Research Article - (2022) Volume 17, Issue 1
Adnexal Masses In Pregnancy: An overview
Amala Sunder1*, Basma Darwish1, Abdulla Darwish2, Veena Nagaraj2 and Nawal M. Dayoub3Received: 27-Dec-2021, Manuscript No. gpmp-22-50656; Editor assigned: 03-Jan-2022, Pre QC No. P-50656; Reviewed: 10-Jan-2022, QC No. Q-50656; Revised: 12-Jan-2022, Manuscript No. R-50656; Published: 29-Mar-2022
Abstract
Objective: Adnexal masses are discovered in pregnancy during routine examination or with symptoms. The Management options and the pregnancy outcome are based upon the clinical presentation and characteristics of the masses. We analysed the importance of surgical management in our study.
Method: Retrospective observational study of adnexal masses during pregnancy at Bahrain Defence Force Hospital between January 2017 and February 2019. The maternal demographics, clinical presentation of adnexal masses, gestational age at presentation, management and pregnancy outcome were evaluated. All computerised data are anonymized.
Result: During our study period, the incidence of adnexal masses during pregnancy was 0.33%. Out of these 51.7% was managed conservatively and 48.3% was managed surgically. Out of the cases that required surgical intervention, 34% of them were complicated benign masses and 3.4% was malignant. Upon looking the pregnancy outcome two patients in the conservative group had miscarriage and 6.9% ended in preterm delivery. Furthermore 6.9% of babies delivered were diagnosed with intrauterine growth restriction and 17.4% were small for their gestational age. Uneventful pregnancy outcome was 31%.
Conclusion: Adnexal masses have variable presentations during pregnancy. Surgical approaches were required either in complicated or in complex masses to optimize the outcome.
https://marmaris.tours
https://getmarmaristour.com
https://dailytourmarmaris.com
https://marmaristourguide.com
https://marmaris.live
https://marmaris.world
https://marmaris.yachts
Keywords
Adnexal masses, Malignancy, Miscarriages, Ovarian hyper stimulation syndrome, Torsion
Introduction
Adnexal masses in pregnancy include masses in fallopian tubes, ovaries, structures around the uterus. The most frequently diagnosed masses in pregnancy are ovarian cysts. Most of these masses are benign but they can be malignant [1,2]. Incidence rate vary from 0.1 to 10% [3,4]. Studies reported the incidence of malignancy in adnexal masses during pregnancy is of 1 to 8% [3,4]. The effects on pregnancy are miscarriage, preterm labour, preterm premature rupture of membranes, and labour obstruction [3-6]. Pregnancy effects on masses include torsion, rupture, bleeding, infection, and increase in size [3]. Ultrasound and Magnetic Resonance Imaging (MRI) are safe modalities for diagnosing adnexal masses during pregnancy. Tumour markers are often inaccurate and of a restricted use during pregnancy as the markers are produced by decidua and also modified by the physiology of the normal pregnancy [1,7].
Ovarian masses are mostly asymptomatic and regress spontaneously either during the mid-trimester or after delivery. However these masses could be more complicated. Persistence of masses are mostly due to its complexity [8]. Surgical management is usually required in symptomatic complicated cases and masses with complex sonographic structure [9]. In cases with a high suspension of malignancy, intrusive management is needed. Surgical interventions generally involve laparotomy or laparoscopic approaches [10]. Laparoscopic interventions during pregnancy necessitate well-trained professionals. Generally, the management options are individualized [7]. Considering the risks of interventions for pregnant women and foetuses, the management options need to be stratified. Large masses and masses with a high suspicion of malignancy required a well-planned approach. A systematic analysis of individual cases and tailored management approaches help to ensure a safe pregnancy outcome.
