Research - (2022) Volume 0, Issue 0
Received: 01-Mar-2022, Manuscript No. gpmp-24-150265; Editor assigned: 03-Mar-2022, Pre QC No. P-150265; Reviewed: 16-Mar-2022, QC No. Q-150265; Revised: 23-Mar-2022, Manuscript No. R-150265; Published: 30-Mar-2022
Background: Preterm Premature Rupture of Membranes (PPROM) is a primary factor in Preterm Labor (PTL). Assessing the angle between the cervix and uterus may be necessary in predicting PTL. The study aims to evaluate the precision of cervical length and the posterior and anterior cervical angles in forecasting the latency in PPROM.
Design: A cohort Prospective study on 140 patients with PPROM was done in 2 private hospitals in KSA from March 2021 to March 2022. The Primary outcome was the latency period, defined as the period from PPROM till the occurrence of labor. In contrast, the Secondary Outcomes were ultrasonographic measurements of Cervical Length (CL), Anterior and posterior cervical angles, and other relevant obstetric outcomes.
Methods: Patients with PPROM underwent a transvaginal ultrasound examination to measure the Cervical Length (CL) and posterior and anterior uterocervical angle.
Results: The latency period was within two days in 39 patients (27.9%) and after two days in 101 (72.1%) cases. The CL was 24.18 ± 3.88mm vs. 26.66 ± 3.42mm (p-value<0.001). After two days, the posterior uterocervical angle was 113.64 ± 5.15 vs. 108.88 ± 4.62 (p-value<0.001). The anterior uterocervical angle was 113.43 ± 5.68, vs. 106.55 ± 4.83 (p-value<0.001). The cervical length cut-off value of 24mm resulted in 80.3% sensitivity and 67.9% specificity. The posterior uterocervical angle cut-off value of 107.0˚ yielded a sensitivity of 94.8% and a specificity of 62.8%. In comparison, an anterior uterocervical angle cut-off value of 105˚ resulted in a sensitivity of 93.9% and a specificity of 74%. An anterior uterocervical angle of ≥ 105˚ demonstrated the highest diagnostic value for predicting a latency period within two days.
Conclusion: Cervical dimensions and cervical angles measurements have predictive value for the latency period in women with PPROM.
Latency period; PPROM; Cervical length
Fetal membrane rupture before 37 weeks of pregnancy is termed as PPROM [1]. It can occur in about 4% of all pregnancies and is responsible for approximately 28% of preterm deliveries. Premature birth can result in respiratory distress syndrome, cerebral palsy due to intraventricular hemorrhage, necrotizing enterocolitis, and perinatal death [2].
The time between PROM and birth is known as the latency period in PPROM. Accurately predicting the duration between PPROM and delivery can assist in making informed decisions about transferring newborns to more advanced neonatal facilities and administering corticosteroids to promote lung development in the fetus. The risk of preterm birth can be assessed by measuring cervical length using Transvaginal Ultrasound (TVS). A short cervix of less than 26 mm in the second trimester shows a significant correlation with preterm labor and has a high negative predictive value. This measurement can predict the likelihood of preterm birth in asymptomatic women and those with threatened preterm labor. However, its predictive accuracy as a single measure is limited [3,4].
The angle between the cervical canal and the posterior uterine wall, known as the Posterior Uterocervical Angle (PCA), has been found to have a specificity of 67.4% in predicting labor within 48 hours of Preterm Prelabor Rupture Of Membranes (PPROM) [5].
The angle between the cervical canal and the anterior uterine wall is referred to as the Anterior uterocervical Angle (ACA) and is identified through ultrasonography. It is defined as the angle between the anterior uterine wall and the cervical canal. Several studies have investigated the potential significance of ACA in predicting preterm birth. A wide uterocervical angle of ≥ 95˚ and ≥ 105˚ identified during the second trimester has been associated with an increased risk of spontaneous preterm birth before 37 and 34 weeks, respectively [6].
This study aims to evaluate the effectiveness of Cervical Length (CL), ACA, and PCA in predicting the latency period in patients with PPROM.
This cohort prospective study was performed on 140 patients with PPROM and was done in United Doctor Hospital, Jeddah and Madinah National Hospital, Madinah al Munawara- Saudia Arabia, from March 2021 to March 2022. The study was approved by the ethics committees of both hospitals. Following a thorough explanation of the study's objectives, all patients provided their informed consent.
