-frequency linear probe and curved probe were used) and 100 mm needle (BBraun Medical Inc., Bethlehem, PA, USA). Intraoperative fentanyl 50 ug was given if the HR or the blood pressure or both increase > 20% of the baseline. Isoflurane was discontinued on completion of the surgical procedure, and neostigmine 0.04 mg/kg plus atropine 0.02 mg/kg was administered to reverse the effect of rocuronium. After emergence from anesthesia and achieving an appropriate level of consciousness, the patient was discharged from the operating room to the postanesthesia care unit (PACU). Then, we recorded postoperative total dose of morphine used/24 h, VAS for pain at 0, 2, 4, 6, 12, and 24 h postoperatively also blood pressure and heart rate 0, 2, 4, 6, 12 and 24 h were recorded,the number of patients needed rescue analgesia and any side effect also, the incidence of postoperative nausea and vomiting between both groups was compared. When VAS score was 3 or more, heart rate > 110 beats per minute and or mean arterial blood pressure > 20% from the baseline, (2-3) mg morphine was given intravenously. No other analgesic drugs were given except morphine. The total amount of morphine consumed in 24 hours was recorded.
Measured outcomes
Primary outcome: The total dose of morphine used postoperatively in patient rescue analgesia for 24 h.
Secondary outcome: VAS for pain (recorded at 0, 2, 4, 6, 12, and 24 h postoperative), incidence of post-operative adverse effects, and the number of patients needed rescue analgesia and time for 1st rescue analgesia.
Sample size calculation: The sample size was calculated using the STATA® version 10 programs, setting the alpha error 5% and power at 90%.
Result from previous study Blanco R, et al. showed that the mean post-operative morphine consumption at 24 hour was 6 ± 8.3 in QL block group compared to 13.5 ± 10.7 among TAP block group. Based on this, a sample size of 30 cases in QL group and 30 cases in TAP block group will be needed, taking in account 10% drop out rate [9].
Statistical analysis: Data were analyzed using Statistical Package for Social Science (SPSS) version 22.0. Quantitative data were expressed as mean ± standard deviation (SD). Qualitative data were expressed as frequency and percentage. The following tests were used: Independent-samples t test of significance was used when comparing between two means, chi-square (χ2) test of significance was used to compare proportions between two qualitative parameters, Mann-Whitney U test: for two group comparisons in non-parametric data, the confidence interval was set to 95% and the margin of error accepted was set to 5%. So, we set the significance level at a p value < 0.001 was considered significant.
Results
Postoperative vital data in the form of Mean Arterial Pressure (MAP) and Heart Rate (HR) (Fig. 1. to Fig. 8.) were compared in the two groups and there were no statistical differences between the groups at 1st 6 h then TAP block group had more increase in mean arterial pressure and Heart Rate further on. The two groups were not statistically different for demographic data (Tab. 1. and Tab. 2.). MAP and HR were significantly higher in the TAP group than in the QLB group with a p value less than 0.05. At PACU arrival till the first 6 h postoperative, the QLB group exhibited better clinical pain scores than the TAP block group, however without statistically significant difference between the two groups (Tab. 3. and Tab. 4.). Then, QLB group started to show better VAS scores with significant differences till 24 h postoperative (Tab. 5.). As regards the total dose of narcotics used in each group postoperative morphine consumption was more in the TAP group than the QLP group (P < 0.01) (Tab. 6.).