Materials and Methods
This is a retrospective analysis of adnexal masses during pregnancy from January 2017 until February 2019 at Bahrain Defence Force Hospital. 8857 pregnant women were seen in our obstetric unit during the study period. We focused the masses identified in the fallopian tubes and ovaries. We excluded ectopic and heterotopic pregnancies, pelvic inflammatory disease, appendicle masses, mesenteric cysts, and hyperstimulated ovaries without torsion .Cases of ovarian hyperstimulation syndrome with torsion were included. Cases were identified on the basis of symptoms, during the routine ultra-sonogram and intrapartum caesarean deliveries. There is always the possibility of missing cases during the routine examination, especially in asymptomatic patients.
Analysis
Data was analysed using Stats Direct statistical package, version: 3.2.10 Merseyside UK 2020. Continuous variables presented in Mean ± SD and median with range. Categorical variables presented as percentage.
Results
In our study, the incidence of adnexal masses during pregnancy was 0.33% (Tab.1. and 2.).
| Total cases | 29 |
| Maternal age | Mean ± SD 27.8 ± 6.4/median (range) 27 (24) |
| Maternal BMI | Mean ± SD 32 ± 6.4/median (range) 33 (21) |
| Previous parity | 20/29 69% |
| Previous preterm delivery | 1/29 3.4% |
| History of infertility | 8/29 27.6% |
| History of Infertility Treatment | |
| IVF | 4/29 13.8% |
| Clomiphene citrate with HCG | 1/29 3.4% |
| Clomiphene citrate with GNRH | 3/29 10.3% |
| Clomiphene | 4/29 13.8% |
Tab. 1. Patient characteristics.
| Presence of symptoms | 18/29 62.1% |
| Gestational age at diagnosis in weeks | Mean ± SD 13.7± 9.3/median (range) 11(34) |
| Unilateral ovarian mass | 25/29 86.2% |
| Bilateral | 4/29 13.8% |
| Hypertrophied ovary+/OHSS | 4/29 13.8% |
| Ovarian torsion | 6/29 20.6% |
| Type of Mass on Scan | |
| Simple(including one paratubal cyst) | 16/29 55.2% |
| Haemorrhagic | 5/29 17.2% |
| Dermoid | 4/29 13.8% |
| Cystic with thick wall | 1/29 3.4% |
| Complex | 3/29 10.3% |
| Ovarian cyst size | |
| ≤ 5 cm | 11/29 37.9% |
| >5 cm | 18/29 62.1% |
| CT scan suggestive of malignancy | 1/29 3.4% |
| MRI | |
| Clear cyst | 2/29 6.8% |
| Dermoid | 3/29 10.3% |
| Complex | 2/29 6.8% |
| Tumour markers elevated (Ca125) | 2/29 6.9% |
Tab. 2. Presentation of adnexal masses.
Clinical presentation on the basis of symptoms and mean gestational age were calculated. Adnexal masses were differentiated with the aid of imaging assessment. Classifications of masses were done according to the ultrasound findings. Computerized Tomography (CT) Scan was used for the suspected malignant case, which was later confirmed by histopathology. Magnetic Resonance Imaging (MRI) was used for the complex masses and it assisted to plan the surgical interventions. Out of the two cases with elevated Ca125 levels, one was confirmed as malignant mass.
The masses were managed either conservatively or surgically according to the severity of the clinical presentation (Tab. 3.). The surgical interventions were done by the laparoscopically or laparotomy. The surgical procedures and approaches were decided after the assessment of various factors including the complications and complexity of the masses upon outweighing the benefits (Tab. 4.).
| Conservative | 15/29 51.72% |
| Antibiotic cover | 17/29 58.6% |
| Spontaneous resolution during pregnancy | 12/29 41.37% |
| Persistence of cyst without symptoms in postpartum period | 3/29 10.34% |
| Antenatal surgery | 10/29 34.48% |
| Ovarian surgery with caesarean delivery | 4/29 13.8% |
| Surgical Approach | |
| Laparotomy including four during caesarean | 7/29 24.1% |
| Laparoscopy | 6/29 20.6% |
| u/s guided trans abdominal cyst aspiration | 1/29 3.4% |
| Surgical Procedure | |
| Ovarian cystectomy | 3/29 10.3% |
| Oopherectomy | 4/29 13.8% |
| cystectomy with salpingectomy | 1/29 3.4% |
| Oopherectomy with salpingectomy | 2/29 6.9% |
| Ovarian detortion | 3/29 10.3% |
| u/s guided transabdominal Cyst aspiration | 1/29 3.4% |
Tab. 3. Management of adnexal masses.
