Research - (2023) Volume 18, Issue 2
A retrospective cross-sectional study evaluation of the success of vaginal birth after cesarean section in patients attended between 2015 and 2019: An experience of a private hospital in the United Arab of Emirates
Dina Yahia Mansour, Heba Alla S. Ashoush and Marwa S. Snosi*Received: 22-Dec-2022, Manuscript No. gpmp-22-84466; Editor assigned: 23-Dec-2022, Pre QC No. P-84466; Reviewed: 18-Jan-2023, QC No. Q-84466; Revised: 29-May-2023, Manuscript No. R-84466; Published: 30-Jun-2023
Abstract
Background: Caesarean section rate has increased markedly worldwide; it reached 72% in some Arab countries as Egypt, in 2021; according to the last governmental statistics, the most common indication is previous CS. Trial of labor after cesarean section is one of the most important strategies to decrease this rise.
Objective: The study aimed to determine the rate of VBAC in a private hospital in UAE and any associated maternal or fetal complications.
Methods: A retrospective cross-sectional study was conducted among all patients admitted to the labor room between 2015 and 2019 for vaginal delivery after one CS, which was uncomplicated. Data were collected from patients’ files, and finally, 672 files were analyzed.
Results: Out of 672 patients, 208 had successful VBAC, which represents 31.0%. Most patients with successful VBACs were in the 25-29 age group (71.28%) with cervical dilatation >4cm and lower head station. Regarding causes of failure, (49.8%) were due to fetal distress, scar tenderness (30%), failure of progress (9.9%), maternal request (5.4%), and the least cause was vaginal bleeding 5.0%. The most prevalent maternal complications recorded were hemodynamic instability (3.4%) in the failed group, and the most prevalent neonatal complications were respiratory distress syndrome (9.1%) in both groups. with one case of neonatal death in each group.
Conclusion: VBAC is a safe procedure, which should be encouraged to decrease the alarming rise in cesarean section rates and its subsequent complications.
Keywords
Vaginal Birth After Cesarean section (VBAC); Cesarean section; Trial of labor
Introduction
The cesarean section rate rises worldwide; in many countries, it exceeded the WHO recommendation, including United Arab of Emirates, considering the ideal cesarean section rate is 10%-15% [1,2].
Cesarean sections should be performed only when indicated to avoid short- and long-term health consequences affecting both mothers and their babies [3]. As it is associated with more blood loss than vaginal delivery, increased risk of urological injuries, postpartum infection, and neonatal respiratory complications, especially if elicited before 39 weeks gestation; in addition, repeated cs increases maternal mortality and morbidity, especially from placenta accrete spectrum leading to cesarean hysterectomy in most of the cases [4].
Vaginal birth after cesarean section (VBAC) has been considered one of the most important strategies in reducing the cesarean section rate. Both RCOG, and ACOG guidelines agreed that women with a history of one lower segment cesarean section with no previous upper segment uterine scar or uterine rupture, who have a clinically adequate pelvis, can safely attempt VBAC, provided that delivery will be conducted at a well-equipped hospital, with available skilled staff and resources in which emergency cs can be done immediately when indicated [5-7].
VBAC Success rates have been reported to be from 60% to 80% after one previous lower-segment cesarean section, with a risk of uterine rupture reported at approximately (0.5%) [8].
There are some Factors associated with increased VBAC success rate, such as maternal age of fewer than 40 years, prior history of vaginal birth, and any indication of previous cesarean section except failure of progress, However, not every woman with a previous cesarean scar is a candidate for VBAC as the trial could likely result in maternal as well as fetal complications [9,10], so careful selection of patients after proper counseling, and strict adherence to the most recent guidelines for managing labor should be the role [11].
The current study aimed to assess the VBAC success rate in a private Hospital in the United Arab of Emirates and to report maternal or neonatal complications.
Methods
This retrospective cross-sectional study was conducted at a Private Hospital In the United Arab of Emirates between 2015 and 2019. The study did not require ethical committee approval as it was a retrospective analytical study.