Eligibility Criteria
Patients who had PPROM were eligible if they had a rupture of membranes between 28 and 34 weeks, which was diagnosed by visually observing amniotic fluid through the external cervical opening using a speculum examination.
The exclusion criteria comprised fetal heart rate abnormalities, antepartum hemorrhage, chorioamnionitis, a history of cervical cerclage in this pregnancy, and women who were in active labor upon admission.
Primary outcomes: Latency period, which is defined as the period from PPROM till the occurrence of labor.
Secondary outcomes: Ultrasonographic measurements of Cervical Length (CL), Anterior and posterior cervical angles, along with other relevant obstetric outcomes
Sample size justification
Sample size of 140 pregnant women was calculated using STATA 14.2 statistical software based on the following parameter: Posterior uterocervical angle showed sensitivity (93%) and specificity (60.1%) in predicting the latency period within two days, as reported by Abd Elhamid, et al., 2020 [7, 8]. The prevalence of preterm premature rupture of membranes was 5%, precision±20 was 20%, and the confidence interval was 95%, with an expected drop out of 10%.
All patients with PPROM were admitted, diagnosed clinically, and managed expectantly without chorioamnionitis criteria. All Patients received corticosteroids in the form of Dexamethasone 6 mg IM/12 hrs for 48 hrs (total 24 mg) and antibiotics in the form of 1 gm oral Azithromycin as per our hospital protocol.
Two examiners conducted abdominal and vaginal ultrasound examinations using a 3.5-5 MHz transabdominal probe and a 5-9 MHz transvaginal probe. The obstetric ultrasound was utilized to assess fetal age, presentation, biophysical profile, amniotic fluid volume, and placenta location. Following the patient's sensation of a full bladder, the transvaginal ultrasound was performed with the probe placed in the anterior fornix to minimize pressure on the cervix. To measure PCA and ACA, a line was drawn from the external to the internal cervical os, and another line was drawn parallel to the inner side of the posterior wall of the uterus (PCA) and the anterior wall of the uterus (ACA). Cervical length is determined by the measurement between the internal and external cervical os. In cases of chorioamnionitis, termination of pregnancy was recommended when the patient went into labor with fetal distress determined by CTG or upon reaching 34 weeks.
Statistical Analysis
The information collected was analyzed using statistical software for social sciences (SPSS Inc., Chicago, Illinois, USA). Mean standard deviation and ranges were used to present quantitative data, while numbers and percentages were used to present qualitative variables. The following steps were taken: An independent-sample t-test was used to compare two means, and a Chi-square (x2) test was used to compare proportions among qualitative parameters. Receiver operating characteristic (ROC curve) analysis was used to assess the overall predictivity of the parameters and to determine the optimal cut-off value. Accuracy was evaluated using sensitivity, specificity, positive predictive value, negative predictive value, overall accuracy, and the likelihood ratios of positive and negative tests.
One Hundred-Forty pregnant women with PPROM were analyzed in this study. The study examined demographic variables like age, Body Mass Index (BMI), and parity, as well as initial measurements such as Total Leucocyte Count (TLC), Amniotic Fluid Index (AFI), Cervical Length (CL), Posterior Uterocervical Angle (PUCA), and Anterior Uterocervical Angle (AUCA), as shown in Tab. 1., which presents the demographic and initial characteristics of the participants.
| Demographic data | Mean ± SD | Range |
|---|---|---|
| Age (years) | 27.18 ± 4.24 | 18-42 |
| BMI (kg/m2) | 21.77 ± 2.45 | 18-31 |
| Parity | No. | % |
| Primi | 52 | 37.1% |
| Multi | 88 | 62.9% |
| Basal | ||
| TLC (× 103/mL) | 8.74 ± 2.71 | 4-18 |
| AFI (cm) | 4.79 ± 1.63 | 2-8 |
| Cervical length (mm) | 25.97 ± 3.71 | 15-32 |
| Posterior uterocervical angle (°) | 110.21 ± 5.21 | 95.2-121.4 |
| Anterior uterocervical angle (°) | 108.47 ± 5.93 | 96.2-124.4 |
Tab. 1. The demographic and basal characteristics.
Labor findings from the study indicated that 91 cases (65%) had vaginal deliveries, while 49 cases (35%) underwent cesarean sections. Among cases with a latency period of 2 days or less, 34 cases (87.2%) had vaginal deliveries, and 5 cases (12.8%) had cesarean sections. In cases with a latency period of more than two days, 57 cases (56.4%) had vaginal deliveries, and 44 cases (43.6%) had cesarean sections (p-value<0.001).