| Miscarriage | 2/29 6.9% |
| Caesarean delivery | 9/29 31% |
| Preterm delivery | 2/29 6.9% |
| IUGR | 2/29 6.9% |
| SGA | 5/29 17.2% |
| Uneventful pregnancy | 9/29 31% |
Tab. 4. Pregnancy outcome.
The histopathology reported ten benign masses, which includes:
• 4 Dermoid masses (13.8%)
• 4 serous cysadenoma (13.8%)
• One haemorrhagic cyst (3.4%)
• One fibrothecoma (3.4%), and
• One confirmed malignancy with rate of (3.4%).
Discussion
The incidence of adnexal masses during pregnancy varies from 0.01% to 10% [1,3,6,11,12]. Our study population rate of adnexal mass was 0.33% which was comparable with previously reported incidence. The study excluded the insignificant adnexal masses like corpus luteal cysts, smaller follicular cysts and also undetected asymptomatic masses that resolved spontaneously. In the present study, we confirmed one malignancy with an incidence of 3.4%. The reported incidence of malignant cases among the adnexal mass in pregnancy varies from 0.05 to 8% [1,3,6,13].
There is no proved correlation between maternal characteristics such as age, BMI, parity and aetiology of adnexal masses during pregnancy. Few studies correlated age and the category of the adnexal masses during pregnancy. Leiserowitz describes the age-related characteristics of the ovarian masses during pregnancy and benign lesions are prevailing [7]. In a study by Soriano et al., the median age of the patients presenting with adnexal masses during pregnancy was 27 to 28 years, which is similar to our findings [5]. Younger patients (mean age 23.47 years) with adnexal masses were noted in a retrospective study by Sunanda et al. [12]. Most of the articles describe the detection of adnexal masses occurring during early pregnancy [1,14]. Our study showed the mean gestational age at diagnosis was 13.7 weeks.
Infertility treatments are not directly correlated to adnexal masses during pregnancy. However, patients undergoing infertility treatment involving ovulation induction with gonadotropins /clomiphene citrate can develop cysts or ovarian hyperstimulation syndrome. In our study, one woman had a history of polycystic ovarian syndrome. OHSS incidence is reported as 3 to 8%. Most OHSS cases resolve spontaneously and surgical intervention is preferred in cases with ovarian torsion or rupture [1,15]. Half of our patients who received infertility treatment also conceived through IVF. Of those eight cases, four had a spontaneous resolution, one case developed an adnexal abscess that was managed conservatively, two cases had ovarian torsion and underwent laparoscopic detortion and one case necessitated surgical removal.
Adnexal masses are usually detected in pregnancy during routine ultrasound scans and are mostly asymptomatic [2,13]. In contrast, more than half of our cases 18/29 (62.1%) presented with symptoms. A few cases were diagnosed incidentally during a caesarean section and the immediate postpartum period. An ultrasound scan is usually used both as an initial diagnostic tool and a supportive appliance to confirm the clinical diagnosis. However, the evaluation of masses by a trained professional is important as analysing the structures around the pregnant uterus is often challenging and requires extensive experience. Ultrasound is also used to stratify masses according to size and other characteristics (e.g., solid components, vascularity, haemorrhagic spots, multi-locations, free pelvic fluid and ascites). These characteristics enable differentiating between benign and malignant masses and also acute emergencies like torsion [1,13,16]. Our ultra-sonogram assessment almost matched the later MRI assessment. A prospective study by Zanetta and review by Ibrahim describe the use of ultrasound in the diagnosis and management of these masses [3,14]. MRI enhances the diagnostic findings in cases of complex masses and to identify metastasis [17]. It is considered safe during pregnancy. Furthermore, MRI helps to select the most suitable management option [1,3,16]. Abdulla et al. emphasize the importance of utilizing MRI to improve the reliability of diagnosis [2].