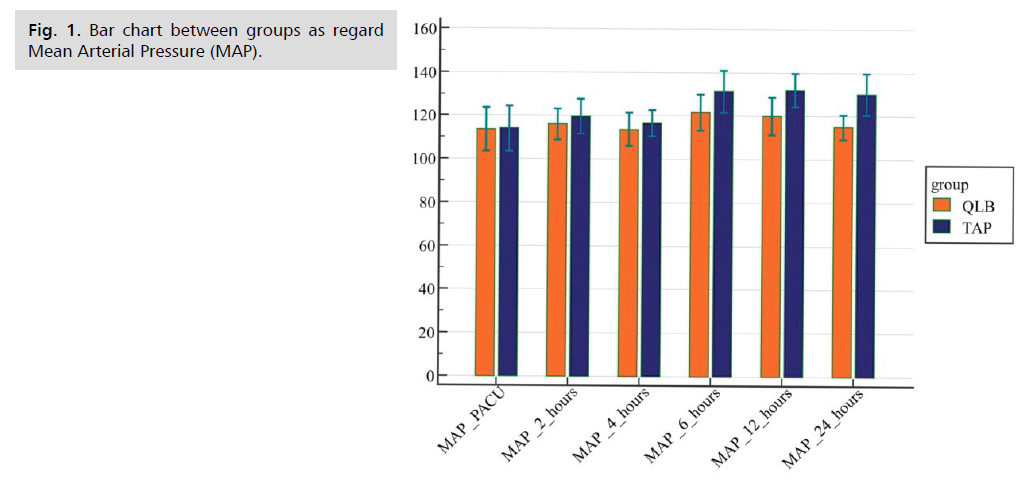
Fig 1. Bar chart between groups as regard Mean Arterial Pressure (MAP).
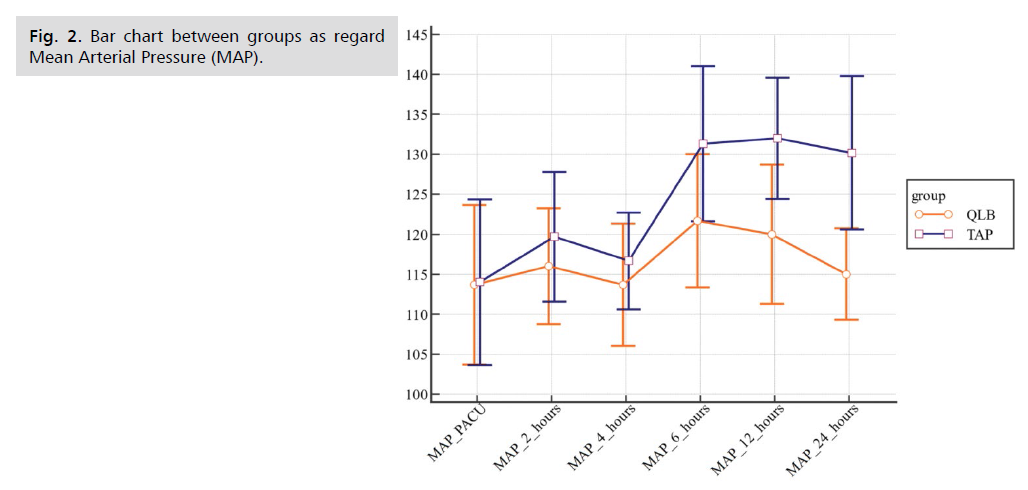
Fig 2. Bar chart between groups as regard Mean Arterial Pressure (MAP).
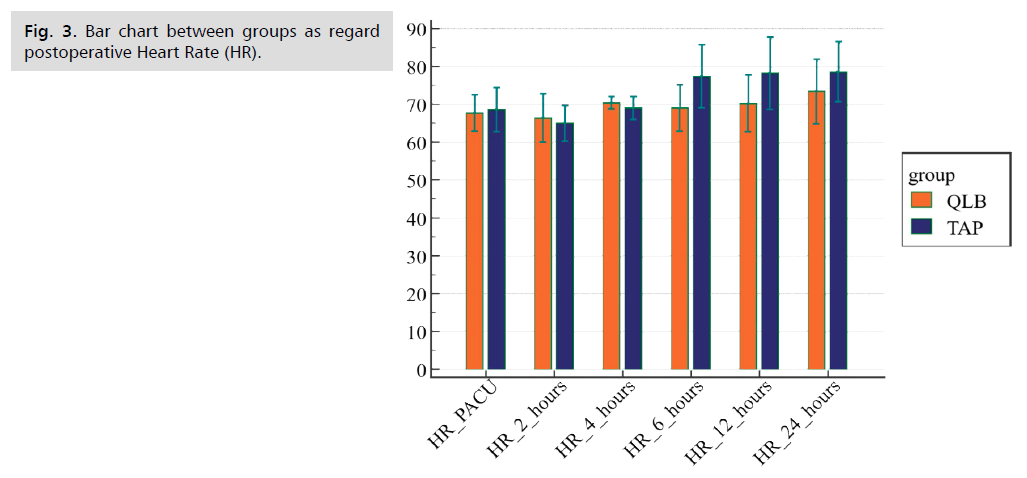
Fig 3. Bar chart between groups as regard postoperative Heart Rate (HR).