Inclusion criteria:
All patients admitted for vaginal delivery with previous lower segment cesarean section, which was uncomplicated, with the following criteria:
• Age between 20 and 40 years.
• Time interval more than 1.5 years from previous CS.
• Single viable full-term pregnancy in vertex presentation.
• Estimated fetal weight between 2.5-3.5 kg.
• Reactive cardiotocography (CTG) on admission.
• Spontaneous labor onset.
• Clinically adequate pelvis.
Exclusion criteria:
• Women with previous upper segment cesarean section or hysterotomy scar.
• Any obstetric complications such as fetal malpresentation, placenta previa, or medical disorders like diabetes mellitus or preeclampsia.
• Presence of any signs and symptoms of scar dehiscence or rupture uterus, known uterine fibroid or anomaly.
• Suspected fetal macrosomia (weight more than 4 kg).
• Multifetal pregnancy.
• Parturient women who refused the trial of vaginal birth after caesarean section.
Data collection:
The following data were collected from patients’ medical record files: maternal age, parity, BMI, gestational age based on last menstrual period or early us scans available, patients’ full medical and surgical history, previous CS details as an indication, and previous complications. Patients’ clinical abdominal and per vaginal examination on admission (cervical dilatation, effacement head station,and position), CTG attached on admission (to exclude fetal distress), laboratory investigations that were done before delivery and postpartum as per hospital standard protocols were revised, labor progress on the portogram was assessed as regard duration of both first and second stages of labor if any instrumental delivery was done. Records for patients’ vital signs, fetal cardiac activity during labor, vaginal bleeding, delivery notes, fetal weight, and 5 minutes APGAR score, and any recorded maternal or fetal complications. If failed VBAC: Causes of failure maternal and fetal outcomes were recorded. After excluding non-eligible files, data were collected from 672 files for analysis. Dividing patients into two groups.
Group 1: Successful VBAC group (n=208)
Group 2: Failed VBAC group (n=464)
The primary outcome was to assess the VBAC success rate. Secondary outcomes assessed factors associated with increased VBAC success rate, maternal morbidity or mortality, fetal complications, NICU admission, and neonatal death.
Statistical analysis
Data analysis was done using Statistical Program for Social Science version 20 (SPSS Inc., Chicago, IL, USA). Quantitative variables were described in the form of mean and standard deviation. Qualitative variables were described as numbers and percentages. A Student test was performed to compare parametric quantitative variables between the two groups. Qualitative variables were compared using the chi-square (X2) or Fisher’s exact test when frequencies were below five. The association between two normally distributed variables was assessed using Pearson correlation coefficients. For variables not normally distributed a P value <0.05 was considered significant.
Results
The number of patients admitted to our hospital during the assessment period was 21317; out of them, 20645 were excluded as they were not matching the inclusion criteria. Finally, 672 patient files were analyzed. From the 672 patients documented within the study, 208 (33.1%) patients had successful VBAC, and 464(66.9%) patients were delivered by repeated Caesarean Section. As shown in the flow chart. Cases of rupture uterus were diagnosed intrapartum, and repair of the uterus was done, no reported cases of intrapartum hysterectomy. By analyzing data over the years, as shown in Tab. 1. the number of successful VBACs had nearly doubled, from an initial percentage of 23.2% in 2015 to 42.86% in 2019. Tab. 2. shows that there was a highly statistically significant difference between the two groups as regards maternal age, head station patients admitted in active labor. Tab. 3. shows the comparison between successful and Failed VBACS as regard Maternal and neonatal outcomes with no statistically significant difference between them. Flow chart of studied patients (Fig. 1.).
