Research - (2022) Volume 17, Issue 4
Received: 12-Nov-2022, Manuscript No. gpmp-22-79619; Editor assigned: 13-Nov-2022, Pre QC No. P-79619; Reviewed: 28-Nov-2022, QC No. Q-79619; Revised: 05-Dec-2022, Manuscript No. R-79619; Published: 29-Dec-2022
Background: A new technique of uterine incision expansion has been studied in different trials in the past few years in elective CS but cephal-cauded is not studied in emergency CS or CS due to arrest in 2nd stage of labor.
Design: A prospective cross-section comparitive study which was carried in 2 hospitals in Saudi Arabia in the period between January 2022 and June 2022.
Methods: Women underwent CS using cephal-cauded expansion (group A; n=40) and transverse expansion (group B; n=40), with each group having underdone it in a different hospital. We included only patients in the 2nd stage of labor with emergency CS (labor arrest or non-reassuring fetal status).
Measured outcomes were: Occurrence of uterine over-extension, vessel injury, need for additional stitches, and blood loss.
Results: Generally, cephalad- caudal expansion, compared with transverse expansion, had better outcomes, but without statistical significance
Conclusions: In CS at 2nd stage of labor, cephalad-caudal expansion of the uterine incision may be an option.
Cephal-caudad expansion; Traditional transverse expansion; Emergency caesarean section; Unintended extension
World Health Organization encourages that cesarean section rates should be kept between 10% and 15% [1]. In recent decades, the incidence of cesarean delivery has sharply increased, reaching approximately 1,190,000 deliveries in the USA (31.7%of all deliveries), which renders it the most prevalent surgical procedure performed on both elective and emergency indications [2,3].
In metanalysis of Pergialiotiseiet al., 6 RCTs were included in this meta-analysis; these studies included 2818 women who had cesarean deliveries with a low transverse uterine incision that was followed by a blunt expansion of the uterine incision. This recent systematic review and metanalysis published in ACOJ 2021, suggested that cephal-cauded blunt expansion of the uterine incision is superior to transverse expansion in terms of reducing unintended incision extension and uterine vessel injury [4].
The limitation from this metanalysis as mentioned by the authors, that it was based on evidence drawn from the six randomized trials of moderate risk of bias that was mainly attributed to the lack of proper allocation concealment of patients. However, wandered if cephal-cauded technique helps to reduce the transfusion rates as the required sample size was not reached in their meta-analysis to allow more precise information of this outcome. They believed that future research they suggested future studies to include women in second stage of labor especially those with malpresentations and women who underwent emergency CS.
The aim of the current work is to compare cephal-cauded and transverse expansion as regards the incidence of unintended uterine extension as a primary outcome at emergency cesarean section and CS done in second stage of labor.
This prospective cross section comparative trial was conducted in 2 hospitals in Saudi Arabia. One hospital consultant performed the cephal-caudaed group and the second group transverse expansion was performed by another consultant in second hospital (all surgeons were of same level and experience). The ethical committee of both hospitals approved the study and proper informed consents were undertaken from the patients.
Patients were subjected to full history taking (personal, menstrual, detailed obstetric & past surgical history), examination (general, obstetric & local pelvic examination), and routine investigations (C.B.C, Rh, blood grouping and albumin in urine) and ultrasonography to select the patients fulfilling the inclusion criteria which are: age 18 till 40 , term pregnancy either primigravid or multigravida, patients in labor either induced or spontaneous onset , no previous CS or previous uterine scar Patients excluded from start are those with malpresentations as breech , Preterm pregnancy, multiple pregnancies, suspected macrosomia, polyhydraminos or cases with oligohydramnios or fetal growth restriction.
Sample Size Justification
The study included all women fulfilling the inclusion and exclusion criteria who were admitted between January 2022 and June 2022 at the 2 hospitals
The included women were classified into two groups:
Group A; Cephal-cauded blunt expansion (Cephal-cauded Group): including 40 women who had cephal-cauded blunt expansion of the uterine incision all done in one hospital by one consultant.
Group B; Transverse blunt expansion (Transverse Group): including 40 women who had transverse blunt expansion of the uterine incision in the second hospital.
Surgical procedure
Patients were taken for emergency CS only in second stage of labor due to failure of descent or fetal distress in second stage of labor. Skin incision with sharp opening of subcutaneous tissue and Scarpa’s fascia using the scalpel; opening of the rectus sheath by transverse incision then dissection off the recti muscles then opening the peritoneum bluntly - Dissection of the bladder downward, the uterine incision was made as C shape incision about 3 finger breadth to standardize the length of incision and the cavity was entered bluntly with a fingertip.