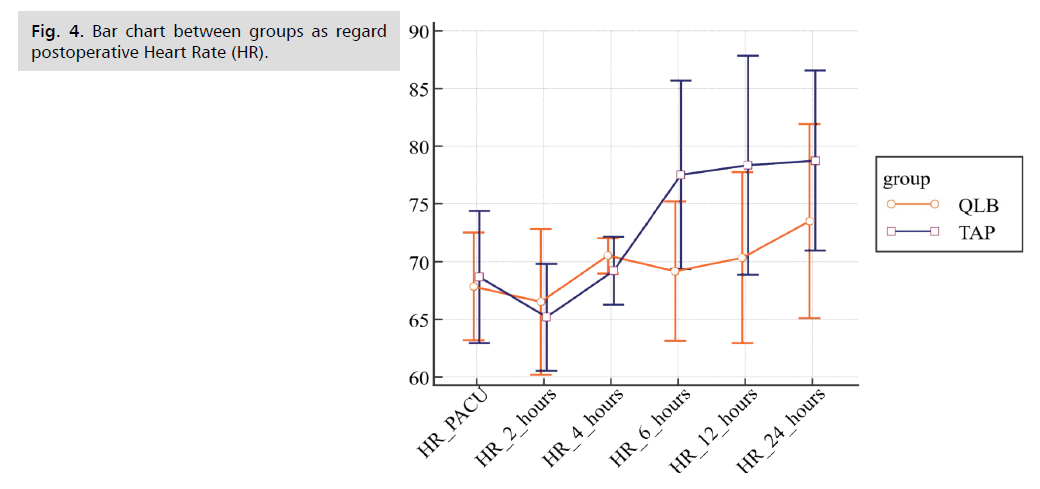
Fig 4. Bar chart between groups as regard postoperative Heart Rate (HR).
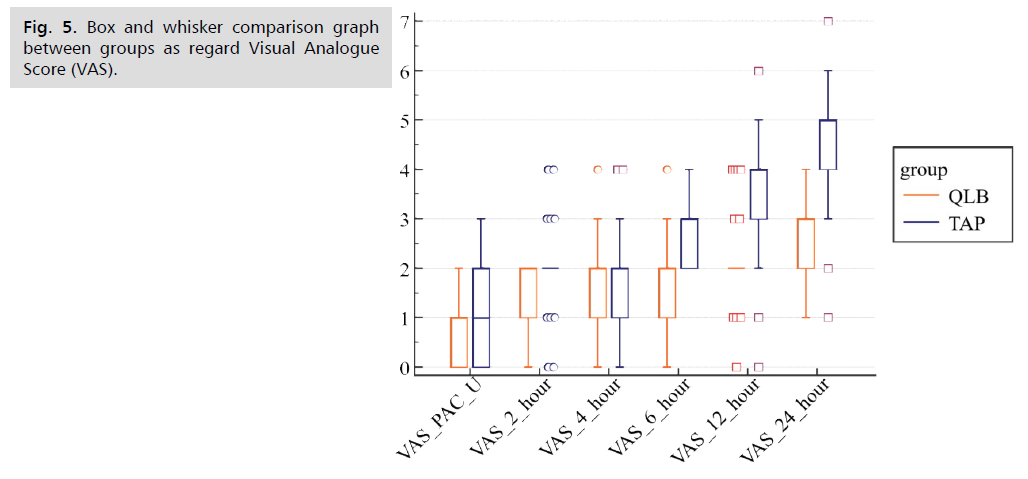
Fig 5. Box and whisker comparison graph between groups as regard Visual Analogue Score (VAS).