| Variables | N | % of VBAC | |
|---|---|---|---|
| Time at admission | 2015 | 125 | 18.60% |
| 2016 | 138 | 20.50% | |
| 2017 | 135 | 20.10% | |
| 2018 | 141 | 21.00% | |
| 2019 | 133 | 19.80% | |
| Patients, age (years) | 20-24 years | 56 | 8.30% |
| 25-29 years | 195 | 29.00% | |
| 30-34 years | 277 | 41.20% | |
| 35-40 years | 144 | 21.40% | |
| Head Station | 0 | 195 | 29.00% |
| -1 | 54 | 8.00% | |
| -2 | 181 | 26.90% | |
| -3 | 242 | 36.00% | |
| CX dilatation | <4 cm | 95 | 14.10% |
| >4 cm | 577 | 85.90% | |
| Active Phase Admission(HRS) Mean± SD, Min- | 2.78±0.96 | 1-4 | |
| Second Stage (min.) Mean± SD, Min-Max | 53.5±12.38 | 30-90 | |
| Outcome of Delivery | Successful VBAC | 208 | 31.00% |
| Failed VBAC | 464 | 69.00% | |
| Causes of failed VBAC (n=464) | Fetal distress | 231 | 49.8% |
| Tender scar | 139 | 30.0% | |
| Failure of progress | 46 | 9.9% | |
| Vaginal bleeding | 23 | 5.0% | |
| Maternal request | 25 | 5.4% | |
Tab. 1. Description of all study variables among study participants.
| Variables | Outcome of Delivery | P | Sig | ||||
|---|---|---|---|---|---|---|---|
| Successful VBAC (n=208) |
|||||||
| Failed VBAC (n=464) | |||||||
| N | % | N | % | ||||
| Time at | 2015 | 29 | 23.20% | 96 | 76.80% | 0.009* | HS |
| admission | 2016 | 37 | 26.80% | 101 | 73.20% | ||
| 2017 | 43 | 31.90% | 92 | 68.10% | |||
| 2018 | 42 | 29.80% | 99 | 70.20% | |||
| 2019** | 57 | 42.90% | 76 | 57.10% | |||
| Age (years) | 20-24 | 35 | 62.50% | 21 | 37.50% | 0.001* | HS |
| 25-29 | 139 | 71.30% | 56 | 28.70% | |||
| 30-34 | 26 | 9.40% | 251 | 90.60% | |||
| 35-40 | 8 | 5.60% | 136 | 94.40% | |||
| Head Station | 0 | 160 | 82.10% | 35 | 17.90% | 0.001* | HS |
| -1 | 48 | 88.90% | 6 | 11.10% | |||
| -2 | 0 | 0.00% | 181 | 100.00% | |||
| -3 | 0 | 0.00% | 242 | 100.00% | |||
| CX dilatation | <4 cm | 7 | 7.40% | 88 | 92.60% | 0.001* | HS |
| >4 cm | 201 | 34.80% | 376 | 65.20% | |||
| Active Phase Admission | 2.16 | 0.93 | 3.06 | 0.83 | 0.001** | HS | |
| Second Stage (min.) | 42.84 | 10.01 | 58.28 | 10.17 | 0.001** | HS | |
Tab. 2. Comparison between successful and failed VBACS as regard personal and obstetric characteristics.
| Variables | Outcome of Delivery | P | Sig | Odds ratio (CI)‡ | ||||
|---|---|---|---|---|---|---|---|---|
| Success (n=208) | Failed (n=464) | |||||||
| N | % | N | % | |||||
| Maternal Complication | Rupture Uterus | 0 | 0% | 9 | 1.9% | 0.063** | NS | |
| Bladder Injury | 0 | 0% | 5 | 1.1% | 0.331** | NS | ||
| Scar dehiscence | 3 | 1.4% | 18 | 3.9% | 0.09* | NS | 2.690 (0.751– | |
| Hemodynamic instability | 3 | 1.4% | 20 | 4.3% | 0.059* | NS | 2.989 (0.900– | |
| Sphincter injury | 4 | 1.92% | 0 | 0% | 0.009** | HS | ||
| Neonatal Complication | HIE | 3 | 60.0% | 2 | 40.0% | 0.175** | NS | 0.296 (0.050– |
| RDS | 23 | 11.1% | 38 | 8.2% | 0.232* | NS | 0.71 (0.16–1.23) | |
| TTN | 16 | 7.7% | 20 | 4.3% | 0.072* | NS | 0.54 (0.274–1.06) | |
| Neonatal death | 1 | 0.48% | 1 | 0.2% | 0.524** | NS | 0.448(0.028– | |
Tab. 3. Comparison between successful and failed VBACS as regard Maternal and neonatal outcomes.