The intervention at this point:
A. Cephalad-caudad blunt expansion (Cephalad-caudad Group) (n=40): where the C shaped uterine incision was widened by separation of the surgeon forefingers in a cephalad -caudad direction along the midline for also a distance finger width (done in one hospital by 2 consultants at same level and experience).
B. Transversal blunt expansion (Transverse Group) (n=40): where uterine incision was widened by the surgeon thumbs of both hands apart from medial to lateral for a distance about another 4-finger width. Delivery of the fetal head by surgeon hand, spontaneous delivery of the placenta. Closure of uterine incision was done by vicryl sutures in a continuous double layer manner. All intraoperative details were recorded; no of ampoules used in closing the uterine incision, time of closure of uterine incision.
Uterine artery injury was defined as injury of the vessels or that required uterine artery ligation. On the first postoperative day, after 24 hours from operation time, the hemoglobin value was determined and compared with the preoperative HB value to evaluate blood loss.
Statistical analysis
The collected data was revised, coded, tabulated and introduced to a PC using Statistical package for Social Science (SPSS 25.0.1 for windows; SPSS Inc, Chicago, IL, 2001). Shapiro wilk's test was used to evaluate normal distribution of quantitative continuous data. Quantitative non parametric variables are expressed as mean and SD. Qualitative variables are expressed as frequencies and percent. Student t test was used to compare a quantitative variable between two study groups for parametric data & Mann-Whitney U test will be used to compare between the two groups for non-parametric data. Chi square and Fisher’s exact test were used to examine the relationship between categorical variables. A p-value <0.05 was considered statistically significant.
A total of 88 pregnant women were enrolled to the study, 8 cases were excluded from the enrollment as follow 5 of them refused to continue to participate, 3 cases excluded as they left for other hospitals before taking the necessary data (Fig. 1.).
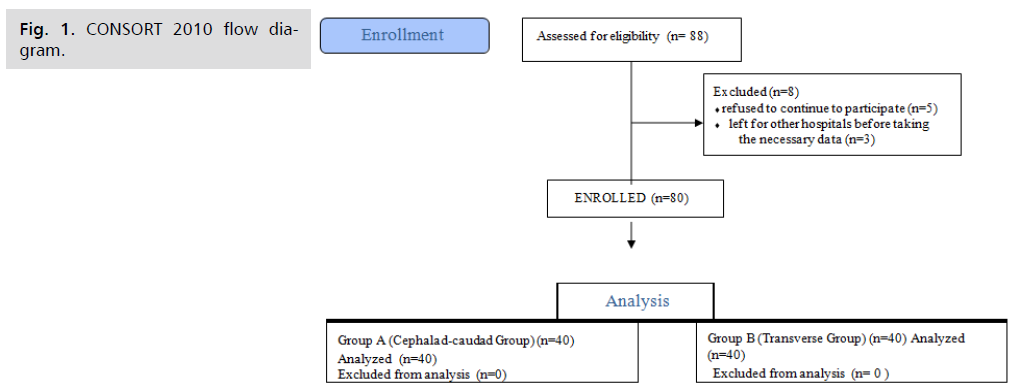
Fig 1. CONSORT 2010 flow diagram.
Finally, eighty pregnant women were classified into two groups; 40 women in each group in one hospital: Group A: cephal-cauded group in first hospital and Group B: Transverse group in second hospital. As shown in (Tab. 1.). No statistical significance difference was found between 2 groups as regarding age, BMI, G.A at birth or fetal weight.
| Variables | Group A [cephal cauded blunt expansion] (N=40) |
Group B [Transverse blunt expansion] (n=40) |
p-value |
|---|---|---|---|
| Age (Years ) | |||
| Range | 18 – 38 | 18 – 38 | 0.261 |
| Median (IQR) | 31 (24 – 35) | 29 ( 23 – 33) | |
| Gestation at Delivery (weeks) | |||
| Range | 38 -41 | 38 – 41 | 0.317 |
| Median (IQR) | 39.4 (38.3 – 40.5) | 39.6 (38.5 – 40.3) | |
Tab. 1. The demographic data of 2 groups.