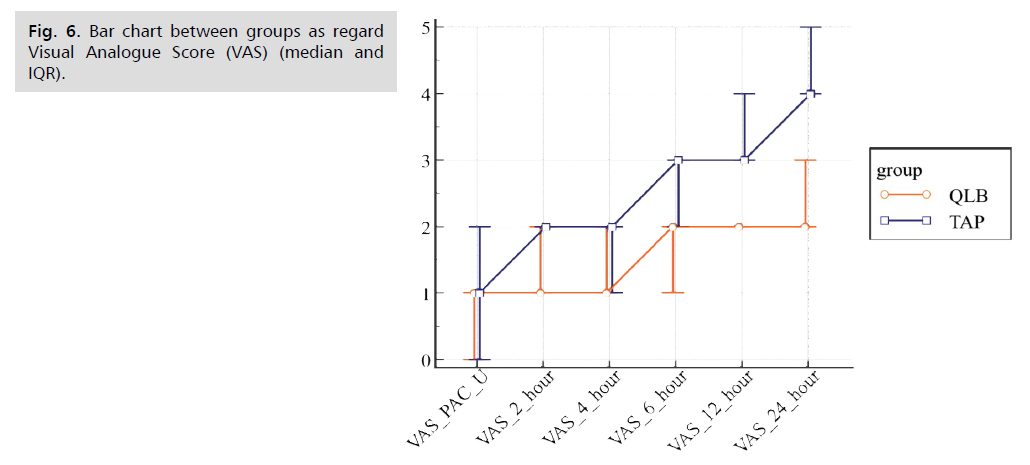
Fig 6. Bar chart between groups as regard Visual Analogue Score (VAS) (median and IQR).
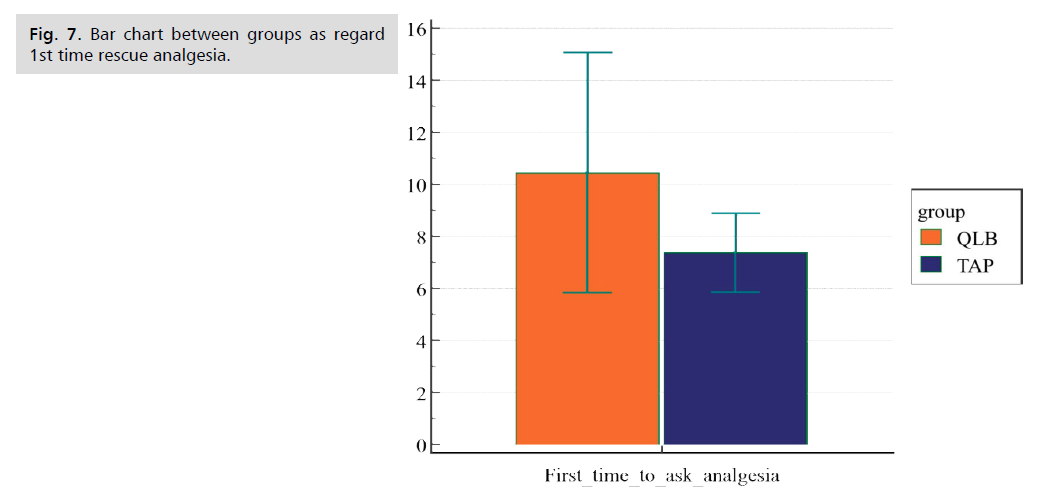
Fig 7. Bar chart between groups as regard 1st time rescue analgesia.
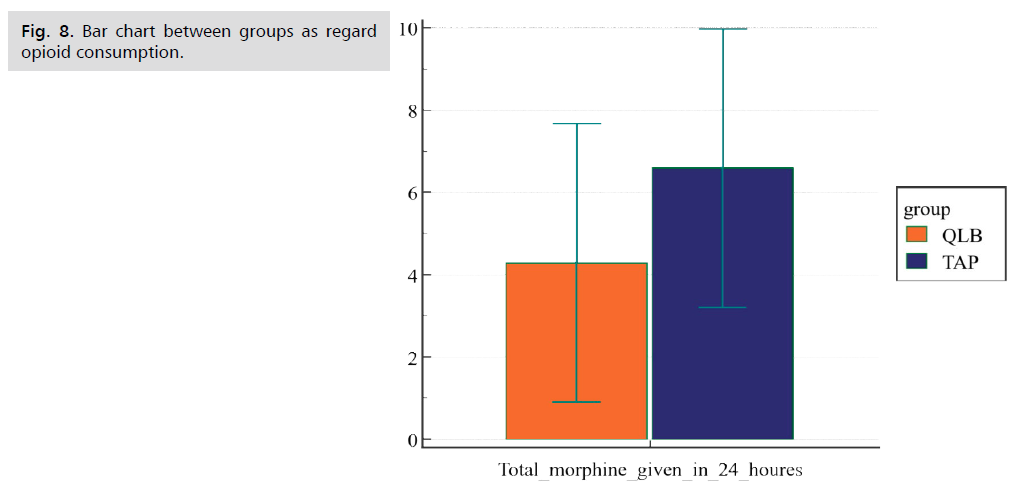
Fig 8. Bar chart between groups as regard opioid consumption.