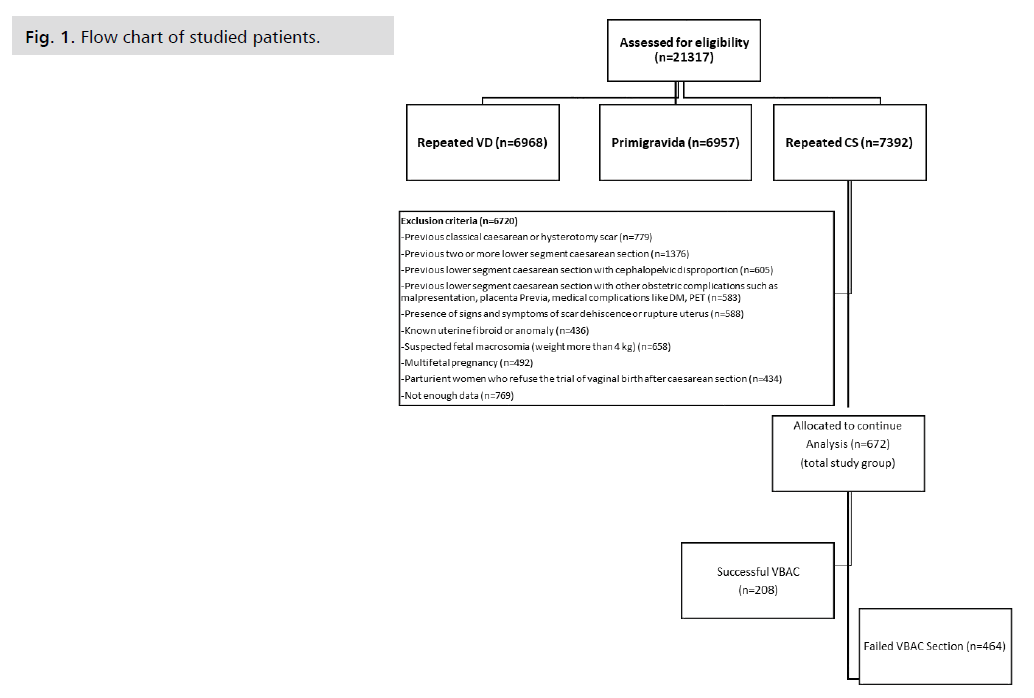
Fig 1. Flow chart of studied patients.
Discussion
CS rate has been alarming in Arab countries; according to the central agency for public mobilization and Statistics (CAPMAS) cesarean section rate raised to 72% in Egypt. in August 2021 after steadily rising from a low of 4.6% in 1992 to 52%in 2014 [12].
Vaginal birth after the cesarean section has been considered a safe and efficient measure in reducing CS rates worldwide [6]. However, success rates are variable between countries. the most commonly reported success rate is between 70%-80% [7].
Interpretation of results of the present study
Our results showed that during the five years study duration, the overall VBAC success rate was only 33.1% and 66.9%of patients delivered by emergency cs. However, it was noticed that the VBAC success rate doubled over the years from an initial percentage of 23.2% in 2015 to 42.86% in 2019, which is still far from the rates of different countries (70-80)%. An analysis of causes of failed VBAC in the present study showed that fetal distress was 49.8% in causes. This is explained by the high flow rate in our hospital and the lack of equipment to document fetal distress as fetal scalp PH apparatus. The second cause was the presence of tender scars in 30.0% (139) of cases which might have raised the fear of obstetricians of scar dehiscence. Among cases of failed VBAC, the results showed that only 18 patients had scar dehiscence. This is explained by the small number of medical staff (residents and nurses). The high medicolegal issues in the United Arab of Emirates may explain the non-insistence of obstetricians to complete the VBAC.
Another cause of decreased VBAC rates in the United Arab of Emirates is the absence of induction in previous CS. The method of induction of VBAC in most countries is the mechanical method (intra-uterine balloon), which is expensive and can be supplied for each patient in governmental hospitals.