In cases with a high suspicion of malignancy, checking for tumour markers is justified. Even though reports indicate variation in diagnoses during pregnancy, tumour markers could help in uncertain cases and also for monitoring outcome in selected cases [1,3]. In our study, one haemorrhagic cyst was noted as having a high level of Ca125 and another case was unfortunately confirmed as malignant later. Adnexal mass assessment by generally accepted protocols like RMI (Risk Malignancy Index), ROMA (Risk of Ovarian Malignancy Algorithm), IOTA (International Ovarian Tumour Analysis Tool) not widely used and has restricted value during pregnancy due to variation in tumour markers and inaccurate interpretations [1,16,17].
Pregnant women with ovarian masses must receive adequate counselling to decide on a management plan. The options available are either to observe the mass during pregnancy and act at or after delivery or intervene during pregnancy [18]. Furthermore, surgeries can be performed either via laparoscopic or by laparotomy [3,19]. The final decision is usually based on the clinical symptoms, gestational age and nature of the mass. However, utilizing trained professionals and identifying the most appropriate surgical approach are paramount to achieving a successful outcome [20]. The conservative approach is usually appealing to pregnant women as they fear interventions could terminate the pregnancy. Our study concurs with the study by Oprescu ND, et al for the terms of conservative management approach [21]. Most adnexal masses during pregnancy resolve spontaneously [13,14,22]. We managed 51.7% of the cases conservatively and 12 cases resolved spontaneously, three of which presented mid-trimester. Large masses found in the first-trimester usually require surgical intervention. However, one of our cases was diagnosed incidentally when she was admitted with a potential miscarriage in the first trimester. The mass was an 11 × 9 cm complex cyst. As she was asymptomatic and had low levels of tumour markers Ca125, we decided to observe the mass. She was scheduled for a cystectomy mid-trimester pregnancy. As she had severe thrombocytopenia, the procedure was postponed. Eventually, she underwent surgical intervention during the emergency caesarean performed at 34 weeks due to obstetric indications. Another interesting case was diagnosed early in gestation and was suspected as malignant based on radiological imaging and high Ca125 levels. After its spontaneous rupture, laparoscopy/histopathology confirmed the presence of a haemorrhagic cyst only.
Once the decision is made to intervene, selecting the best approach is crucial [23]. This decision is based on clinical/radiological criteria and the availability of a trained professional [1]. Many authors investigate the risks and benefits of each surgical procedure in terms of length of hospital stay, postoperative complications and safety [3,13]. The Ibrahim group recommended criteria for surgical intervention to include a persistent mass and the mass being at risk of complications like torsion or rupture [3]. Another author determined the individual timing of an intervention given the risk to the mother and foetus [2]. Aderemi reported the incidence of torsion to be 1 to 5 of every 10,000 pregnancies. This rate is higher in OHSS [1]. In our study, six cases presented as acute emergencies with torsion of the cyst including two with hyperstimulated ovaries with a torsion rate of 20.7%. Three cases underwent successful laparoscopic detortion and preservation of the ovaries based on conserved viability and vascularity of the ovary. Ye P, and et al supported our study for the significances of laparoscopic approach [24]. Cyst aspiration is acceptable in selective cases for temporary symptom relief and is associated with fewer complications1. One of our cases requires ultrasound-guided transabdominal aspiration, but unfortunately, the cyst became infected and turned into an abscess. Another case involved a large paratubal cyst (20 x 15 cm). The mass was diagnosed at 23 weeks of gestation. Due to pressure symptoms, she underwent a cystectomy along with salpingectomy through mini-laparotomy and the pregnancy was continued successfully. The cyst is shown in (Fig.1.).