| Demographic data | TAP group (n=30) | QLB group (n=30) | p-value |
|---|---|---|---|
| Age (years) | 29.6 ± 7.3 | 30.5 ± 7.1 | 0.63 |
| BMI | 29.98 ± 4.7 | 30.73 ± 4.65 | 0.537 |
Tab. 1. Comparison between groups as regard demographic data.
| MAP | TAP group (n=30) | QLB group (n=30) | p-value |
|---|---|---|---|
| PACU | 80.67 ± 5.7 | 80.89 ± 5.39 | 0.87 |
| 2 h | 84 ± 5.06 | 83.44 ± 5.57 | 0.68 |
| 4 h | 82.44 ± 4 | 81.22 ± 4.15 | 0.25 |
| 6 h | 98 ± 6.05 | 88.67 ± 7.41 | <0.001 |
| 12 h | 92.44 ± 8.78 | 87 ± 8.87 | 0.02 |
| 24 h | 94.83 ± 7.05 | 81 ± 3.83 | <0.001 |
Tab. 2. Comparison between groups as regard post-operative MAP.
| HR | TAP group (n=30) | QLB group (n=30) | T | p-value |
|---|---|---|---|---|
| PACU | 68.67 ± 5.7 | 67.83 ± 4.7 | 0.6 | 0.54 |
| 2 h | 65.17 ± 4.6 | 66.50 ± 6.3 | -0.9 | 0.36 |
| 4 h | 69.70 ± 2.6 | 70.17 ± 1.34 | -2.2 | 0.38 |
| 6 h | 77.50 ± 8.2 | 69.17 ± 6.0 | 4.5 | <0.001 |
| 12 h | 78.33 ± 9.5 | 70.33 ± 7.4 | 3.6 | <0.001 |
| 24 h | 78.77 ± 7.8 | 73.50 ± 8.4 | 2.5 | 0.01 |
Tab. 3. Comparison between groups as regard post-operative HR.
| VAS | TAP group (n=30) | QLB group (n=30) | Z | P-value | ||||
|---|---|---|---|---|---|---|---|---|
| Range | Median | IQR | Range | Median | IQR | |||
| PAC|U | 0-3 | 1 | 0 - 2 | 0-2 | 1 | 0 - 1 | 0.87 | 0.38 |
| 2 hours | 0-2 | 1 | 1 - 2 | 0-2 | 1 | 1 - 2 | 4.2 | 0.43 |
| 4 hours | 0-4 | 2 | 1 - 2 | 0-4 | 1 | 1 - 2 | 1.7 | 0.11 |
| 6 hours | 2-4 | 3 | 2 - 3 | 0-4 | 2 | 1 - 2 | 3.97 | <0.001 |
| 12 hours | 0-6 | 3 | 3 - 4 | 0-4 | 2 | 2 - 2 | 3.78 | <0.001 |
| 24 hours | 1-7 | 4 | 4 - 5 | 1-4 | 2 | 2 - 3 | 5.8 | <0.001 |
Tab. 4. Comparison between groups as regard VAS score.
| TAP group (n=30) | QLB group (n=30) | T | p-value | |
|---|---|---|---|---|
| 1st time for rescue analgesia (hours) | 7.40 ± 1.5 | 10.47 ± 4.6 | 3.5 | <0.001 |
| Total morphine consumption (mg) | 6.60 ± 3.4 | 4.30 ± 3.4 | 2.6 | 0.01 |
Tab. 5. Comparison between groups as regard postoperative time and amount of rescue opioids.
| Nausea and/or vomiting | QLP group (n=30) | TAP group (n=30) | P value | ||
|---|---|---|---|---|---|
| No. | % | No. | % | ||
| Yes | 3 | 10 | 10 | 33.3 | 0.028 |
| No | 27 | 90 | 20 | 66.7 | |
Tab. 6. Postoperative complications.