Regarding maternal complications in the present study, there was a statistically significant difference between the two groups regarding maternal sphincteric injury, which was higher in the successful VBAC group. Other maternal complications were more in failed VBAC group, such as hemodynamic instability, scar dehiscence, rupture uterus, and bladder injury, and were not statistically significant. No maternal deaths were reported in both study groups. There was also no statistically significant difference between the two groups as regards fetal complications. The most frequent fetal complications reported were hypoxic-ischemic encephalopathy 60%, 40%, respiratory distress syndrome 11.1%,8.2%, and transient tachypnea of newborns 7.7%, 4.3%, in the successful group and failed group, respectively. Two reported cases of fetal death, one in each group. The one in the successful group, the baby delivered flaccid and intubated after CPR, then died in NICU. In the other case, the baby died intrapartum in one case of uterine rupture. These results support the fact is VBAC is a safe procedure.
The comparison of current results with similar studies comparing the rate of the current study in Success of VBAC (33.1%) with developed countries and developing countries, we found that the results of the current study are much lower. In some countries, there is a higher success rate of VBAC, as in Nigeria (73%), India (73%), and Ghana (61%). This reflects the high motivation of the women to deliver vaginal in Ethiopia. However, they are considered low-income countries, and, in turn, patient complaints decrease the medicolegal burden on obstetricians.
As regard high-income countries, the VBAC success rate was reported to be in Japan (91.5%), Australia (83%), United States (71%). and China (80%) which are double the success rates in the present study which is explained by the adequate number of medical staff and assisting equipment [13-20].
In the present study, factors associated with higher success rates with statistically significant differences between the two groups were young maternal age, and women admitted in the active stage of labor (cervical dilatation equal to or more than 4 cm). This was in agreement with a study done by Srinivas SK, et al. who stated that advanced maternal age of fewer than 35 years was more likely associated with the unsuccessful trial of labor while women more than 35 years of age had 39% more risk of experiencing one of the VBAC-related operative complications [21].
Dayoub N and Alani WY evaluated the factors of successful VBAC delivery at Bahrain Defence Force Hospital between 1 January 2014 and 31 January 2015. They found significant successful VBAC in patients with previous vaginal birth, high parity, and presented with cervical dilatation of more than or equal to 4 cm; this was in agreement with the results of the current study [22].
As regard the comparison of maternal and neonatal complications, the present study agrees with the study of Mirteymouri M, et al. regarding the same rates of evaluated maternal and neonatal complications of VBAC. Maternal and neonatal death did not happen during their study, and none of their cases experienced uterine rupture, dystocia, or neonatal complications. This again reflects the safety of VBAC [23].
Study Strengths and Limitations
The study’s strength is that it was conducted over a long period on a relatively large number of patients. Limitations of this study are that it was performed in one hospital, which could cause statistical bias.
Implications in clinical practice: VBAC is a safe procedure and is the only solution to decrease the rates of CS; patients should be counseled for induction by mechanical ways to decrease the financial and medical burden of recurrent CS.
Recommendations for Further Studies
Multicenter studies should be performed to give real figures of TOLAC and VBAC in the United Arab of Emirates private medical sector.
Conclusion
The success rate of VBAC is lower than most of studies, but the factors affecting success and rate of complications are the same as other studies.
Competing Interests
The authors report there are no competing interests to declare.
Funding
This study received no financial support.
Acknowledgement
Not applicable.
Authors Contribution
(A) Study Design · (B) Data Collection · (C) Statistical Analysis · (D) Data Interpretation · (E) Manuscript Preparation · (F) Literature Search · (G) No Fund Collection
References
- Betran AP, Ye J, Moller AB, et al. Trends and projections of caesarean section rates: Global and regional estimates. BMJ Glob Health. 2021;6(6):e005671.
- World Health Organization. WHO statement on caesarean section rates. World Health Organization; 2015.
- World Health Organization. World Health Organization Statement on Caesarean Section Rates. 2016.