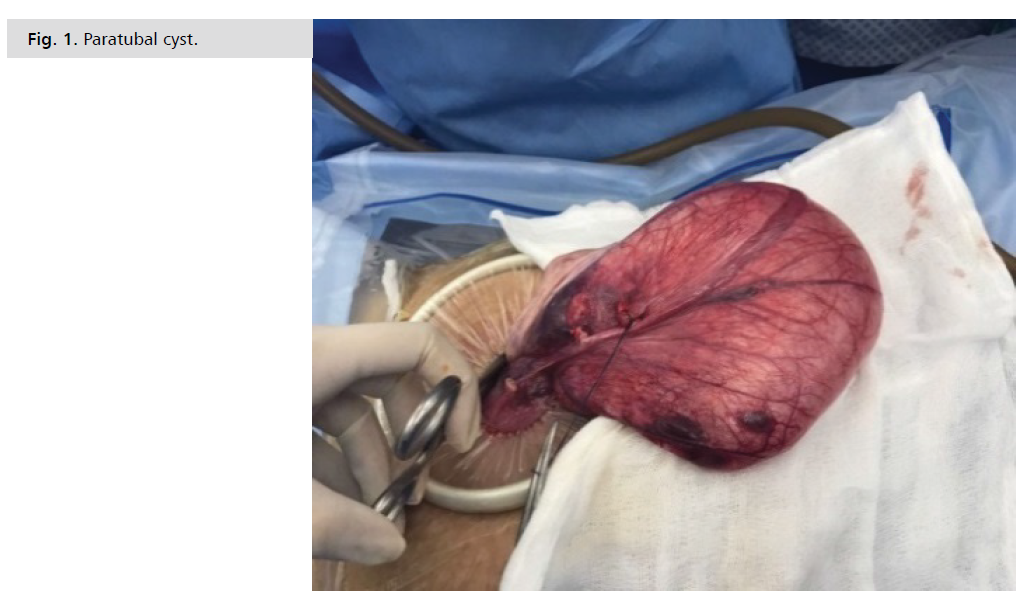
Fig 1. Paratubal cyst.
Another useful approach is performing ovarian surgery during the caesarean section. One of our cases was a 9 x 5 cm clear cyst diagnosed at 14 weeks. The patient was asymptomatic and was observed until her caesarean. The women were counselled about the benefits and risks. Also, the cases diagnosed incidentally during caesarean section were removed and histopathology reports were followed up. Ulker and Baser elaborate on the coincidental diagnosis of adnexal masses during caesarean delivery and their management. These masses require surgical intervention at the time of caesarean delivery so that we can reduce the likelihood of further interventions as well as categorize the characteristics of adnexal masses [25]. Mostly these women experience good outcome [26].
Suspected malignant mass during pregnancy is a challenging case. In malignant masses, well planned primary surgeries during pregnancy followed by restaging after delivery are the mainstay of management [1]. Involving specialized professionals and a systematic approach in the management of these cases has a major impact on outcome [27]. Thankfully, we had only one malignant case in our study. Our patient was diagnosed with a complex adnexal mass at 18 weeks. The mass was multiloculated with solid tissue and very high levels of Ca125. She was counselled about the risks of miscarriage, preterm delivery, Preterm Premature Rupture of Membranes (PPROM), the progression of the tumour to more advance stages and the need for chemotherapy. Given her age, gestational age and future fertility concerns, she had a laparotomy at 26 weeks of gestation and underwent surgical removal of the mass, which was approximately 2 kg, along with right ovary, which was enlarged, septated and had multiple gross cystic lesions (Fig. 2.). Specimens were taken for staging from the omentum, peritoneum, ipsilateral and contralateral sides. Nearly 1.5 L of ascitic fluid was aspirated. Her left ovary and adnexa were grossly normal. She was staged as 1c. The aim was to deliver upon reaching minimum foetal viability. She had PPROM and cord prolapse at 32 weeks and received an emergency caesarean section. The baby weighed 1750 g and was in the Neonatal Intensive Care Unit (NICU) for 20 days, the stay of the baby during this period was uneventful. She had six cycles of chemotherapy and is under the care of an oncologist.