For patients where the time between onset and delivery is 2 days or less, the average birth weight was 2.23 ± 0.41kg. However, for situations where the time between onset and delivery is more than two days, the average birth weight was 2.95 ± 0.35 kg (p-value<0.001). Vaginal delivery was notably more frequent among situations with labor within two days, and birth weight was notably lower for situations with labor within two days.
Tab. 2. displays a comparison of demographic and basal characteristics with a two-day delay. Among cases with labor within two days, the BMI was significantly higher, and TLC, posterior uterocervical angle, and anterior uterocervical angle were also significantly higher. Additionally, AFI and cervical length were significantly lower in cases with labor within two days.
| Variables | Within (n=39) | After (n=101) | p-value |
|---|---|---|---|
| Demographic data | |||
| Age (years) | 27.24 ± 4.61 | 27.16 ± 4.11 | 0.916 |
| BMI (kg/m2) | 23.92 ± 2.34 | 20.94 ± 1.95 | <0.001** |
| Parity | |||
| Primipara | 11 (28.2%) | 41 (40.6%) | 0.174# |
| Multipara | 28 (71.8%) | 60 (59.4%) | |
| Basal | |||
| Enrollment GA (week) | 33.72 ± 1.43 | 33.44 ± 1.26 | 0.255 |
| TLC (×103/mL) | 9.33 ± 2.87 | 8.50 ± 2.63 | 0.105 |
| AFI (cm) | 4.36 ± 1.75 | 4.95 ± 1.55 | 0.045* |
| Cervical length (mm) | 24.18 ± 3.88 | 26.66 ± 3.42 | <0.001** |
| Posterior uterocervical angle (°) | 113.64 ± 5.15 | 108.88 ± 4.62 | <0.001** |
| Anterior uterocervical angle (°) | 113.43 ± 5.68 | 106.55 ± 4.83 | <0.001** |
Tab. 2. Comparison according to latency period (two days) regarding demographic and basal characteristics.
The data presented in Tab. 3. demonstrates that baseline measurements have a significant impact on the prediction of the latency period within a two-day timeframe. The study found that AFI and CL decreased notably in patients with a latency period of less than two days (p<0.037 and p<0.001, respectively). Furthermore, there was an observed increase in PUCA and AUCA in patients with a latency period of less than two days (p<0.001 for both).
| Factor | AUC | SE | P | 95% CI | Cut off |
|---|---|---|---|---|---|
| TLC | 0.546 | 0.052 | 0.519 | 0.424-0.659 | - |
| AFI | 0.639 | 0.044 | 0.037* | 0.525-0.741 | - |
| Cervical length | 0.785 | 0.042 | <0.001** | 0.667-0.887 | ≤24 mm |
| Posterior uterocervical angle | 0.836 | 0.035 | <0.001** | 0.730-0.923 | ≥107.0˚ |
| Anterior uterocervical angle | 0.924 | 0.026 | <0.001** | 0.832-0.993 | ≥105.0˚ |
Tab. 3. Predicting the latency period within two days using basal measurements has a diagnostic performance.
In the analysis of Receiver Operator Curve (ROC) statistics (Fig. 1.), it was noted that a cervical length threshold of 24mm produced a sensitivity of 80.3% and a specificity of 67.9%. A posterior uterocervical angle threshold of 107.0˚ resulted in a sensitivity of 94.8% and a specificity of 62.8%, while an anterior uterocervical angle threshold of 105˚ yielded a sensitivity of 93.9% and a specificity of 74%. It was determined that having an anterior uterocervical angle of ≥105˚ showed the highest diagnostic value for predicting a latency period within two days (Tab. 4.).