Nausea and vomiting were also examined between the groups and there was a significant difference as the TAP group had more postoperative nausea and vomiting mostly related to more narcotic consumption and more pain score.
Discussion
Our study was conducted on 60 pregnant females enrolled for elective cesarean section divided into two groups; one group received general anesthesia with bilateral Quadratus lumborum block while the other group received general anesthesia with bilateral Transversus abdominis plane block, we found patients received QLB block shows less pain score, less consumption of opioids, and asked rescue analgesia after longer periods than TAP block group. Following cesarean section, poor pain control is linked to longer hospital stay and recovery times, as well as psychological impacts, and patient satisfaction [10]. Traditionally, Opioids are commonly used to manage postoperative pain following CS [11]. The current study also calculated and compared the standard deviation for each of the two groups analyzed, as well as the postoperative VAS score, initial time to rescue analgesia, and total amount of opioids morphine administered in the first 24 h. When compared to the QLB group, TAP block patients showed higher values. The effects of QLB and TAP blocks in this study resulted in a lower incidence and severity of postoperative pain, as well as a lower incidence of total opioid demand.
There was statistically highly significant difference between the two groups as regard Heart rate ,mean arterial blood pressure higher in TAP block group than QLB group at 6,12,24 hrs postoperatively.
There was a statistically highly significant difference between the two groups (P-value <0.001) as regards time for 1st rescue analgesia. In the QLB group it was (10.47 ± 4.6 hr.) while it was earlier in TAP block group (7.40 ± 1.5 hr.)
Also there was a statistically significant difference (P-value <0.01) as regards the rescue analgesic dose of morphine which was lower in the QLB group (4.30 ± 3.4 mg) than the TAP block group (6.60 ± 3.4 mg). Groups were comparable in postoperative pain score using VAS score at regular intervals, and there was a statistically highly significant difference between the two groups (P-value <0.001) as the study group showed less VAS score at (6 hr.,12 hr. and 24 hr.) while there was no statistically difference at (PACU, 2 and 4 hrs. intervals p-value 0.38 and.08 respectively). The current study's findings were congruent with Verma K, et al. findings on a similar topic in which he compared QL and TAP blocks using Ropivacaine 0.2% on 60 females undergoing elective cesarean section under general anesthesia and separated in to two groups. The findings corroborated our findings in terms of total opioid use and pain control duration in the following 72 hours after QL block. Time for rescue analgesic requirement was higher in the QL group than the TAP group (mean ± SD: 68.77 ± 1.74 h vs. 13.3 ± 1.21 h) (P < 0.001). The QLB group had significantly less analgesic demand (P < 0.001) at 2, 4, 6, 12, 24, 36, 48 and 72 h post-CS. The VAS at rest and movement was significantly reduced in the QLB group at all times [12].
In addition the result of our study is in harmony with the results of Alansary AM, et al. who proved that QLB was more effective in providing analgesia after TAH in comparison to TAP block and even more time covering to rescue opioids, sensory level was higher in the QLB group than in the TAP group with less incidence of postoperative nausea and/or vomiting [13].
Aditianingsih D, et al. investigated the analgesic impact of repeated QLB vs. continuous epidural analgesia after laparoscopic nephrectomy in terms of total opioid dose, hemodynamic changes, and postoperative nausea and vomiting QLB used the same total amount of opioids as epidural analgesia to control pain in 65 patients in the first 24 hours after surgery, with no difference in the incidence of postoperative nausea and vomiting [14].
However, Borys M, et al. found that the TAB or QL block did not manage postoperative persistent pain, such as neuropathic pain. They measure post-operative pain for the first, third, and sixth months after CS surgery, but we didn't address these topics here. Whoever was successful in managing pain in the first 24 hours postoperatively using the QLB approach, as previously mentioned [15].