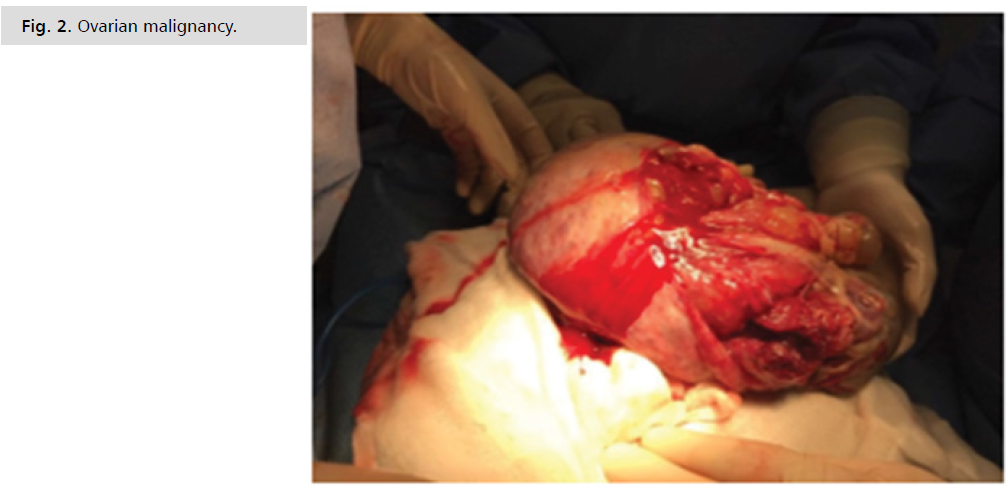
Fig 2. Ovarian malignancy.
A study by Schmeler showed 17 patients had antenatal surgeries out of which 12 were benign and five were malignant [18]. Sunanda highlighted the foetal and maternal considerations during surgical intervention in malignant cases [12]. The timing of mass removal needs to be modified according to the characteristics of the mass and the gestational age. Also, the benefits and risks of surgeries for suspected malignancies in terms of foetal viability should be analysed thoughtfully [12].Our study agreed with the views by D’Ambrosio V, et al for the indications of surgeries of the adnexal masses during pregnancy [28]. Surgery was provided mainly for the malignant cases or complicated adnexal masses during pregnancies.
Many authors stated that the adverse foetus outcomes are by chance occurrences and are not directly related to adnexal masses during pregnancy and surgical interventions [13]. Generally, adnexal masses during pregnancy cause negligible maternal morbidity and mortality. Foetal risks include intrauterine growth restriction, preterm membrane rupture, preterm delivery and intrauterine death [2,5]. Nick described variable miscarriage rates [13]. Zanetta reported that caesarean delivery was needed in 12 out of 78 deliveries [14]. We performed 9 caesareans out of 29 deliveries for obstetric reason. The gestational age at diagnosis and size of the cyst had no direct effect on pregnancy outcome. Two of our cases ended in first-trimester miscarriages despite being treated conservatively. One patient had a 4 cm haemorrhagic cyst and the other a bilateral clear cyst under 5 cm. We had two preterm deliveries; one was confirmed to be malignant at early gestation and required major intervention during the pregnancy. The other was diagnosed in early pregnancy and the cyst was 9 x 11 cm. Her surgery was cancelled due to severe thrombocytopenia. She had PPROM with breech presentation and underwent an emergency caesarean section and cystectomy with oophorectomy, which revealed a mature teratoma. The baby was 3200 g and in need of neonatal unit care for 11 days for preterm-associated comorbidities. Poor pregnancy outcomes like preterm and PPROM are reported by Agarwal [29].