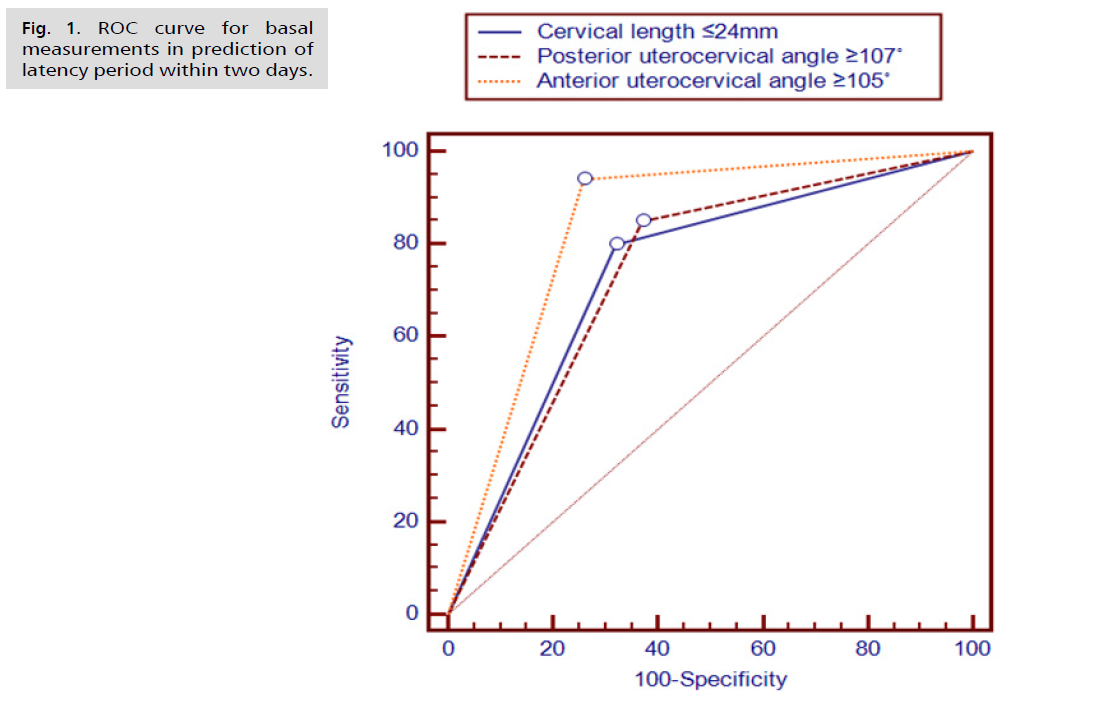
Fig 1. ROC curve for basal measurements in prediction of latency period within two days.
| Characters | Cervical length ≤ 24 mm | Posterior uterocervical angle ≥ 107° | Anterior uterocervical angle ≥ 105° | |||
|---|---|---|---|---|---|---|
| Value | 95% CI | Value | 95% CI | Value | 95% CI | |
| Sensitivity | 80.3% | 68.0%-91.1% | 94.8% | 85.3%-100.0% | 93.9% | 84.2%-100.0% |
| Specificity | 67.9% | 58.9%-75.3% | 62.8% | 53.3%-70.0% | 74.0% | 65.4%-80.0% |
| DA | 71.3% | 64.3%-77.6% | 71.3% | 64.3%-77.6% | 79.8% | 73.2%-85.4% |
| YI | 45.8% | 32.3%-59.2% | 54.6% | 44.0%-65.2% | 66.4% | 56.3%-76.5% |
| PPV | 48.2% | 37.6%-58.9% | 48.6% | 38.9%-58.6% | 57.4% | 46.5%-67.9% |
| NPV | 91.5% | 83.9%-96.8% | 98.4% | 91.9%-100.0% | 99.1% | 93.6%-100.0% |
| LR+ | 2.36 | 1.83-3.07 | 2.40 | 1.95-2.97 | 3.38 | 2.59-4.41 |
| LR− | 0.34 | 0.19-0.56 | 0.12 | 0.04-0.31 | 0.10 | 0.04-0.26 |
| LR | 7.33 | 3.58-15.14 | 20.55 | 7.09-60.03 | 34.38 | 11.76-80.34 |
| Kappa | 0.39 | 0.25-0.51 | 0.42 | 0.31-0.53 | 0.56 | 0.45-0.67 |
Tab. 4. Diagnostic features of basic measurements cutoff thresholds for predicting the time between two days.
There were significantly more perinatal complications in cases where labor occurred within two days. Among cases within 2-day latency period, 6 (5.9%) were complicated by chorioamnionitis, while none of the cases with a latency period after 2 days experienced this complication (p-value<0.001). In cases with a latency period of two days or less, neonatal sepsis occurred in 18 (17.8%) of cases. In contrast, in cases with a latency period exceeding two days, neonatal sepsis occurred in 2 (5.1%) of cases (p-value<0.001). Additionally, in cases with a latency period of 2 days or less, neonatal mortality occurred in 20 (19.8%) of cases, while in cases with a latency period exceeding 2 days, neonatal mortality occurred in 3 (7.7%) of cases (p-value<0.001) (Tab. 5.).
| Variables | Within (n=39) | After (n=101) | p-value |
|---|---|---|---|
| Chorioamnionitis | 6 (5.9%) | 0 (0.0%) | <0.001** |
| Neonatal sepsis | 18 (17.8%) | 2 (5.1%) | <0.001** |
| Neonatal mortality | 20 (19.8%) | 3 (7.7%) | <0.001** |
Tab. 5. Complications.