In the current study there was no statistically significant difference between the 2 groups as regards uterine extension (Tab. 2.). Also, there was no statistically significant difference between two groups in regards to occurrence of uterine vessel injury. There was no significant difference between two groups as regards the need of blood transfusion, pre-operative Hb value and post-operative value of Hb level.
| Adverse outcomes | Group A [cephal cauded blunt expansion] (N=40) |
Group B [Transverse blunt expansion] (n=40) |
P-value |
|---|---|---|---|
| Unintended uterine extension Nil | 38 (95.0%) | 37 (92.5%) | 0.646¶ |
| Lateral extension | 2 (5.0%) | 3 (7.5%) | 0.646¶ |
| Cervical laceration | 1 (2.5%) | 2 (5.0%) | 0.559¶ |
| Uterine vessel injury | 1 (2.5%) | 2 (5.0%) | 0.559¶ |
| Blood transfusion | 1 (2.5%) | 2 (5.0%) | 0.559¶ |
| Pre-operative Hb | 11.13±0.78 | 11.31±0.79 | 0.308 # |
| Post-operative Hb | 10.88±0.76 | 10.77±0.75 | 0.517 # |
Tab. 2. The comparison between 2 groups as regard the study outcomes.
Interpretation of our results and their comparison to similar studies
This study aimed to compare cephal-cauded and transverse blunt expansion of uterine incision in emergency CS that emerges from urgent indications of second stage of labor either failure of descent or fetal distress and this was the recommendation of last metanalysis and review article of Pergialiotiseiet et al. that was published in AJOG [4].
The results of the present study showed that there is decrease in occurrence of lateral extension, cervical extension and uterine vessel injury but they did not reach statistically significant difference between two groups. There was no difference between the 2 groups in need of blood transfusion neither in preoperative or post-operative HB.
The results of the metanalysis of Pergialiotiseiet al. were summarized as follow; Cephalad- caudad blunt expansion was associated with a lower prevalence of unintended incision extension (relative risk, 0.62; 95% confidence interval, 0.45e0.86) and uterine vessel injury (relative risk, 0.55; 95% confidence interval 0.41e0.73). However, these complications were not accompanied by the increased need for additional suture placement (relative risk, 0.62; 95% confidence interval, 0.31e4.12) or transfusion rates (relative risk, 0.75; 95% confidence interval, 0.28e2.03). Similarly, the intraoperative duration was comparable with cases treated with transverse blunt expansion (95% confidence interval 2.12 to 1.21) and the risk of intentional incision extension in the form of an inverted T (relative risk, 0.38; 95% confidence interval, 0.09e1.52). Trial sequential analysis revealed that the required sample size was reached in the unintended incision extension and uterine vessel injury outcomes.
This trial was done on groups of urgent cases, the consultant in charge was the one who is performing the urgent CS aided by the senior registrar where he is experienced enough to do least complications.
There was no statistically significant difference between 2 groups as regard uterine expansion or injury of uterine vessel. This is agreement with study of Mahawerawat and Jeerasap [5] and that of Ozcan et al., [6] where they stated that there was no significant difference between same groups as regard the incidence of uterine extension, although in study of Mahawerawat and Jeerasap and Cromi et al., they stated that blunt transverse expansion is associated with significantly higher injury of uterine vessels compared to cephal-cauded group [5,7] .
In this study, we found that there is no significant difference between 2 groups the need for intra- operative blood transfusion. This is agreement with other RCTs as stated in meta-analysis of Pergialiotiseiet al., [4].
As for comparing the preoperative hemoglobin level between the 2 groups, no statistically significant difference between both groups (P=0.980), this was also applied for postoperative results with no statistically significant difference (P=0.272), this can be attributed to good experience of consultants performing the caesarean sections in the study.
The strength of the current study is that it is the first study to evaluate the cephal-cauded expansion in emergency CS (all studies evaluated it in elective CS). Weak points or limitations of this study are the relative small number of patients and lack of randomization.
As regard clinical practice, we recommend teaching this technique to junior obstetricians as well as traditional technique
Further studies are needed to be randomized and on larger scale of patients
Cephal-caudad technique has lower complication rate than transverse expansion technique but not reaching level of statistical significance.
Study approved by Ethical Committee of 2 hospitals.
Non-applicable.
The datasets used and/or analysed during the current study are available from the corresponding author on reasonable request.
The authors report there are no competing interests to declare.
This study received no financial support.
(A) Study Design · (B) Data Collection . (C) Statistical Analysis · (D) Data Interpretation · (E) Manuscript Preparation · (F) Literature Search · (G) No Fund Collection
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Google Scholar, Crossref, Indexed at
Copyright:This is an open access article distributed under the terms of the Creative Commons Attribution License, which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly cited.