- Harrison MS, Pasha O, Saleem S, et al. A prospective study of maternal, fetal and neonatal outcomes in the setting of cesarean section in low‐and middle‐income countries. Acta Obstet Gynecol Scand. 2017;96(4):410-420.
- Misgan E, Gedefaw A, Negash S, et al. Validation of a vaginal birth after cesarean delivery prediction model in teaching hospitals of Addis Ababa University: A cross-sectional study. Biomed Res Int. 2020;2020.
- ACOG Practice Committee. ACOG Practice bulletin no. 115: Vaginal birth after previous cesarean delivery. Obstet Gynecol. 2010;116:450-463.
- Royal College of Obstetricians & Gynaecologists. Birth after previous caesarean birth. Green-top Guideline. 2015 (45).
- Kiwan R, Al Qahtani N. Outcome of vaginal birth after cesarean section: A retrospective comparative analysis of spontaneous vs. induced labor in women with one previous cesarean section. Ann Afr Med. 2018;17(3):145.
- Wu Y, Kataria Y, Wang Z, et al. Factors associated with successful vaginal birth after a cesarean section: A systematic review and meta-analysis. BMC Pregnancy Childbirth. 2019;19(1):1-2.
- Haumonté JB, Raylet M, Sabiani L, et al. Quels facteurs influencent la voie d’accouchement en cas de tentative de voie basse sur utérus cicatriciel?. J Gynecol Obstet Biol Reprod. 2012;41(8):735-752.
- Tanos V, Toney ZA. Uterine scar rupture-Prediction, prevention, diagnosis, and management. Best Pract Res Clin Obstet Gynaecol. 2019;59:115-131.
- Kandil M. The sky rocketing rate of cesarean section in Egypt. Glob Drugs Therap. 2018;3(4):1-3.
- Vikhareva O, Nedopekina E, Kristensen K, et al. Strategies to increase the rate of vaginal deliveries after cesarean without negative impact on outcomes. Midwifery. 2022;106:103247.
- Hassan A. Trial of scar and vaginal birth after caesarean section. J Ayub Med Coll Abbottabad. 2005;17(1).
- Tripathi JB, Doshi HU, Kotdawala PJ. Vaginal birth after one caesarean section: Analysis of indicators of success. J Indian Med Assoc. 2006;104(3):113-115.
- Dayyabu AL, Adamu YI, Patric EO. Vaginal birth after caesarean section (vbac) a two year comparative review of outcome at Abubakar Tafawa Balewa University Teaching Hospital Bauchi Nigeria. Asian J Nat Appl Sci. 2013;2:88-93.
- Seffah JD, Adu-Bonsaffoh K. Vaginal birth after a previous caesarean section: Current trends and outlook in Ghana. J West Afr College Surg. 2014;4(2):1.
- Yokoi A, Ishikawa K, Miyazaki K, et al. Validation of the prediction model for success of vaginal birth after cesarean delivery in Japanese women. Int J Medical Sci. 2012;9(6):488.
- Mooney SS, Hiscock R, Clarke ID, et al. Estimating success of vaginal birth after caesarean section in a regional Australian population: Validation of a prediction model. Aust N Z J Obstet Gynaecol. 2019;59(1):66-70.
- Tang JS, Lo TK. Developing a pilot model to predict successful vaginal birth after caesarean section for Hong Kong Chinese women. Hong Kong J Gynaecol Obstet Midwifery. 2017;17(1).
- Srinivas SK, Stamilio DM, Sammel MD, et al. Vaginal birth after caesarean delivery: Does maternal age affect safety and success?. Paediatr Perinat Epidemiol. 2007;21(2):114-20.
- Alani WY, Dayoub N. Factors influencing successful vaginal birth after cesarean delivery. Bahrain Med Bull. 2017;158(5879):1-5.
- Mirteymouri M, Ayati S, Pourali L, et al. Evaluation of maternal-neonatal outcomes in vaginal birth after cesarean delivery referred to maternity of academic hospitals. J Family Reprod Health. 2016;10(4):206.
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Author Info
Dina Yahia Mansour, Heba Alla S. Ashoush and Marwa S. Snosi*Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.