Among the examined cases, chorioamnionitis was a complication in 6 (4.3%), neonatal sepsis was a complication in 20 (14.3%), and neonatal mortality complication in 23 (16.4%) cases.
We conducted a study to use transvaginal ultrasound to measure cervical length, posterior uterocervical angle, and anterior uterocervical angle. Our goal was to predict the latency period in patients with PPROM. Our findings revealed that in cases with a latency period within two days, certain measurements were significantly different compared to cases with a latency period after two days. For instance, cervical length, posterior uterocervical angle, and anterior uterocervical angle significantly differed between the two groups. BMI, TLC, AFI, and cervical length also showed significant differences.
The results indicate that basal measurements significantly impact the prediction of the latency period within two days. AFI and CL decreased significantly in patients with a latency period of less than two days (p<0.037 and p<0.001, respectively). PCA and ACA increased in patients with a latency period of less than two days (p<0.001 for both).
In a study using Receiver Operator Curve (ROC) statistics, certain cervical and uterocervical angle cut-off values were found to have high sensitivity and specificity for predicting the latency period before labor. Cases with a latency period of 2 days or less experienced more perinatal complications, including chorioamnionitis, neonatal sepsis, and neonatal mortality, compared to cases with a latency period longer than 2 days (p-value<0.001 for all comparisons).
Rizzo and colleagues, who reviewed 92 patients with PPROM, discovered that a Cervical Length (CL) of less than 20 mm was linked to a shorter latency period. On the other hand, Carlan and colleagues, as well as Fischer and Austin, did not find a statistically significant correlation between CL and the latency period when using a 3 cm cut-off to define a short CL [9-11].
Our research demonstrated that PCA and ACA parameters have a high statistical significance in predicting the latency period within two days in PPROM. Kathir, et al.'s study linked PCA to the latency period (p-value = 0.003). A PCA of 113.0˚ was associated with 80.4% sensitivity and 65.5% specificity for labor within two days of PROM [5].
In their research, Perez and colleagues found that an ACA measurement greater than 105 degrees predicted a latency period of 7 days or less with a sensitivity of 78%, and a latency period of 2 days or less with a sensitivity of 90%. These findings may have been influenced by the small number of cases included in Perez's study (98 women). The average AFI among patients with a latency period of two days or less was 4.31 ± 1.09 cm, while it was 4.92 ± 1.38 cm among patients with a latency period longer than two days (p value=0.011) [12].
Mehra, et al. discovered a strong connection between a short Cervical Length (CL) and increased likelihood of labor within a week (if the cutoff value is less than 20 mm, the sensitivity is 44%, and the specificity is 74%) [13].
Ayad, et al. conducted a study where they found that the mean Total Leukocyte Count (TLC) for cases with a latency period of less than two days, a latency period between two and seven days, and a latency period of more than seven days were 13.449 ± 2.959, 10.845 ± 2.432, and 9.389 ± 2.656 (103/μL), respectively. The analysis of variance (ANOVA) test revealed a statistically significant difference in the TLC mean among the different Preterm Premature Rupture Of Membranes (PPROM) groups, with F = 16.755 and a p-value of less than 0.001.
In clinical practice, utilizing transvaginal ultrasound in this investigation for patients with PPROM might help determine whether to transfer expectant mothers to more advanced hospitals with superior neonatal care and administer corticosteroids to improve fetal lung development.
The study is limited by the relatively small sample size and the absence of randomization. The study's advantage is that it was carried out in 2 hospitals, which decreases the publication bias.
More research is necessary, conducted at multiple centers and involving many participants, to examine the impact of cervical angles on predicting the latency period in PPROM.
The Length of the Cervix (CL), the Posterior Uterocervical Angle (PCA), and the Anterior Uterocervical Angle (ACA) measurements have predictive value for the latency period in women with PPROM.
Study approved by Ethical Committee of 2 private hospitals.
Non-applicable.
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
The authors report there are no competing interests to declare.
This study received no financial support.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.