Our histopathology report found dermoid cysts (13.8%), haemorrhagic cysts (3.4%), fibrothecomas (3.4%), serous cystadenomas (13.8%) which categorize the benign masses (34.4%) and malignant masses (3.4%). In a study by Schmeler on 127,177 deliveries, most of the masses are dermoid cysts and benign whereas malignant masses were only 0.0032% of deliveries [18]. Another study reported the masses are dermoid cysts in 37 to 50% of cases and malignancies in 0 to 8.5% of cases, which matched our findings [13].
Conclusion
The surgical management of adnexal masses during pregnancy needs to be thoroughly analysed in terms of clinical presentation, size, gestational age, the complexity of the masses and the complications. Optimized surgical approaches by the specialized professionals have the potential to improve the outcome. Consideration to be given for the viability of the foetus without compromising the maternal outcome.
Author Contribution
All authors share equal effort towards contributions to conception and design, acquisition, analysis and interpretation of data.
Conflicts of Interest
None.
Sponsorship
None.
Ethical Approval
The study was approved by the Ethical Committee, Research Centre in Bahrain Defense Force Hospital.
Acknowledgement
We thank The Royal Bahrain Defense Force Hospital, The Crown Prince Centre for Training and Medical Research.
Learning Point
Specialized professionals should be involved in assessment and management of patients with adnexal masses during pregnancy to categorize the surgical interventions.
References
- Alalade AO, Maraj H. Management of adnexal masses in pregnancy. Obstet Gynecol. 2017;19(4):317-25.
- Hakoun AM, AbouAl-Shaar I, Zaza KJ, et al. Adnexal masses in pregnancy: An updated review. Avicenna J Clin Med. 2017;7(4):153.
- Yakasal AA, Bappa LA. Diagnosis and management of adnexal masses in pregnancy. J Surg Tech Case Rep. 2012;4(2):79-85.
- Leiserowitz GS, Xing G, Cress R, et al. Adnexal masses in pregnancy: how often are they malignant?. Gynecol Oncol. 2006;101(2):315-21.
- Soriano D, Yefet Y, Seidman DS, et al. Laparoscopy versus laparotomy in the management of adnexal masses during pregnancy. Fertil Steril. 1999;71(5):955-60.
- Nazer A, Czuzoj-Shulman N, Oddy L, et al. Incidence of maternal and neonatal outcomes in pregnancies complicated by ovarian masses. Arch Gynecol Obstet. 2015;292(5):1069-74.
- Leiserowitz GS. Managing ovarian masses during pregnancy. Obstet Gynecol Surv. 2006;61(7):463-70.
- Bernhard LM, Klebba PK, Gray DL, et al. Predictors of persistence of adnexal masses in pregnancy. Obstet Gynecol. 1999;93(4):585-9.
- Yen CF, Lin SL, Murk W, et al. Risk analysis of torsion and malignancy for adnexal masses during pregnancy. Fertil Steril. 2009;91(5):1895-902.
- Chen L, Ding J, Hua K. Comparative analysis of laparoscopy versus laparotomy in the management of ovarian cyst during pregnancy. J Obstet Gynaecol Res. 2014;40(3):763-9.
- Aggarwal P, Kehoe S. Ovarian tumours in pregnancy: a literature review. Eur J Obstet Gynecol Reprod Biol. 2011;155(2):119-24.
- Sunanda N, Akhila MV. Ovarian tumours associated with pregnancy: A five year retrospective study in a tertiary care hospital. Int J Reprod Contracept Obstet Gynecol. 2015;4(6):1965-9.
- Nick AM, Schmeler K. Adnexal masses in pregnancy. Perinatology. 2010;2:13-21.