The findings of this study backed up Blanco R, et al. findings from 2016, which revealed that the QLB provides longer-lasting analgesia than the TAP block. Furthermore, their findings demonstrate that using QLB as the default approach can dramatically minimize opiate consumption and deleterious effects after cesarean delivery [7].
Conclusion
Our results showed that QLB was more effective in providing analgesia after CS in comparison to TAP block and even more time covering to rescue opioids with fewer incidences of postoperative nausea and/or vomiting.
References
- Shida D, Tagawa K, Inada K, et al. Enhanced recovery after surgery (ERAS) protocols for colorectal cancer in Japan. BMC Surg. 2015; 15:90.
- Woodhouse A and Mather LE. The effect of duration of dose delivery with patient-controlled analgesia on the incidence of nausea and vomiting after hysterectomy. Br J Clin Pharmacol. 1998; 45: 57-62.
- Ng A, Swami A, Smith G, et al. The analgesic effects of intraperitoneal and incisional bupivacaine with epinephrine after total abdominal hysterectomy. Anesth Analg. 2002; 95: 158-162.
- Almarakbi WA and Kaki AM. Addition of dexmedetomidine to bupivacaine in transversus abdominis plane block potentiates postoperative pain relief among abdominal hysterectomy patients: A prospective randomized controlled trial. Saudi J Anaesth. 2014; 8: 161-166.
- Wegner R, Akwar D, Reyes S, et al. Evaluating the adjuvant effect of dexamethasone to ropivacaine in transversus abdominus plain block for inguinal hernia repair and spermatocelectomy: a Randomized control trial. Pain Physician. 2017; 20:413-418.
- Abrahams M, Derby R, Horn J-L. Update on ultrasound for truncal blocks: a review of the evidence. Reg Anesth Pain Med. 2016; 2: 275-288.
- Blanco R, Ansari T, Girgis E. Quadratus lumborum block for postoperative pain after cesarean section: a randomized controlled trial. Eur J Anaesthesiol. 2015; 32(11): 812-818.
- Hansen CK, Dam M, Bendtsen TF, et al. Ultrasound-guided quadratus lumborum blocks: Definition of the clinically relevant endpoint of injection and the safest approach. An A Case Rep. 2016; 6(2): 39.
- Blanco R, Ansari T, Riad W, et al. Quadratus lumborum block vs. transversus abdominis plane block for postoperative pain after cesarean delivery: A randomized controlled trial. Reg Anesth Pain Med. 2016; 41(6): 757–762.
- Blanton E, Lamvu G, Patanwala I, et al. Non-opioid pain management in benign minimally invasive hysterectomy: A systematic review. Am J Obstet Gynecol. 2017; 216: 557–567.
- Brummett CM, Waljee JF, Goesling J, et al. New persistent opioid use after minor and major surgical procedures in US adults. JAMA Surg. 2017; 152: 70504.
- Verma K, Malawat A, Jethava D, et al. Comparison of transversus abdominis plane block and quadratus lumborum block for post-caesarean section analgesia: A randomised clinical trial. Indian J Anaesth. 2019; 63(10): 820.
- Alansary AM, Kamaly AM, Abdel Hamid HS, et al. Ultrasound-guided quadratus lumborum block versus transversus abdominis plane block in patients undergoing total abdominal hysterectomy. Ain Shams J Anesthesiol. 2022; 14(1): 1-6.
- Aditianingsih D, Pryambodho, Anasy N, et al. A randomized controlled trial on analgesic effect of repeated Quadratus Lumborum block vs. continuous epidural analgesia following laparoscopic nephrectomy. BMC Anesthesiol. 2019;19(1): 221.
- Borys M, Potręć-Studzińska B, Wiech M, et al. Transversus abdominis plane block and quadratus lumborum block did not reduce the incidence or severity of chronic postsurgical pain following cesarean section: a prospective, observational study. Anaesthesiol Intensive Ther. 2019; 51(4): 257-261.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Author Info
Omar Mohammed Taha Elsafty, Karim Youssef Kamal Hakim and Mohamed Mourad AliCopyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.