- Zanetta G, Mariani E, Lissoni A, et al. A prospective study of the role of ultrasound in the management of adnexal masses in pregnancy. BJOG: Int J Obstet Gynaecol. 2003;110(6):578-83.
- Royal College of Obstetricians and Gynaecologists.Green-top Guideline 5.The management of ovarian hyperstimulationsyndrome. London: RCOG. 2016.
- Kaijser J, Van Hoorde K, Van Calster B, et al. Diagnosing adnexal tumours before surgery: a critical appraisal of recent evidence. Obstet Gynecol. 2015;17(3):163-71.
- Yacobozzi M, Nguyen D, Rakita D. Adnexal masses in pregnancy. Semin Ultrasound CT MR. 2012;33(1):55-64.
- Schmeler KM, Mayo-Smith WW, Peipert JF, et al. Adnexal masses in pregnancy: surgery compared with observation. Obstet Gynecol. 2005;105(5):1098-103.
- Latika DP. Ovarian mass in pregnancy. Int J Reprod Contracept Obstet Gynecol. 2015 Jun;4(3):915-7.
- Hoover K, Jenkins TR. Evaluation and management of adnexal mass in pregnancy. Am J Obstet Gynecol. 2011;205(2):97-102.
- Oprescu ND, Ionescu CA, Drăgan IO, et al. Adnexal masses in pregnancy: perinatal impact. Rom J Morphol Embryol. 2018;59(1):153-8.
- Bignardi T, Condous G. The management of ovarian pathology in pregnancy. Best Pract Res Clin Obstet Gynaecol. 2009;23(4):539-48.
- de Haan J, Verheecke M, Amant F. Management of ovarian cysts and cancer in pregnancy. Facts Views Vis Obgyn. 2015;7(1):25.
- Ye P, Zhao N, Shu J, et al. Laparoscopy versus open surgery for adnexal masses in pregnancy: a meta-analytic review. Arch Gynecol Obstet. 2019;299(3):625-34.
- Ulker V, Gedikbasi A, Numanoglu C, et al. Incidental adnexal masses at cesarean section and review of the literature. J Obstet Gynaecol Res. 2010;36(3):502-5.
- Baser E, Erkilinc S, Esin S, et al. Adnexal masses encountered during cesarean delivery. Int J Gynaecol Obstet. 2013;123(2):124-6.
- Mancari R, Tomasi-Cont N, Sarno MA, et al. Treatment options for pregnant women with ovarian tumors. Int J Gynecol Cancer. 2014;24(6).
- D’Ambrosio V, Brunelli R, Musacchio L, et al. Adnexal masses in pregnancy: an updated review on diagnosis and treatment. Tumori J. 2021;107(1):12-6.
- Agarwal N, Kriplani A, Bhatla N, et al. Management and outcome of pregnancies complicated with adnexal masses. Arch Gynecol Obstet. 2003;267(3):148-52.
Google Scholar Crossref Pubmed
Google Scholar Crossref Pubmed
Google Scholar Crossref Pubmed
Google Scholar Crossref Pubmed
Google Scholar Crossref Pubmed
Google Scholar Crossref PubMed
Google Scholar Crossref Pubmed
Google Scholar Crossref Pubmed
Google Scholar Crossref Pubmed
Google Scholar Crossref Pubmed
Google Scholar Crossref Pubmed
Google Scholar Crossref Pubmed
Google Scholar Crossref Pubmed
Google Scholar Crossref Pubmed
Google Scholar Crossref Pubmed
Google Scholar Crossref Pubmed
Google Scholar Crossref Pubmed
Google Scholar Crossref Pubmed
Google Scholar Crossref Pubmed
Google Scholar Crossref Pubmed
Author Info
Amala Sunder1*, Basma Darwish1, Abdulla Darwish2, Veena Nagaraj2 and Nawal M. Dayoub32Department of Pathology, Bahrain Defense Force Hospital, Riffa, Bahrain
3Fertility Consultant, ARGC, London, United Kingdom
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.